Abstract
Several experimental studies implicate uric acid in renal injury and fibrosis. The objective of this study was to examine the association between uric acid level and allograft fibrosis after kidney transplantation. 241 adult patients who underwent kidney transplantation between 2003 and 2014 were divided into three groups according to the sex specific tertiles of mean uric acid level within the first post-transplant year. The renal biopsies performed during 1 to 5 post-transplant year were analyzed to compare the degree of interstitial fibrosis and tubular atrophy (IF/TA). Mean interval between kidney transplantation and biopsy was similar between groups (23.7 ± 15.3 vs. 30.0 ± 18.6 vs. 27.5 ± 18.5 months, P = 0.072). The higher tertile uric acid level was, the more advanced grade of IF/TA was shown (P = 0.001). Multivariate analysis identified uric acid tertile was independent risk factor for severe IF/TA (odds ratio [95% confidence interval] was 3.16 [1.13–8.82] for tertile 2 and 3.70 [1.25–10.93] for tertile 3, versus tertile 1, respectively). Other independent factors were estimated glomerular filtration rate at 1year post-transplant (0.80 [CI 0.65–0.98]) and biopsy-proven rejection (2.34 [1.05–5.21]). Graft survival over 10 years was significantly lower in tertile 3 (P = 0.041). The results showed that higher uric acid level after kidney transplantation was associated with more severe IF/TA.
Similar content being viewed by others
Introduction
Outcomes after kidney transplantation (KT) have improved over the years, but the proportion of long-term graft failures remains high1,2. Hyperuricemia has been reported as one of the modifiable factors predictive of long-term allograft outcomes3,4,5,6,7,8, although several studies have failed to identify uric acid as an independent risk factor for graft loss9,10,11. These conflicting findings are difficult to reconcile because uric acid is mainly excreted via the kidney, so graft function will affect uric acid levels12, and most previous studies focused on estimated glomerular filtration rate (eGFR) or loss of graft as an endpoint.
Reported mechanisms for renal injury from hyperuricemia include inhibition of endothelial nitric oxide13 and activation of the renin angiotensin system14, inducing vasoconstriction15, as well as vascular smooth muscle cell proliferation16. These changes lead to progressive renal fibrosis17,18, which is a common histologic finding of failing grafts19. In the Banff criteria, allograft fibrosis is defined as interstitial fibrosis and tubular atrophy (IF/TA) and graded according to the extent of the affected area20. IF/TA is associated with progression of graft dysfunction and graft failure, regardless of the underlying pathologic diagnosis21,22,23. Various causes of IF/TA are well described in literature, including rejection, hypertension, calcineurin inhibitor (CNI) toxicity, infections, and other donor or transplant factors24,25,26.
Despite the aforementioned experimental evidence, no study has heretofore investigated the pathologic changes occurring with hyperuricemia after KT, and the association between uric acid and allograft fibrosis has not yet been established in the clinical setting. In this study, our aim was to examine the association between uric acid level and allograft fibrosis after kidney transplantation.
Results
Baseline characteristics
Each group of the sex specific uric acid tertile included 80 (tertile 1), 81 (tertile 2) and 80 patients (tertil 3). Changes in uric acid level over time during the first post-transplant year were demonstrated in Fig. 1. Males showed higher mean uric acid values than females for each tertile. Baseline characteristics of three groups are demonstrated in Table 1. The intervals between KT and biopsy were similar (23.7 ± 15.3 vs. 30.0 ± 18.6 vs. 27.5 ± 18.5 months, respectively; P = 0.072), as were the recipient’s sex, donor’s sex, retransplantation, tacrolimus use, blood pressure at 1 year, use of angiotensin converting enzyme inhibitor, use of uric acid lowering agent. However, recipient age, the body mass index, the proportions of deceased donors, donor’s age, pretransplant diabetes, duration of pretransplant dialysis and delayed graft function were significantly different between groups. The higher tertile of uric acid was, the lower eGFR was at 1 year post-transplant, representing an inverse relationship between uric acid levels and allograft function11,27. Biopsy-proven rejection was not significantly different but numerically higher in tertile 2 and tertile 3 than tertile 1 (46.3% vs. 56.8% vs. 65.0%, P = 0.057). Incidences of each diagnosis of biopsy were similar including CNI toxicity and polyoma virus nephropathy.
