Abstract
Ras homology (RHO) GTPases are signalling proteins that have crucial roles in triggering multiple immune functions. Through their interactions with a broad range of effectors and kinases, they regulate cytoskeletal dynamics, cell polarity and the trafficking and proliferation of immune cells. The activity and localization of RHO GTPases are highly controlled by classical families of regulators that share consensus motifs. In this Review, we describe the recent discovery of atypical modulators and partners of RHO GTPases, which bring an additional layer of regulation and plasticity to the control of RHO GTPase activities in the immune system. Furthermore, the development of large-scale genetic screening has now enabled researchers to identify dysregulation of RHO GTPase signalling pathways as a cause of many immune system-related diseases. We discuss the mutations that have been identified in RHO GTPases and their signalling circuits in patients with rare diseases. The discoveries of new RHO GTPase partners and genetic mutations in RHO GTPase signalling hubs have uncovered unsuspected layers of crosstalk with other signalling pathways and may provide novel therapeutic opportunities for patients affected by complex immune or broader syndromes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Takai, Y., Sasaki, T. & Matozaki, T. Small GTP-binding proteins. Physiol. Rev. 81, 153–208 (2001).
Heasman, S. J. & Ridley, A. J. Mammalian Rho GTPases: new insights into their functions from in vivo studies. Nat. Rev. Mol. Cell Biol. 9, 690–701 (2008).
Cherfils, J. & Zeghouf, M. Chronicles of the GTPase switch. Nat. Chem. Biol. 7, 493–495 (2011).
Hodge, R. G. & Ridley, A. J. Regulating Rho GTPases and their regulators. Nat. Rev. Mol. Cell Biol. 17, 496–510 (2016).
Aspenström, P. Fast-cycling Rho GTPases. Small GTPases 11, 248–255 (2020).
Cherfils, J. & Zeghouf, M. Regulation of small GTPases by GEFs, GAPs, and GDIs. Physiol. Rev. 93, 269–309 (2013).
Laurin, M. & Côté, J. F. Insights into the biological functions of Dock family guanine nucleotide exchange factors. Genes Dev. 28, 533–547 (2014).
Tcherkezian, J. & Lamarche-Vane, N. Current knowledge of the large RhoGAP family of proteins. Biol. Cell 99, 67–86 (2007).
Garcia-Mata, R., Boulter, E. & Burridge, K. The ‘invisible hand’: regulation of RHO GTPases by RHOGDIs. Nat. Rev. Mol. Cell Biol. 12, 493–504 (2011).
Peurois, F., Peyroche, G. & Cherfils, J. Small GTPase peripheral binding to membranes: molecular determinants and supramolecular organization. Biochem. Soc. Trans. 47, 13–22 (2019).
Wang, M. & Casey, P. J. Protein prenylation: unique fats make their mark on biology. Nat. Rev. Mol. Cell Biol. 17, 110–122 (2016).
Rougerie, P. et al. Fam65b is a new transcriptional target of FOXO1 that regulates RhoA signaling for T lymphocyte migration. J. Immunol. 190, 748–755 (2013). This study presents the first description of FAM65B as an atypical RHOA inhibitor that affects T cell migration by decreasing RHOA–GTP levels.
Gao, K. et al. Front-signal-dependent accumulation of the RHOA inhibitor FAM65B at leading edges polarizes neutrophils. J. Cell Sci. 128, 992–1000 (2015).
Uhlén, M. et al. Proteomics. Tissue-based map of the human proteome. Science 347, 1260419 (2015).
Megrelis, L. et al. Fam65b phosphorylation relieves tonic RhoA inhibition during T cell migration. Front. Immunol. 9, 2001 (2018).
Mardakheh, F. K., Self, A. & Marshall, C. J. RHO binding to FAM65A regulates Golgi reorientation during cell migration. J. Cell Sci. 129, 4466–4479 (2016).
Flynn, P., Mellor, H., Palmer, R., Panayotou, G. & Parker, P. J. Multiple interactions of PRK1 with RhoA. Functional assignment of the Hr1 repeat motif. J. Biol. Chem. 273, 2698–2705 (1998).
Froehlich, J. et al. FAM65B controls the proliferation of transformed and primary T cells. Oncotarget 7, 63215–63225 (2016).
Zhou, L. Y. et al. The circular RNA ACR attenuates myocardial ischemia/reperfusion injury by suppressing autophagy via modulation of the Pink1/ FAM65B pathway. Cell Death Differ. 26, 1299–1315 (2019).
Kong, K. F. et al. Protein kinase C-eta controls CTLA-4-mediated regulatory T cell function. Nat. Immunol. 15, 465–472 (2014).
Chen, Z. et al. Structure and control of the actin regulatory WAVE complex. Nature 468, 533–538 (2010).
