Abstract
Peripheral neurons that sense glucose relay signals of glucose availability to integrative clusters of neurons in the brain. However, the roles of such signalling pathways in the maintenance of glucose homoeostasis and their contribution to disease are unknown. Here we show that the selective activation of the nerve plexus of the hepatic portal system via peripheral focused ultrasound stimulation (pFUS) improves glucose homoeostasis in mice and rats with insulin-resistant diabetes and in swine subject to hyperinsulinemic-euglycaemic clamps. pFUS modulated the activity of sensory projections to the hypothalamus, altered the concentrations of metabolism-regulating neurotransmitters, and enhanced glucose tolerance and utilization in the three species, whereas physical transection or chemical blocking of the liver–brain nerve pathway abolished the effect of pFUS on glucose tolerance. Longitudinal multi-omic profiling of metabolic tissues from the treated animals confirmed pFUS-induced modifications of key metabolic functions in liver, pancreas, muscle, adipose, kidney and intestinal tissues. Non-invasive ultrasound activation of afferent autonomic nerves may represent a non-pharmacologic therapy for the restoration of glucose homoeostasis in type-2 diabetes and other metabolic diseases.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
The main data supporting the results in this study are available within the manuscript and its Supplementary Information. Source data for the figures are provided with this paper. The RNA-sequencing datasets generated during the study are available in the US National Center for Biotechnology Information Search (NCBI) Gene Expression Omnibus (GEO) repository (series record: GSE197097). Source data are provided with this paper.
Code availability
The source codes used for the data analyses of the study are available on request.
References
Shahriari, D., Rosenfeld, D. & Anikeeva, P. Emerging frontier of peripheral nerve and organ interfaces. Neuron 108, 270–285 (2020).
Pavlov, V. A. & Tracey, K. J. The vagus nerve and the inflammatory reflex—linking immunity and metabolism. Nat. Rev. Endocrinol. 8, 743–754 (2012).
Tracey, K. J. Reflex control of immunity. Nat. Rev. Immunol. 9, 418–428 (2009).
Tracey, K. J. Reflexes in immunity. Cell 164, 343–344 (2016).
Wang, H. et al. Nicotinic acetylcholine receptor α7 subunit is an essential regulator of inflammation. Nature 421, 384–388 (2002).
Koopman, F. A. et al. Vagus nerve stimulation inhibits cytokine production and attenuates disease severity in rheumatoid arthritis. Proc. Natl Acad. Sci. USA 113, 8284–8289 (2016).
Birmingham, K. et al. Bioelectronic medicines: a research roadmap. Nat. Rev. Drug Discov. 13, 399–400 (2014).
Olofsson, P. S. & Tracey, K. J. Bioelectronic medicine: technology targeting molecular mechanisms for therapy. J. Intern. Med. 282, 3–4 (2017).
Bonaz, B. et al. Chronic vagus nerve stimulation in Crohn’s disease: a 6-month follow-up pilot study. Neurogastroenterol. Motil. 28, 948–953 (2016).
Datta-Chaudhuri, T. et al. The Fourth Bioelectronic Medicine Summit ‘Technology Targeting Molecular Mechanisms’: current progress, challenges, and charting the future. Bioelectron. Med. 7, 7 (2021).
Puleo, C. & Cotero, V. Noninvasive neuromodulation of peripheral nerve pathways using ultrasound and its current therapeutic implications. Cold Spring Harb. Perspect. Med. 10, a034215 (2020).
Chen, R., Romero, G., Christiansen, M. G., Mohr, A. & Anikeeva, P. Wireless magnetothermal deep brain stimulation. Science 347, 1477–1480 (2015).
Kim, C. K., Adhikari, A. & Deisseroth, K. Integration of optogenetics with complementary methodologies in systems neuroscience. Nat. Rev. Neurosci. 18, 222–235 (2017).
Ibsen, S., Tong, A., Schutt, C., Esener, S. & Chalasani, S. H. Sonogenetics is a non-invasive approach to activating neurons in Caenorhabditis elegans. Nat. Commun. 6, 8264 (2015).
Cotero, V. et al. Noninvasive sub-organ ultrasound stimulation for targeted neuromodulation. Nat. Commun. 10, 952 (2019).