Banff pathologic score
Figure. 2 shows comparisons for average of each pathologic (Banff) score. The ci and ct scores were significantly different between the groups (0.4 vs. 0.6 vs. 0.9, P < 0.001 and 0.8 vs. 0.9 vs. 1.2, P = 0.002, respectively), and cg score was also different (0.02 vs. 0.08 vs. 0.35, P = 0.001). In the post hoc analysis, those 3 chronic scores were significantly higher only in tertile 3 than other two groups (P < 0.001 and 0.010 for ci; P = 0.003 and 0.010 for ct; P = 0.001 and 0.009 for cg, vs. tertile 1 and tertile 2, respectively).
Comparison of mean values of Banff scores between uric acid tertiles. *P < 0.05 by one way Analysis of Variance. ah, arteriolar hyalinosis; cg, glomerular basement membrane double contour; ci, interstitial fibrosis; ct, tubular atrophy; cv, vascular fibrous intimal thickening; g, glomerulitis; HighUA, high mean uric acid level; i, interstitial inflammation; ptc, peritubular capillaritis; t, tubulitis; v, intimal arteritis.
Grade of interstitial fibrosis and tubular atrophy
We graded IF/TA from 0 to 3 according to the higher value of the ci and ct scores. There was a significant ordered relationship between the grade of IF/TA and uric acid level (P = 0.001) (Table 2). Overall severe IF/TA (ci ≥2 or ct ≥2) was 18.3% (n = 44). The higher uric acid tertile was, the more frequent severe IF/TA developed (8.8% [n = 7] vs. 19.8% [n = 16] vs. 26.3% [n = 21], P = 0.015). Although male patients had higher uric acid level than female, there was no difference in the severity of IF/TA between both sexes.
Risk assessment for severe interstitial fibrosis and tubular atrophy
Univariate and multivariate analyses showed higher uric acid level was an independent risk factor for severe IF/TA (Table 3). Adjusted odds ratio (OR) of uric acid tertile 2 versus tertile 1 was 2.16 (95% confidence interval [CI] 1.13–8.82, P = 0.028) and that of tertile 3 versus tertile 1 was 3.70 (95% CI 1.25–10.93). Other independent determinants for severe IF/TA were eGFR at 1year post-transplant (per increase of 10 ml/min) (OR 0.8, 95% CI 0.65–0.98) and biopsy-proven rejection (OR 2.34, 95% CI 1.05–5.21). When considered as a continuous variable (per increase of 1 mg/dL), uric acid was still independent risk factor for severe IF/TA (OR 1.42, 95% CI 1.07–1.88).
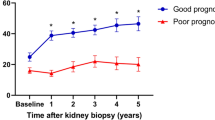
Graft survival
The Kaplan-Meier survival curves showed that death censored graft survival over 10 years was significantly different between three groups (P = 0.041) (Fig. 3). In the post hoc analysis, only tertile 3 had significantly lower survival than tertile 1 (P = 0.036) or tertile 2 (P = 0.041).
Discussion
By comparing Banff pathologic scores from renal biopsies, we demonstrated that higher uric acid was associated with more severe fibrosis in transplanted kidneys. Several experimental studies have shown evidence implicating uric acid in the progression of fibrosis28. Moreover, a recent study hypothesized molecular mechanism of renal injury from soluble uric acid by upregulation of NALP3 inflammasome29 which has been suggested as an endogenous pathway of tissue injury in other organs such as lung30 as well as gout31,32. However, it has been debated whether hyperuricemia exerts a causal effect on the deterioration of renal allografts and native kidneys with chronic disease.