Fort, L. et al. Fam49/CYRI interacts with Rac1 and locally suppresses protrusions. Nat. Cell Biol. 20, 1159–1171 (2018).
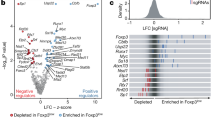
Shang, W. et al. Genome-wide CRISPR screen identifies FAM49B as a key regulator of actin dynamics and T cell activation. Proc. Natl Acad. Sci. USA 115, E4051–E4060 (2018). Fort et al. (2018) and Shang et al. (2018) provide the first descriptions of FAM49 as an inhibitor of RAC1.
Yuki, K. E. et al. CYRI/FAM49B negatively regulates RAC1-driven cytoskeletal remodelling and protects against bacterial infection. Nat. Microbiol. 4, 1516–1531 (2019).
Gilli, F. et al. Loss of braking signals during inflammation: a factor affecting the development and disease course of multiple sclerosis. Arch. Neurol. 68, 879–888 (2011).
Faroudi, M. et al. Critical roles for Rac GTPases in T-cell migration to and within lymph nodes. Blood 116, 5536–5547 (2010).
Kuramochi, S. et al. LOK is a novel mouse STE20-like protein kinase that is expressed predominantly in lymphocytes. J. Biol. Chem. 272, 22679–22684 (1997).
Walter, S. A., Cutler, R. E. Jr., Martinez, R., Gishizky, M. & Hill, R. J. Stk10, a new member of the polo-like kinase kinase family highly expressed in hematopoietic tissue. J. Biol. Chem. 278, 18221–18228 (2003).
Bagci, H. et al. Mapping the proximity interaction network of the Rho-family GTPases reveals signalling pathways and regulatory mechanisms. Nat. Cell Biol. 22, 120–134 (2020). This article maps the interaction network of RHO GTPases and identifies novel effectors.
Mott, H. R. & Owen, D. Structures of Ras superfamily effector complexes: what have we learnt in two decades? Crit. Rev. Biochem. Mol. Biol. 50, 85–133 (2015).
Belkina, N. V., Liu, Y., Hao, J. J., Karasuyama, H. & Shaw, S. LOK is a major ERM kinase in resting lymphocytes and regulates cytoskeletal rearrangement through ERM phosphorylation. Proc. Natl Acad. Sci. USA 106, 4707–4712 (2009).
Charrin, S. & Alcover, A. Role of ERM (ezrin-radixin-moesin) proteins in T lymphocyte polarization, immune synapse formation and in T cell receptor-mediated signaling. Front. Biosci. 11, 1987–1997 (2006).
Fehon, R. G., McClatchey, A. I. & Bretscher, A. Organizing the cell cortex: the role of ERM proteins. Nat. Rev. Mol. Cell Biol. 11, 276–287 (2010).
Garcia-Ortiz, A. & Serrador, J. M. ERM proteins at the crossroad of leukocyte polarization, migration and intercellular adhesion. Int. J. Mol. Sci. 21, 1502 (2020).
Endo, J. et al. Deficiency of a STE20/PAK family kinase LOK leads to the acceleration of LFA-1 clustering and cell adhesion of activated lymphocytes. FEBS Lett. 468, 234–238 (2000).
Lee, J. H. et al. Roles of p-ERM and Rho-ROCK signaling in lymphocyte polarity and uropod formation. J. Cell Biol. 167, 327–337 (2004).
Faure, S. et al. ERM proteins regulate cytoskeleton relaxation promoting T cell-APC conjugation. Nat. Immunol. 5, 272–279 (2004).
Nijhara, R. et al. Rac1 mediates collapse of microvilli on chemokine-activated T lymphocytes. J. Immunol. 173, 4985–4993 (2004).
Kim, S. Y. et al. Coordinated balance of Rac1 and RhoA plays key roles in determining phagocytic appetite. PLoS ONE 12, e0174603 (2017).
Salloum, G., Jaafar, L. & El-Sibai, M. RhoA and Rac1: antagonists moving forward. Tissue Cell 65, 101364 (2020).
Ishihara, S. et al. Dual functions of Rap1 are crucial for T-cell homeostasis and prevention of spontaneous colitis. Nat. Commun. 6, 8982 (2015).
Kinashi, T. & Katagiri, K. Regulation of lymphocyte adhesion and migration by the small GTPase Rap1 and its effector molecule, RAPL. Immunol. Lett. 93, 1–5 (2004).
Matsui, T., Yonemura, S. & Tsukita, S. Activation of ERM proteins in vivo by Rho involves phosphatidyl-inositol 4-phosphate 5-kinase and not ROCK kinases. Curr. Biol. 9, 1259–1262 (1999).