Cotero, V. et al. Peripheral focused ultrasound stimulation (pFUS): new competitor in pharmaceutical markets? SLAS Technol. 24, 448–452 (2019).
Huerta, T. S. et al. Targeted peripheral focused ultrasound stimulation attenuates obesity-induced metabolic and inflammatory dysfunctions. Sci. Rep. 11, 5083 (2021).
Cotero, V. et al. Peripheral focused ultrasound neuromodulation (pFUS). J. Neurosci. Methods 341, 108721 (2020).
Akhtar, K. et al. Non-invasive peripheral focused ultrasound neuromodulation of the celiac plexus ameliorates symptoms in a rat model of inflammatory bowel disease. Exp. Physiol. 106, 1038–1060 (2021).
Malbert, C.-H., Picq, C., Divoux, J.-L., Henry, C. & Horowitz, M. Obesity-associated alterations in glucose metabolism are reversed by chronic bilateral stimulation of the abdominal vagus nerve. Diabetes 66, 848–857 (2017).
Meyers, E. E., Kronemberger, A., Lira, V., Rahmouni, K. & Stauss, H. M. Contrasting effects of afferent and efferent vagal nerve stimulation on insulin secretion and blood glucose regulation. Physiol. Rep. 4, e12718 (2016).
Stauss, H., Meyers, E., Glab, T. & Rahmouni, K. Modulation of blood glucose concentration by vagal nerve stimulation. FASEB J. 29, 828.6 (2015).
Tanida, M. et al. Leptin receptor signalling in the hypothalamus regulates hepatic autonomic nerve activity via phosphatidylinositol 3-kinase and AMP-activated protein kinase. J. Neurosci. 35, 474–484 (2015).
Chen, J., Pasricha, P. J., Yin, J., Lin, L. & Chen, J. D. Z. Hepatic electrical stimulation reduces blood glucose in diabetic rats. Neurogastroenterol. Motil. 22, 1109–e286 (2010).
Pocai, A., Obici, S., Schwartz, G. J. & Rossetti, L. A brain–liver circuit regulates glucose homeostasis. Cell Metab. 1, 53–61 (2005).
Burcelin, R., Dolci, W. & Thorens, B. Glucose sensing by the hepatoportal sensor is GLUT2-dependent: in vivo analysis in GLUT2-null mice. Diabetes 49, 1643–1648 (2000).
Lam, T. K. T. Neuronal regulation of homeostasis by nutrient sensing. Nat. Med. 16, 392–395 (2010).
Lam, T. K. T. et al. Hypothalamic sensing of circulating fatty acids is required for glucose homeostasis. Nat. Med. 11, 320–327 (2005).
Delaere, F., Magnan, C. & Mithieux, G. Hypothalamic integration of portal glucose signals and control of food intake and insulin sensitivity. Diabetes Metab. 36, 257–262 (2010).
Delaere, F. et al. The role of sodium-coupled glucose co-transporter 3 in the satiety effect of portal glucose sensing. Mol. Metab. 2, 47–53 (2013).
Cherrington, A. D. Banting Lecture 1997. Control of glucose uptake and release by the liver in vivo. Diabetes 48, 1198–1214 (1999).
Coate, K. C. et al. Portal vein glucose entry triggers a coordinated cellular response that potentiates hepatic glucose uptake and storage in normal but not high-fat/high-fructose-fed dogs. Diabetes 62, 392–400 (2013).
Mithieux, G. Metabolic effects of portal vein sensing. Diabetes Obes. Metab. 16, 56–60 (2014).
Pal, A., Rhoads, D. B. & Tavakkoli, A. Effect of portal glucose sensing on systemic glucose levels in SD and ZDF rats. PLoS ONE 11, e0165592 (2016).
Burcelin, R. et al. GLUT4, AMP kinase, but not the insulin receptor, are required for hepatoportal glucose sensor-stimulated muscle glucose utilization. J. Clin. Invest. 111, 1555–1562 (2003).
Kraft, G. et al. Portal glucose delivery stimulates muscle but not liver protein metabolism. Am. J. Physiol. Metab. 303, E1202–E1211 (2012).
Yi, C.-X., la Fleur, S. E., Fliers, E. & Kalsbeek, A. The role of the autonomic nervous liver innervation in the control of energy metabolism. Biochim. Biophys. Acta 1802, 416–431 (2010).