Because serum uric acid and renal function bidirectionally interact with each other, the resultant decline in eGFR could mask the effect of uric acid itself, thus necessitating a longitudinal approach examining time-varying eGFR and uric acid levels. In a retrospective analysis, Kim et al.10 concluded that uric acid was not an independent risk factor for renal allograft loss. However, another large cohort study, using a similar analytical method but a longer follow-up period, showed that uric acid was a risk factor7. Additionally, Tsai et al.33 reported that higher uric acid levels were independently associated with end-stage renal disease and all-cause mortality in patients with chronic kidney disease (CKD) based on the concept of trajectories of uric acid and corresponding eGFRs. Even in the Korean population, where the prevalence of gout is low as 0.4%34, there was a report that higher serum uric acid was associated with increased risk of CKD35. Demonstration of the relationship between uric acid and graft loss or progression of CKD requires long-term follow-up. Therefore, we hypothesized that estimating the differences in chronic renal histologic injuries would help distinguish the true effects of uric acid.
Based on analysis of surveillance biopsies, Stegall et al.36 demonstrated that the majority of renal allografts functioning over 10 years contained chronic injury. They also alluded to the necessity for intensive management of metabolic factors. Another study reported that rejection or the underlying presence of donor-specific antibody (DSA) might be major determinants of fibrosis25. However, treatment benefits after subclinical rejection have so far been restricted to low-risk recipients and have not yet been established in cases of long-term graft survival26, indicating that immunologic causes are not the only factors deserving attention. From this perspective, uric acid could be one of the primary concerns in preventing allograft fibrosis.
Few studies have described the relationship between uric acid and allograft fibrosis. Alkalin et al. reported that hyperuricemia was associated with chronic allograft nephropathy (CAN)37, but that terminology is now outdated and, more specifically, it includes rejection and nonspecific tubulointerstitial fibrosis. Furthermore, hyperuricemia was an independent risk factor for pooled outcomes including death, graft loss, and CAN, but not for CAN alone. More recently, Hart et al.38 demonstrated that hyperuricemia was a risk factor for doubling of the interstitium or end– stage renal disease from IF/TA after KT in a post hoc analysis of a prospective study. However, this study involved a small study population and the multivariate analysis endpoint was intermixed with graft losses from all other causes. Therefore, it was not clear whether hyperuricemia independently increased the risk of IF/TA. Additionally, neither of those two studies compared pathologic scores or considered the underlying pathologic diagnoses. Our results provided more definitive information about the relationship between uric acid level and allograft fibrosis by analyzing pathologic scores as endpoints, especially in the presence of known risk factors such as corresponding renal function and rejection.
In a Korean population study, they showed early post-transplant hyperuricemia was an independent risk factor for allograft loss7. In contrast, we divided KT patients according to sex specific tertiles of serum uric acid and showed an ordered relationship between uric acid level and IF/TA; even tertile 1 showed less severe IF/TA than tertile 2 of which uric acid level was conventionally normal. This result could provide not only a pathologic evidence to support previous studies about uric acid and allograft outcome4,5,7,8 but also an inspiration for the future study on lowering uric acid below the normal level to reduce allograft fibrosis.
In a recent review, Vanhove et al. summarized several therapeutic approaches to reducing the progression of allograft fibrosis after KT, such as CNI-sparing immunosuppression, reduction of renin-angiotensin-aldosterone system activation, appropriate management of subclinical rejection, and direct intervention for fibrogenic molecules26. No interventional study has examined the effects of hyperuricemia treatment on renal fibrosis, but many studies have examined the effects of uric acid-lowering agents on eGFR decline in patients with CKD39. These include a well-designed randomized controlled trial using febuxostat, which is a newly developed xanthine oxidase inhibitor40. In the transplantation field, only a few retrospective, small-volume studies have evaluated the effects of lowering uric acid levels on renal allograft outcome41,42,43. The extent to which hyperuricemia contributes to fibrogenesis of an allograft has not been fully established, especially in the presence of immunologic challenges; however, our study shows that lowering uric acid levels could be an antifibrotic option.