Matsui, T. et al. Rho-kinase phosphorylates COOH-terminal threonines of ezrin/radixin/moesin (ERM) proteins and regulates their head-to-tail association. J. Cell Biol. 140, 647–657 (1998).
Ormonde, J. V. S., Li, Z., Stegen, C. & Madrenas, J. TAOK3 regulates canonical TCR signaling by preventing early SHP-1-mediated inactivation of LCK. J. Immunol. 201, 3431–3442 (2018).
Ormonde, J. V. S., Nie, Y. & Madrenas, J. TAOK3, a regulator of LCK-SHP-1 crosstalk during TCR signaling. Crit. Rev. Immunol. 39, 59–81 (2019).
Hammad, H. et al. Transitional B cells commit to marginal zone B cell fate by Taok3-mediated surface expression of ADAM10. Nat. Immunol. 18, 313–320 (2017).
Youn, J. Y. et al. High-density proximity mapping reveals the subcellular organization of mRNA-associated granules and bodies. Mol. Cell 69, 517–532 e511 (2018).
Diaz-Horta, O. et al. Ripor2 is involved in auditory hair cell stereociliary bundle structure and orientation. J. Mol. Med. 96, 1227–1238 (2018).
Diaz-Horta, O. et al. FAM65B is a membrane-associated protein of hair cell stereocilia required for hearing. Proc. Natl Acad. Sci. USA 111, 9864–9868 (2014).
de Bruijn, S. E. et al. A RIPOR2 in-frame deletion is a frequent and highly penetrant cause of adult-onset hearing loss. J. Med. Genet. https://doi.org/10.1136/jmedgenet-2020-106863 (2020).
Aguilar, B. J., Zhou, H. & Lu, Q. Cdc42 signaling pathway inhibition as a therapeutic target in Ras- related cancers. Curr. Med. Chem. 24, 3485–3507 (2017).
Kazanietz, M. G. & Caloca, M. J. The Rac GTPase in cancer: from old concepts to new paradigms. Cancer Res. 77, 5445–5451 (2017).
Aspenström, P. Activated Rho GTPases in cancer-the beginning of a new paradigm. Int. J. Mol. Sci. 19, 3949 (2018).
Bustelo, X. R. RHO GTPases in cancer: known facts, open questions, and therapeutic challenges. Biochem. Soc. Trans. 46, 741–760 (2018).
Maldonado, M. D. M. & Dharmawardhane, S. Targeting Rac and Cdc42 GTPases in cancer. Cancer Res. 78, 3101–3111 (2018).
Voena, C. & Chiarle, R. RHO family GTPases in the biology of lymphoma. Cells 8, 646 (2019).
Cannon, A. C., Uribe-Alvarez, C. & Chernoff, J. RAC1 as a therapeutic target in malignant melanoma. Trends Cancer 6, 478–488 (2020).
Clayton, N. S. & Ridley, A. J. Targeting Rho GTPase signaling networks in cancer. Front. Cell Dev. Biol. 8, 222 (2020).
Jung, H., Yoon, S. R., Lim, J., Cho, H. J. & Lee, H. G. Dysregulation of Rho GTPases in human cancers. Cancers 12, 1179 (2020).
Bouafia, A. et al. Loss of ARHGEF1 causes a human primary antibody deficiency. J. Clin. Invest. 129, 1047–1060 (2019).
Serwas, N. K. et al. Human DEF6 deficiency underlies an immunodeficiency syndrome with systemic autoimmunity and aberrant CTLA-4 homeostasis. Nat. Commun. 10, 3106 (2019).
Dobbs, K. et al. Inherited DOCK2 deficiency in patients with early-onset invasive infections. N. Engl. J. Med. 372, 2409–2422 (2015).
Moens, L. et al. Human DOCK2 deficiency: report of a novel mutation and evidence for neutrophil dysfunction. J. Clin. Immunol. 39, 298–308 (2019).
Engelhardt, K. R. et al. Large deletions and point mutations involving the dedicator of cytokinesis 8 (DOCK8) in the autosomal-recessive form of hyper-IgE syndrome. J. Allergy Clin. Immunol. 124, 1289–1302 e1284 (2009).
Zhang, Q. et al. Combined immunodeficiency associated with DOCK8 mutations. N. Engl. J. Med. 361, 2046–2055 (2009).
Engelhardt, K. R. et al. The extended clinical phenotype of 64 patients with dedicator of cytokinesis 8 deficiency. J. Allergy Clin. Immunol. 136, 402–412 (2015).
Phatarpekar, P. V. et al. The septin cytoskeleton regulates natural killer cell lytic granule release. J. Cell Biol. 219, e202002145 (2020).
Randall, K. L. et al. DOCK8 deficiency impairs CD8 T cell survival and function in humans and mice. J. Exp. Med. 208, 2305–2320 (2011).