Moore, M. C. et al. Effect of hepatic nerves on disposition of an intraduodenal glucose load. Am. J. Physiol. 265, E487–E496 (1993).
Wasserman, D. H., Williams, P. E., Lacy, D. B., Bracy, D. & Cherrington, A. D. Hepatic nerves are not essential to the increase in hepatic glucose production during muscular work. Am. J. Physiol. 259, E195–E203 (1990).
Chan, O. & Sherwin, R. S. Is there cross talk between portal and hypothalamic glucose-sensing circuits? Diabetes 63, 2617–2619 (2014).
Levin, B. E., Kang, L., Sanders, N. M. & Dunn-Meynell, A. A. Role of neuronal glucosensing in the regulation of energy homeostasis. Diabetes 55, S122 LP–S122130 (2006).
Jo, Y.-H. & Chua, S. C. The brain–liver connection between BDNF and glucose control. Diabetes 62, 1367–1368 (2013).
Uno, K. et al. Neuronal pathway from the liver modulates energy expenditure and systemic insulin sensitivity. Science 312, 1656–1659 (2006).
Tahrani, A. A., Barnett, A. H. & Bailey, C. J. Pharmacology, and therapeutic implications of current drugs for type 2 diabetes mellitus. Nat. Rev. Endocrinol. 12, 566–592 (2016).
Jokiaho, A. J., Donovan, C. M. & Watts, A. G. The rate of fall of blood glucose determines the necessity of forebrain-projecting catecholaminergic neurons for male rat sympathoadrenal responses. Diabetes 63, 2854–2865 (2014).
Bohland, M. et al. Activation of hindbrain neurons is mediated by portal-mesenteric vein glucosensors during slow-onset hypoglycemia. Diabetes 63, 2866–2875 (2014).
Fujita, S. & Donovan, C. M. Celiac-superior mesenteric ganglionectomy, but not vagotomy, suppresses the sympathoadrenal response to insulin-induced hypoglycemia. Diabetes 54, 3258–3264 (2005).
Randich, A., Spraggins, D. S., Cox, J. E., Meller, S. T. & Kelm, G. R. Jejunal or portal vein infusions of lipids increase hepatic vagal afferent activity. Neuroreport 12, 3101–3105 (2001).
Routh, V. H., Hao, L., Santiago, A. M., Sheng, Z. & Zhou, C. Hypothalamic glucose sensing: making ends meet. Front. Syst. Neurosci. 8, 236 (2014).
Adachi, A., Shimizu, N., Oomura, Y. & Kobáshi, M. Convergence of hepatoportal glucose-sensitive afferent signals to glucose-sensitive units within the nucleus of the solitary tract. Neurosci. Lett. 46, 215–218 (1984).
Kandilis, A. N., Papadopoulou, I. P., Koskinas, J., Sotiropoulos, G. & Tiniakos, D. G. Liver innervation and hepatic function: new insights. J. Surg. Res. 194, 511–519 (2015).
Kalra, S. P. Disruption in the leptin–NPY link underlies the pandemic of diabetes and metabolic syndrome: new therapeutic approaches. Nutrition 24, 820–826 (2008).
Chee, M. J. S., Myers, M. G. J., Price, C. J. & Colmers, W. F. Neuropeptide Y suppresses anorexigenic output from the ventromedial nucleus of the hypothalamus. J. Neurosci. 30, 3380–3390 (2010).
Loh, K., Herzog, H. & Shi, Y.-C. Regulation of energy homeostasis by the NPY system. Trends Endocrinol. Metab. 26, 125–135 (2015).
Engström Ruud, L., Pereira, M. M. A., de Solis, A. J., Fenselau, H. & Brüning, J. C. NPY mediates the rapid feeding and glucose metabolism regulatory functions of AgRP neurons. Nat. Commun. 11, 442 (2020).
Cowley, M. A. et al. Leptin activates anorexigenic POMC neurons through a neural network in the arcuate nucleus. Nature 411, 480–484 (2001).
Hahn, T. M., Breininger, J. F., Baskin, D. G. & Schwartz, M. W. Co-expression of Agrp and NPY in fasting-activated hypothalamic neurons. Nat. Neurosci. 1, 271–272 (1998).