Our study has limitations. As reported in a recent large cohort study, circulating DSA is one of the main contributors to allograft fibrosis25, but it was not assessed in this study because laboratory detection of DSA has been available in our institution since only 2011. Also, because renal biopsies are not standard parts of the post-transplant protocols in our institution, the biopsies included in this study were performed only when deemed indicated by the clinical care team. So, we could not show the changes over time in pathologic scores representing graft fibrosis. A study with routine serial biopsies is necessary to provide more information about the effect of higher uric acid on fibrosis progression.
Despite these limitations, our study demonstrated that higher uric acid level was an independent risk factor for severe IF/TA after kidney transplantation, even in the presence of corresponding renal allograft function and rejection. The results would be not only a good help for the clinical decision about lowering serum uric acid after kidney transplantation but also inspiration for the future research on the allograft fibrosis and long-term outcome.
Methods
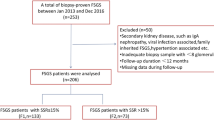
Materials
We conducted a retrospective analysis of prospectively collected data from 296 patients who underwent KT from January 2003 to December 2014 and received renal biopsy during 1 to 5 post-transplant year. The exclusion criteria were as follows: (1) age <18 years at the time of KT, (2) multi-organ transplantation, (3) ABO-incompatible KTs, (4) crossmatch-positive KTs, and (5) insufficient uric acid data (Fig. 4). Finally, 241 patients were analyzed in this study. The biopsies were performed in our study population solely when clinically indicated, such as for increases in serum creatinine or increases in proteinuria. Biopsies performed at the time of surgery were not considered.
Data collection
We obtained serum uric acid levels at 1, 3, 6, 9, and 12 month post-transplant. Patients were divided into three groups according to the sex specific tertiles of their mean uric acid level within the first year. Characteristics of the recipients and donors were also collected from the database.
Pathologic review
All biopsies performed between 1 and 5 year post-transplant were examined by experienced renal pathologists (HJJ, BJL) and scored for glomerulitis (g), interstitial inflammation (i), tubulitis (t), intimal arteritis (v), peritubular capillaritis (ptc), glomerular basement membrane double contour (cg), interstitial fibrosis (ci), tubular atrophy (ct), vascular fibrous intimal thickening (cv), and arteriolar hyalinosis (ah)44. In case of multiple results of biopsy during study period, highest value of each score were recorded. Interstitial fibrosis and tubular atrophy are known to consistently occur together45, so IF/TA was graded according to the higher of the ci score or ct score.
We reviewed the pathology reports diagnosed by criteria before the 2007 Banff meeting report46 so that rejection diagnosis could be determined using the 2007 diagnostic criteria. Other pathologic diagnoses were confirmed in each biopsy, including CNI toxicity, acute tubular injury, polyomavirus nephropathy, diabetic nephropathy, IgA nephropathy, focal segmental glomerulosclerosis, and immune complex-mediated glomerulonephritis other than IgA nephropathy.
Study endpoints
Our primary endpoint was incidence of severe IF/TA (ci ≥ 2 or ct ≥ 2)25. We also investigated the difference in death censored graft survival between groups.
Statistical analysis
Data are shown as mean ± standard deviation for continuous variables and number (frequency) for categorical variables. The one-way Analysis of Variance and chi square test were used when appropriate. To examine ordered-relationship between uric acid tertile and degree of IF/TA, the Mantel-Haenszel chi square test was performed. Logistic regression was utilized in the univariate and multivariate analyses to determine whether uric acids levels independently affected allograft fibrosis. Considering the sizes of the study populations, only covariates with a P value < 0.05 in the univariate analysis and known risk factors of allograft fibrosis in the literature were entered into the multivariate analysis. Univariate and multivariate results were reported as odds ratios (ORs) with 95% confidence intervals (CIs). Kaplan-Meier survival curves were compared using the log rank test. All analyses were performed using SPSS software (version 23.0; SPSS, Inc., Chicago, IL, USA) and P values < 0.05 were considered statistically significant.
Ethic statement
The study was conducted according to the principles of the Declaration of Helsinki and approved by the independent Institutional Review Board of Yonsei University College of Medicine (IRB No.: 4-2017-1154).