Dasouki, M. et al. Deficient T cell receptor excision circles (TRECs) in autosomal recessive hyper IgE syndrome caused by DOCK8 mutation: implications for pathogenesis and potential detection by newborn screening. Clin. Immunol. 141, 128–132 (2011).
Lambe, T. et al. DOCK8 is essential for T-cell survival and the maintenance of CD8+T-cell memory. Eur. J. Immunol. 41, 3423–3435 (2011).
Mizesko, M. C. et al. Defective actin accumulation impairs human natural killer cell function in patients with dedicator of cytokinesis 8 deficiency. J. Allergy Clin. Immunol. 131, 840–848 (2013).
Ham, H. et al. Dedicator of cytokinesis 8 interacts with talin and Wiskott-Aldrich syndrome protein to regulate NK cell cytotoxicity. J. Immunol. 190, 3661–3669 (2013).
Tangye, S. G. et al. Dedicator of cytokinesis 8-deficient CD4+ T cells are biased to a TH2 effector fate at the expense of TH1 and TH17 cells. J. Allergy Clin. Immunol. 139, 933–949 (2017).
Schneider, C. et al. Migration-induced cell shattering due to DOCK8 deficiency causes a type 2-biased helper T cell response. Nat. Immunol. 21, 1528–1539 (2020).
Keles, S. et al. Dedicator of cytokinesis 8 regulates signal transducer and activator of transcription 3 activation and promotes TH17 cell differentiation. J. Allergy Clin. Immunol. 138, 1384–1394 e1382 (2016).
Zhang, Q. et al. DOCK8 regulates lymphocyte shape integrity for skin antiviral immunity. J. Exp. Med. 211, 2549–2566 (2014). This study shows that DOCK8, which is associated with human immunodeficiency diseases, regulates the shape integrity of lymphocytes during migration through CDC42.
Janssen, E. et al. Dedicator of cytokinesis 8-deficient patients have a breakdown in peripheral B-cell tolerance and defective regulatory T cells. J. Allergy Clin. Immunol. 134, 1365–1374 (2014).
Keles, S. et al. Plasmacytoid dendritic cell depletion in DOCK8 deficiency: rescue of severe herpetic infections with IFN-alpha 2b therapy. J. Allergy Clin. Immunol. 133, 1753–1755 e1753 (2014).
Bittner, T. C. et al. Successful long-term correction of autosomal recessive hyper-IgE syndrome due to DOCK8 deficiency by hematopoietic stem cell transplantation. Klin. Padiatr. 222, 351–355 (2010).
Gatz, S. A. et al. Curative treatment of autosomal-recessive hyper-IgE syndrome by hematopoietic cell transplantation. Bone Marrow Transpl. 46, 552–556 (2011).
Sanal, O. et al. Additional diverse findings expand the clinical presentation of DOCK8 deficiency. J. Clin. Immunol. 32, 698–708 (2012).
Jing, H. et al. Somatic reversion in dedicator of cytokinesis 8 immunodeficiency modulates disease phenotype. J. Allergy Clin. Immunol. 133, 1667–1675 (2014).
Crequer, A. et al. Human RHOH deficiency causes T cell defects and susceptibility to EV-HPV infections. J. Clin. Invest. 122, 3239–3247 (2012).
Chae, H. D., Lee, K. E., Williams, D. A. & Gu, Y. Cross-talk between RhoH and Rac1 in regulation of actin cytoskeleton and chemotaxis of hematopoietic progenitor cells. Blood 111, 2597–2605 (2008).
Reijnders, M. R. F. et al. RAC1 missense mutations in developmental disorders with diverse phenotypes. Am. J. Hum. Genet. 101, 466–477 (2017).
Ambruso, D. R. et al. Human neutrophil immunodeficiency syndrome is associated with an inhibitory Rac2 mutation. Proc. Natl Acad. Sci. USA 97, 4654–4659 (2000).
Gu, Y. & Williams, D. A. RAC2 GTPase deficiency and myeloid cell dysfunction in human and mouse. J. Pediatr. Hematol. Oncol. 24, 791–794 (2002).
Accetta, D. et al. Human phagocyte defect caused by a Rac2 mutation detected by means of neonatal screening for T-cell lymphopenia. J. Allergy Clin. Immunol. 127, 535–538 e531-532 (2011).
Gu, Y. et al. Biochemical and biological characterization of a human Rac2 GTPase mutant associated with phagocytic immunodeficiency. J. Biol. Chem. 276, 15929–15938 (2001).
Hsu, A. P. et al. Dominant activating RAC2 mutation with lymphopenia, immunodeficiency, and cytoskeletal defects. Blood 133, 1977–1988 (2019).
Arrington, M. E., Temple, B., Schaefer, A. & Campbell, S. L. The molecular basis for immune dysregulation by the hyper-activated E62K mutant of the GTPase RAC2. J. Biol. Chem. 295, 12130–12142 (2020).
Alkhairy, O. K. et al. RAC2 loss-of-function mutation in 2 siblings with characteristics of common variable immunodeficiency. J. Allergy Clin. Immunol. 135, 1380–1384 (2015).
Sharapova, S. O. et al. Heterozygous activating mutation in RAC2 causes infantile-onset combined immunodeficiency with susceptibility to viral infections. Clin. Immunol. 205, 1–5 (2019).
Lougaris, V. et al. A monoallelic activating mutation in RAC2 resulting in a combined immunodeficiency. J. Allergy Clin. Immunol. 143, 1649–1653 (2019).
Stengel, K. & Zheng, Y. Cdc42 in oncogenic transformation, invasion, and tumorigenesis. Cell Signal. 23, 1415–1423 (2011).
Takenouchi, T., Kosaki, R., Niizuma, T., Hata, K. & Kosaki, K. Macrothrombocytopenia and developmental delay with a de novo CDC42 mutation: yet another locus for thrombocytopenia and developmental delay. Am. J. Med. Genet. A 167A, 2822–2825 (2015).
Takenouchi, T., Okamoto, N., Ida, S., Uehara, T. & Kosaki, K. Further evidence of a mutation in CDC42 as a cause of a recognizable syndromic form of thrombocytopenia. Am. J. Med. Genet. A 170A, 852–855 (2016).
Motokawa, M. et al. A hot-spot mutation in CDC42 (p.Tyr64Cys) and novel phenotypes in the third patient with Takenouchi-Kosaki syndrome. J. Hum. Genet. 63, 387–390 (2018).
Kalina, T. et al. EuroFlow standardized approach to diagnostic immunopheneotyping of severe PID in newborns and young children. Front. Immunol. 11, 371 (2020).
Bucciol, G. et al. Systemic inflammation and Myelofibrosis in a patient with Takenouchi-Kosaki syndrome due to CDC42 Tyr64Cys mutation. J. Clin. Immunol. 40, 567–570 (2020).
Hamada, N. et al. Neuropathophysiological significance of the c.1449T>C/p.(Tyr64Cys) mutation in the CDC42 gene responsible for Takenouchi-Kosaki syndrome. Biochem. Biophys. Res. Commun. 529, 1033–1037 (2020).
Martinelli, S. et al. Functional dysregulation of CDC42 causes diverse developmental phenotypes. Am. J. Hum. Genet. 102, 309–320 (2018). This report establishes the first genotype–phenotype relationships in patients with various mutations in CDC42.
Szczawinska-Poplonyk, A., Ploski, R., Bernatowska, E. & Pac, M. A novel CDC42 mutation in an 11-year old child manifesting as syndromic immunodeficiency, autoinflammation, hemophagocytic lymphohistiocytosis, and malignancy: a case report. Front. Immunol. 11, 318 (2020).
Gernez, Y. et al. Severe autoinflammation in 4 patients with C-terminal variants in cell division control protein 42 homolog (CDC42) successfully treated with IL-1beta inhibition. J. Allergy Clin. Immunol. 144, 1122–1125 e1126 (2019).
Lam, M. T. et al. A novel disorder involving dyshematopoiesis, inflammation, and HLH due to aberrant CDC42 function. J. Exp. Med. 216, 2778–2799 (2019).
Bekhouche, B. et al. A toxic palmitoylation of Cdc42 enhances NF-kappaB signaling and drives a severe autoinflammatory syndrome. J. Allergy Clin. Immunol. 146, 1201–1204 (2020).
He, T., Huang, Y., Ling, J. & Yang, J. A new patient with NOCARH syndrome due to CDC42 defect. J. Clin. Immunol. 40, 571–575 (2020).
Verboon, J. M. et al. Infantile myelofibrosis and myeloproliferation with CDC42 dysfunction. J. Clin. Immunol. 40, 554–566 (2020).
Johnson, J. L., Erickson, J. W. & Cerione, R. A. C-terminal di-arginine motif of Cdc42 protein is essential for binding to phosphatidylinositol 4,5-bisphosphate-containing membranes and inducing cellular transformation. J. Biol. Chem. 287, 5764–5774 (2012).
Akula, M. K. et al. Protein prenylation restrains innate immunity by inhibiting Rac1 effector interactions. Nat. Commun. 10, 3975 (2019).
Akula, M. K. et al. Control of the innate immune response by the mevalonate pathway. Nat. Immunol. 17, 922–929 (2016).
Park, Y. H., Wood, G., Kastner, D. L. & Chae, J. J. Pyrin inflammasome activation and RhoA signaling in the autoinflammatory diseases FMF and HIDS. Nat. Immunol. 17, 914–921 (2016).