References
Meier-Kriesche, H.-U., Schold, J. D., Srinivas, T. R. & Kaplan, B. Lack of Improvement in Renal Allograft Survival Despite a Marked Decrease in Acute Rejection Rates Over the Most Recent Era. American Journal of Transplantation 4, 378–383, https://doi.org/10.1111/j.1600-6143.2004.00332.x (2004).
Hart, A. et al. OPTN/SRTR 2015 Annual Data Report: Kidney. Am J Transplant 17(Suppl 1), 21–116, https://doi.org/10.1111/ajt.14124 (2017).
Min, S. I. et al. Moderate-to-severe early-onset hyperuricaemia: a prognostic marker of long-term kidney transplant outcome. Nephrol Dial Transplant 24, 2584–2590, https://doi.org/10.1093/ndt/gfp192 (2009).
Haririan, A. et al. The independent association between serum uric acid and graft outcomes after kidney transplantation. Transplantation 89, 573–579, https://doi.org/10.1097/TP.0b013e3181c73c18 (2010).
Haririan, A. et al. Association of serum uric acid with graft survival after kidney transplantation: a time-varying analysis. Am J Transplant 11, 1943–1950, https://doi.org/10.1111/j.1600-6143.2011.03613.x (2011).
Oh, I. H., Kim, J. E., Lee, C. H., Kim, G. H. & Park, J. S. A J-Shaped Association Between Serum Uric Acid Level and Allograft Outcomes After Living Donor Kidney Transplantation. Artif Organs 40, 136–143, https://doi.org/10.1111/aor.12519 (2016).
Han, M. et al. Early onset hyperuricemia is a prognostic marker for kidney graft failure: Propensity score matching analysis in a Korean multicenter cohort. PLoS One 12, e0176786, https://doi.org/10.1371/journal.pone.0176786 (2017).
Zhang, K. et al. Serum Uric Acid and Renal Transplantation Outcomes: At Least 3-Year Post-transplant Retrospective Multivariate Analysis. PLoS One 10, e0133834, https://doi.org/10.1371/journal.pone.0133834 (2015).
Meier-Kriesche, H. U., Schold, J. D., Vanrenterghem, Y., Halloran, P. F. & Ekberg, H. Uric acid levels have no significant effect on renal function in adult renal transplant recipients: evidence from the symphony study. Clin J Am Soc Nephrol 4, 1655–1660, https://doi.org/10.2215/CJN.02700409 (2009).
Kim, E. D., Famure, O., Li, Y. & Kim, S. J. Uric acid and the risk of graft failure in kidney transplant recipients: a re-assessment. Am J Transplant 15, 482–488, https://doi.org/10.1111/ajt.13000 (2015).
Kalil, R. S. et al. Impact of Hyperuricemia on Long-term Outcomes of Kidney Transplantation: Analysis of the FAVORIT Study. Am J Kidney Dis 70, 762–769, https://doi.org/10.1053/j.ajkd.2017.06.013 (2017).
Marangella, M. Uric acid elimination in the urine. Pathophysiological implications. Contrib Nephrol 147, 132–148, https://doi.org/10.1159/000082551 (2005).
Khosla, U. M. et al. Hyperuricemia induces endothelial dysfunction. Kidney Int 67, 1739–1742, https://doi.org/10.1111/j.1523-1755.2005.00273.x (2005).
Ruggiero, C. et al. Uric acid and inflammatory markers. Eur Heart J 27, 1174–1181, https://doi.org/10.1093/eurheartj/ehi879 (2006).
Sanchez-Lozada, L. G. et al. Mild hyperuricemia induces vasoconstriction and maintains glomerular hypertension in normal and remnant kidney rats. Kidney Int 67, 237–247, https://doi.org/10.1111/j.1523-1755.2005.00074.x (2005).
Kang, D. H. et al. Uric acid causes vascular smooth muscle cell proliferation by entering cells via a functional urate transporter. Am J Nephrol 25, 425–433, https://doi.org/10.1159/000087713 (2005).