Schnappauf, O., Chae, J. J., Kastner, D. L. & Aksentijevich, I. The pyrin inflammasome in health and disease. Front. Immunol. 10, 1745 (2019).
Özen, S., Batu, E. D. & Demir, S. Familial Mediterranean fever: recent developments in pathogenesis and new recommendations for management. Front. Immunol. 8, 253 (2017).
Migita, K. et al. Familial Mediterranean fever: overview of pathogenesis, clinical features and management. Immunol. Med. 41, 55–61 (2018).
Jamilloux, Y., Magnotti, F., Belot, A. & Henry, T. The pyrin inflammasome: from sensing RhoA GTPases-inhibiting toxins to triggering autoinflammatory syndromes. Pathog. Dis. https://doi.org/10.1093/femspd/fty020 (2018).
Xu, H. et al. Innate immune sensing of bacterial modifications of Rho GTPases by the Pyrin inflammasome. Nature 513, 237–241 (2014).
Vabres, P. et al. Postzygotic inactivating mutations of RHOA cause a mosaic neuroectodermal syndrome. Nat. Genet. 51, 1438–1441 (2019).
Harms, F. L. et al. Activating mutations in PAK1, encoding p21-activated kinase 1, cause a neurodevelopmental disorder. Am. J. Hum. Genet. 103, 579–591 (2018).
Kernohan, K. D. et al. p21 protein-activated kinase 1 is associated with severe regressive autism, and epilepsy. Clin. Genet. 96, 449–455 (2019).
Ohori, S. et al. A novel PAK1 variant causative of neurodevelopmental disorder with postnatal macrocephaly. J. Hum. Genet. 65, 481–485 (2020).
Fritz-Laylin, L. K., Lord, S. J. & Mullins, R. D. WASP and SCAR are evolutionarily conserved in actin-filled pseudopod-based motility. J. Cell Biol. 216, 1673–1688 (2017).
Fritz-Laylin, L. K. et al. Actin-based protrusions of migrating neutrophils are intrinsically lamellar and facilitate direction changes. eLife 6, 437 (2017).
Westerberg, L. et al. Wiskott-Aldrich syndrome protein deficiency leads to reduced B-cell adhesion, migration, and homing, and a delayed humoral immune response. Blood 105, 1144–1152 (2005).
Zhang, X. et al. Abnormalities of follicular helper T-cell number and function in Wiskott-Aldrich syndrome. Blood 127, 3180–3191 (2016).
Zhou, L. et al. Abnormal distribution of distinct lymphocyte subsets in children with Wiskott-Aldrich syndrome. Hum. Immunol. 78, 565–573 (2017).
Cotta-de-Almeida, V., Dupré, L., Guipouy, D. & Vasconcelos, Z. Signal integration during T lymphocyte activation and function: lessons from the Wiskott-Aldrich syndrome. Front. Immunol. 6, 47 (2015).
Rivers, E. & Thrasher, A. J. Wiskott-Aldrich syndrome protein: emerging mechanisms in immunity. Eur. J. Immunol. 47, 1857–1866 (2017). This review provides an overview of the roles of WASp in innate and adaptive immunity and clarifies mechanistic insights into Wiskott–Aldrich syndrome.
Sun, X., Wei, Y., Lee, P. P., Ren, B. & Liu, C. The role of WASp in T cells and B cells. Cell Immunol. 341, 103919 (2019).
de Noronha, S. et al. Impaired dendritic-cell homing in vivo in the absence of Wiskott-Aldrich syndrome protein. Blood 105, 1590–1597 (2005).
Snapper, S. B. et al. WASP deficiency leads to global defects of directed leukocyte migration in vitro and in vivo. J. Leukoc. Biol. 77, 993–998 (2005).
Haddad, E. et al. The interaction between Cdc42 and WASP is required for SDF-1-induced T-lymphocyte chemotaxis. Blood 97, 33–38 (2001).
Lanzi, G. et al. A novel primary human immunodeficiency due to deficiency in the WASP-interacting protein WIP. J. Exp. Med. 209, 29–34 (2012).
Gallego, M. D. et al. WIP and WASP play complementary roles in T cell homing and chemotaxis to SDF-1alpha. Int. Immunol. 18, 221–232 (2006).
Castiello, M. C. et al. Wiskott-Aldrich syndrome protein deficiency perturbs the homeostasis of B-cell compartment in humans. J. Autoimmun. 50, 42–50 (2014).
Dupré, L. et al. Wiskott-Aldrich syndrome protein regulates lipid raft dynamics during immunological synapse formation. Immunity 17, 157–166 (2002).
Kumari, S. et al. Actin foci facilitate activation of the phospholipase C-gamma in primary T lymphocytes via the WASP pathway. eLife 4, e04953 (2015).