Kang, D. H. A Role for Uric Acid in the Progression of Renal Disease. Journal of the American Society of Nephrology 13, 2888–2897, https://doi.org/10.1097/01.asn.0000034910.58454.fd (2002).
Feig, D. I., Kang, D. H. & Johnson, R. J. Uric acid and cardiovascular risk. N Engl J Med 359, 1811–1821, https://doi.org/10.1056/NEJMra0800885 (2008).
Nankivell, B. J. et al. The natural history of chronic allograft nephropathy. N Engl J Med 349, 2326–2333, https://doi.org/10.1056/NEJMoa020009 (2003).
Loupy, A. et al. The Banff 2015 Kidney Meeting Report: Current Challenges in Rejection Classification and Prospects for Adopting Molecular Pathology. Am J Transplant 17, 28–41, https://doi.org/10.1111/ajt.14107 (2017).
Cosio, F. G. et al. Kidney allograft fibrosis and atrophy early after living donor transplantation. Am J Transplant 5, 1130–1136, https://doi.org/10.1111/j.1600-6143.2005.00811.x (2005).
John, R. et al. Determinants of long-term graft outcome in transplant glomerulopathy. Transplantation 90, 757–764, https://doi.org/10.1097/TP.0b013e3181efcffd (2010).
Naesens, M. et al. The histology of kidney transplant failure: a long-term follow-up study. Transplantation 98, 427–435, https://doi.org/10.1097/TP.0000000000000183 (2014).
Solez, K. et al. Banff ‘05 Meeting Report: differential diagnosis of chronic allograft injury and elimination of chronic allograft nephropathy (‘CAN’). Am J Transplant 7, 518–526, https://doi.org/10.1111/j.1600-6143.2006.01688.x (2007).
Gosset, C. et al. Circulating donor-specific anti-HLA antibodies are a major factor in premature and accelerated allograft fibrosis. Kidney Int 92, 729–742, https://doi.org/10.1016/j.kint.2017.03.033 (2017).
Vanhove, T., Goldschmeding, R. & Kuypers, D. Kidney Fibrosis: Origins and Interventions. Transplantation 101, 713–726, https://doi.org/10.1097/TP.0000000000001608 (2017).
Abbott, K. C. et al. New-onset gout after kidney transplantation: incidence, risk factors and implications. Transplantation 80, 1383–1391 (2005).
Kim, I. Y., Lee, D. W., Lee, S. B. & Kwak, I. S. The role of uric acid in kidney fibrosis: experimental evidences for the causal relationship. Biomed Res Int 2014, 638732, https://doi.org/10.1155/2014/638732 (2014).
Xiao, J. et al. Soluble uric acid increases NALP3 inflammasome and interleukin-1beta expression in human primary renal proximal tubule epithelial cells through the Toll-like receptor 4-mediated pathway. Int J Mol Med 35, 1347–1354, https://doi.org/10.3892/ijmm.2015.2148 (2015).
Gasse, P. et al. Uric acid is a danger signal activating NALP3 inflammasome in lung injury inflammation and fibrosis. Am J Respir Crit Care Med 179, 903–913, https://doi.org/10.1164/rccm.200808-1274OC (2009).
Martinon, F., Petrilli, V., Mayor, A., Tardivel, A. & Tschopp, J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature 440, 237–241, https://doi.org/10.1038/nature04516 (2006).
Liu-Bryan, R. Intracellular innate immunity in gouty arthritis: role of NALP3 inflammasome. Immunol Cell Biol 88, 20–23, https://doi.org/10.1038/icb.2009.93 (2010).
Tsai, C. W. et al. Uric acid predicts adverse outcomes in chronic kidney disease: a novel insight from trajectory analyses. Nephrol Dial Transplant, https://doi.org/10.1093/ndt/gfx297 (2017).
Kuo, C. F., Grainge, M. J., Zhang, W. & Doherty, M. Global epidemiology of gout: prevalence, incidence and risk factors. Nat Rev Rheumatol 11, 649–662, https://doi.org/10.1038/nrrheum.2015.91 (2015).