Rey-Suarez, I. et al. WASP family proteins regulate the mobility of the B cell receptor during signaling activation. Nat. Commun. 11, 439 (2020).
Lorenzi, R., Brickell, P. M., Katz, D. R., Kinnon, C. & Thrasher, A. J. Wiskott-Aldrich syndrome protein is necessary for efficient IgG-mediated phagocytosis. Blood 95, 2943–2946 (2000).
Tsuboi, S. & Meerloo, J. Wiskott-Aldrich syndrome protein is a key regulator of the phagocytic cup formation in macrophages. J. Biol. Chem. 282, 34194–34203 (2007).
Orange, J. S. et al. Wiskott-Aldrich syndrome protein is required for NK cell cytotoxicity and colocalizes with actin to NK cell-activating immunologic synapses. Proc. Natl Acad. Sci. USA 99, 11351–11356 (2002).
Gismondi, A. et al. Impaired natural and CD16-mediated NK cell cytotoxicity in patients with WAS and XLT: ability of IL-2 to correct NK cell functional defect. Blood 104, 436–443 (2004).
Lee, P. P. et al. Wiskott-Aldrich syndrome protein regulates autophagy and inflammasome activity in innate immune cells. Nat. Commun. 8, 1576 (2017).
Taylor, M. D. et al. Nuclear role of WASp in the pathogenesis of dysregulated TH1 immunity in human Wiskott-Aldrich syndrome. Sci. Transl Med. 2, 37ra44 (2010).
Hurst, V., Shimada, K. & Gasser, S. M. Nuclear actin and actin-binding proteins in DNA repair. Trends Cell Biol. 29, 462–476 (2019).
Keszei, M. et al. Constitutive activation of WASp in X-linked neutropenia renders neutrophils hyperactive. J. Clin. Invest. 128, 4115–4131 (2018).
Al-Mousa, H. et al. Hematopoietic stem cell transplantation corrects WIP deficiency. J. Allergy Clin. Immunol. 139, 1039–1040 e1034 (2017).
Rai, R. et al. Targeted gene correction of human hematopoietic stem cells for the treatment of Wiskott - Aldrich syndrome. Nat. Commun. 11, 4034 (2020).
Pala, F. et al. Lentiviral-mediated gene therapy restores B cell tolerance in Wiskott-Aldrich syndrome patients. J. Clin. Invest. 125, 3941–3951 (2015).
Schaefer, A., Reinhard, N. R. & Hordijk, P. L. Toward understanding RhoGTPase specificity: structure, function and local activation. Small GTPases 5, 6 (2014).
Madaule, P. & Axel, R. A novel ras-related gene family. Cell 41, 31–40 (1985).
Didsbury, J., Weber, R. F., Bokoch, G. M., Evans, T. & Snyderman, R. rac, a novel ras-related family of proteins that are botulinum toxin substrates. J. Biol. Chem. 264, 16378–16382 (1989).
Adams, A. E., Johnson, D. I., Longnecker, R. M., Sloat, B. F. & Pringle, J. R. CDC42 and CDC43, two additional genes involved in budding and the establishment of cell polarity in the yeast Saccharomyces cerevisiae. J. Cell Biol. 111, 131–142 (1990).
Johnson, D. I. & Pringle, J. R. Molecular characterization of CDC42, a Saccharomyces cerevisiae gene involved in the development of cell polarity. J. Cell Biol. 111, 143–152 (1990).
Ridley, A. J. & Hall, A. The small GTP-binding protein rho regulates the assembly of focal adhesions and actin stress fibers in response to growth factors. Cell 70, 389–399 (1992). This study is the first to show a role for RHOA in actin polymerization.
Ridley, A. J., Paterson, H. F., Johnston, C. L., Diekmann, D. & Hall, A. The small GTP-binding protein rac regulates growth factor-induced membrane ruffling. Cell 70, 401–410 (1992). This article shows that RAC1 generates actin filaments that are organized in ruffles.
Nobes, C. D. & Hall, A. Rho, rac, and cdc42 GTPases regulate the assembly of multimolecular focal complexes associated with actin stress fibers, lamellipodia, and filopodia. Cell 81, 53–62 (1995). This report establishes that the three most common members of the RHO GTPase family can polymerize actin filaments and organize them in different types of array.
Valitutti, S., Dessing, M., Aktories, K., Gallati, H. & Lanzavecchia, A. Sustained signaling leading to T cell activation results from prolonged T cell receptor occupancy. Role T cell actin cytoskeleton. J. Exp. Med. 181, 577–584 (1995).
Delon, J., Bercovici, N., Liblau, R. & Trautmann, A. Imaging antigen recognition by naive CD4+ T cells: compulsory cytoskeletal alterations for the triggering of an intracellular calcium response. Eur. J. Immunol. 28, 716–729 (1998).