Mok, Y. et al. Serum uric acid and chronic kidney disease: the Severance cohort study. Nephrol Dial Transplant 27, 1831–1835, https://doi.org/10.1093/ndt/gfr530 (2012).
Stegall, M. D., Cornell, L. D., Park, W. D., Smith, B. H. & Cosio, F. G. Renal Allograft Histology at 10 Years After Transplantation in the Tacrolimus Era: Evidence of Pervasive Chronic Injury. Am J Transplant 18, 180–188, https://doi.org/10.1111/ajt.14431 (2018).
Akalin, E., Ganeshan, S. V., Winston, J. & Muntner, P. Hyperuricemia is associated with the development of the composite outcomes of new cardiovascular events and chronic allograft nephropathy. Transplantation 86, 652–658, https://doi.org/10.1097/TP.0b013e3181814f5b (2008).
Hart, A. et al. Uric acid and allograft loss from interstitial fibrosis/tubular atrophy: post hoc analysis from the angiotensin II blockade in chronic allograft nephropathy trial. Transplantation 97, 1066–1071, https://doi.org/10.1097/01.TP.0000440952.29757.66 (2014).
Kanji, T., Gandhi, M., Clase, C. M. & Yang, R. Urate lowering therapy to improve renal outcomes in patients with chronic kidney disease: systematic review and meta-analysis. BMC Nephrol 16, 58, https://doi.org/10.1186/s12882-015-0047-z (2015).
Sircar, D. et al. Efficacy of Febuxostat for Slowing the GFR Decline in Patients With CKD and Asymptomatic Hyperuricemia: A 6-Month, Double-Blind, Randomized, Placebo-Controlled Trial. Am J Kidney Dis 66, 945–950, https://doi.org/10.1053/j.ajkd.2015.05.017 (2015).
Perez-Ruiz, F. et al. Long-term efficacy of hyperuricaemia treatment in renal transplant patients. Nephrol Dial Transplant 18, 603–606 (2003).
Osadchuk, L. et al. Effect of allopurinol on slowing allograft functional decline in kidney transplant recipients. Exp Clin Transplant 12, 190–194 (2014).
Pagonas, N. et al. Effects of Treatment of Asymptomatic Hyperuricemia on Graft Survival and Mortality in Kidney Transplant Recipients. Ann Transplant 21, 350–359, https://doi.org/10.12659/AOT.896821 (2016).
Racusen, L. C. et al. The Banff 97 working classification of renal allograft pathology. Kidney Int 55, 713–723, https://doi.org/10.1046/j.1523-1755.1999.00299.x (1999).
Sis, B. et al. Cluster analysis of lesions in nonselected kidney transplant biopsies: microcirculation changes, tubulointerstitial inflammation and scarring. Am J Transplant 10, 421–430, https://doi.org/10.1111/j.1600-6143.2009.02938.x (2010).
Solez, K. et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am J Transplant 8, 753–760, https://doi.org/10.1111/j.1600-6143.2008.02159.x (2008).
Acknowledgements
The authors thank Drs Soon Il Kim, Dong Jin Joo, Jae Geun Lee and Jee Youn Lee (Transplantation Surgery) for their significant contribution during follow-up of the patients.
Author information
Authors and Affiliations
Contributions
D.G.K., B.S.K., Y.S.K. participated in research design. D.G.K., H.J.J., B.J.L. participated in data acquisition. D.G.K., B.S.K., H.J.J., H.Y.C. participated in statistical analysis. Y.S.K., H.J.J., K.H.H., M.S.K. participated in the performance of the research. D.G.K., B.S.K. participated in data analysis.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, D.G., Kim, B.S., Choi, H.Y. et al. Association between post-transplant uric acid level and renal allograft fibrosis: Analysis using Banff pathologic scores from renal biopsies. Sci Rep 8, 11601 (2018). https://doi.org/10.1038/s41598-018-29948-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-29948-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.