Acuto, O. & Cantrell, D. T cell activation and the cytoskeleton. Annu. Rev. Immunol. 18, 165–184 (2000).
Acknowledgements
This work was supported by Inserm, CNRS, Université de Paris, the French Agence Nationale de la Recherche, Société Française de Dermatologie, Programme Germaine de Stael and Fondation ARC. The authors thank E. Bloch-Gallego, M. Mangeney and C. Randriamampita for critical reading of the manuscript. The authors apologize to colleagues whose work could not be cited owing to space limitations.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Immunology thanks I. Meyts and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Glossary
- SCAR/WAVE proteins
-
Suppressor of cAMP receptor/Wiskott–Aldrich syndrome protein (WASp) family verprolin homology proteins. A complex of WASp family-related proteins that are implicated in the regulation of cytoskeletal organization, lamellipodium formation, actin dynamics and cell motility through the activation of actin-related protein 2/3 (ARP2/3) complex-dependent actin nucleation.
- Pseudopod
-
A filamentous actin-rich projection of the cell membrane of leukocytes formed to trigger cell migration and to direct their movement in response to a chemoattractive stimulus.
- Ezrin/radixin/moesin proteins
-
(ERM proteins). Highly homologous proteins involved in multiple cellular processes, notably cell migration and activation, by crosslinking plasma membrane proteins to the underlying cortical actin cytoskeleton when they adopt an open conformation upon phosphorylation.
- Marginal zone B cells
-
A subpopulation of B cells localized in the spleen and lymph nodes at the site of exposure to antigens, where they can rapidly proliferate and differentiate into IgM+ plasmablasts.
- RNA processing bodies
-
(P-bodies). Cytoplasmic aggregates composed of mRNA and proteins that are involved in mRNA decay and translation repression.
- Septins
-
Guanosine triphosphate (GTP)-binding, membrane-interacting proteins that are highly conserved components of the cytoskeletal system and are involved in multiple cellular processes, including cytokinesis, cell polarity and membrane dynamics, through their capacity to adopt variable architectures.
- TCR excision circles
-
Small circular DNA fragments generated by developing T cells in the thymus as a product of the rearrangement of gene segments encoding the variable domains of the T cell receptor (TCR).
- Wiskott–Aldrich syndrome protein
-
(WASp). A cytoplasmic signalling protein expressed in haematopoietic cells that regulates the actin cytoskeleton through the control of actin-related protein 2/3 (ARP2/3) complex activity and that participates in both innate and adaptive immune responses.
- Somatic reversion
-
Genetic mechanism by which a DNA mutation is repaired to give back a normal protein.
- Switch II domain
-
A region of the Ras homology (RHO) GTPases that has the capacity to change its conformation according to the nature of the bound phosphate group (guanosine diphosphate (GDP) or guanosine triphosphate (GTP)), which switches the activity state of the protein and affects its interaction with regulator and effector proteins.
- Noonan syndrome
-
A common genetic multisystem disorder characterized by variable phenotypes, including typical facial features, developmental delay, short stature, congenital heart defects, renal anomalies, lymphatic malformations, bleeding difficulties and learning disabilities, caused by mutations in the genes encoding proteins involved in the RAS–mitogen-activated protein kinase signalling pathway.
- Familial Mediterranean fever syndrome
-
An autoinflammatory disease caused by mutations in MEFV, which encodes a 781 amino acid protein known as pyrin.
- Actin-related protein 2/3 complex
-
(ARP2/3 complex). A seven-subunit conserved protein complex that nucleates branched actin filament networks and finely regulates their organization in crucial cellular functions, including cell migration, endocytosis, phagocytosis, vesicular trafficking and cytokinesis, through its interaction with nucleation-promoting factors such as Wiskott–Aldrich syndrome protein (WASp) and the SCAR/WAVE proteins.
Rights and permissions
About this article
Cite this article
El Masri, R., Delon, J. RHO GTPases: from new partners to complex immune syndromes. Nat Rev Immunol 21, 499–513 (2021). https://doi.org/10.1038/s41577-021-00500-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41577-021-00500-7
This article is cited by
-
Relapsing polychondritis: clinical updates and new differential diagnoses
Nature Reviews Rheumatology (2024)
-
RhoA promotes osteoclastogenesis and regulates bone remodeling through mTOR-NFATc1 signaling
Molecular Medicine (2023)
-
Protein kinases: drug targets for immunological disorders
Nature Reviews Immunology (2023)
-
Longitudinal dynamics of circulating miRNAs in a swine model of familial hypercholesterolemia during early atherosclerosis
Scientific Reports (2023)
-
TRIM40 is a pathogenic driver of inflammatory bowel disease subverting intestinal barrier integrity
Nature Communications (2023)