O’Hare, J. D. & Zsombok, A. Brain-liver connections: role of the pre-autonomic PVN neurons. Am. J. Physiol. Endocrinol. Metab. 310, E183–E189 (2016).
Fenselau, H. et al. A rapidly acting glutamatergic ARC→PVH satiety circuit post-synaptically regulated by α-MSH. Nat. Neurosci. 20, 42–51 (2017).
Van den Pol, A. N., Acuna, C., Davis, J. N., Huang, H. & Zhang, X. Defining the caudal hypothalamic arcuate nucleus with a focus on anorexic excitatory neurons. J. Physiol. 597, 1605–1625 (2019).
Wang, P. et al. A leptin-BDNF pathway regulating sympathetic innervation of adipose tissue. Nature 583, 839–844 (2020).
Miki, T. et al. ATP-sensitive K+ channels in the hypothalamus are essential for the maintenance of glucose homeostasis. Nat. Neurosci. 4, 507–512 (2001).
Murphy, B. A., Fakira, K. A., Song, Z., Beuve, A. & Routh, V. H. AMP-activated protein kinase and nitric oxide regulate the glucose sensitivity of ventromedial hypothalamic glucose-inhibited neurons. Am. J. Physiol. Cell Physiol. 297, C750–C758 (2009).
Routh, V. H. Glucose sensing neurons in the ventromedial hypothalamus. Sensors 10, 9002–9025 (2010).
Cotero, V. E. & Routh, V. H. Insulin blunts the response of glucose-excited neurons in the ventrolateral-ventromedial hypothalamic nucleus to decreased glucose. Am. J. Physiol. Endocrinol. Metab. 296, E1101–E1109 (2009).
Cotero, V. E., Zhang, B. B. & Routh, V. H. The response of glucose-excited neurones in the ventromedial hypothalamus to decreased glucose is enhanced in a murine model of type 2 diabetes mellitus. J. Neuroendocrinol. 22, 65–74 (2010).
Gardemann, A., Strulik, H. & Jungermann, K. A portal-arterial glucose concentration gradient as a signal for an insulin-dependent net glucose uptake in perfused rat liver. FEBS Lett. 202, 255–259 (1986).
Moore, M. C., Coate, K. C., Winnick, J. J., An, Z. & Cherrington, A. D. Regulation of hepatic glucose uptake and storage in vivo. Adv. Nutr. 3, 286–294 (2012).
Wang, R. et al. The regulation of glucose-excited neurons in the hypothalamic arcuate nucleus by glucose and feeding-relevant peptides. Diabetes 53, 1959–1965 (2004).
Williams, G. et al. The hypothalamus and the control of energy homeostasis: different circuits, different purposes. Physiol. Behav. 74, 683–701 (2001).
Marty, N., Dallaporta, M. & Thorens, B. Brain glucose sensing, counter-regulation, and energy homeostasis. Physiology 22, 241–251 (2007).
Karnani, M. & Burdakov, D. Multiple hypothalamic circuits sense and regulate glucose levels. Am. J. Physiol. Integr. Comp. Physiol. 300, R47–R55 (2010).
Ren, H. et al. Altered central nutrient sensing in male mice lacking insulin receptors in Glut4-expressing neurons. Endocrinology 160, 2038–2048 (2019).
King, B. M. The rise, fall, and resurrection of the ventromedial hypothalamus in the regulation of feeding behaviour and body weight. Physiol. Behav. 87, 221–244 (2006).
Muroya, S., Yada, T., Shioda, S. & Takigawa, M. Glucose-sensitive neurons in the rat arcuate nucleus contain neuropeptide Y. Neurosci. Lett. 264, 113–116 (1999).
Ibrahim, N. et al. Hypothalamic proopiomelanocortin neurons are glucose responsive and express K(ATP) channels. Endocrinology 144, 1331–1340 (2003).
Moparthi, L. & Zygmunt, P. M. Human TRPA1 is an inherently mechanosensitive bilayer-gated ion channel. Cell Calcium 91, 102255 (2020).
Bae, C., Sachs, F. & Gottlieb, P. A. The mechanosensitive ion channel Piezo1 Is inhibited by the peptide GsMTx4. Biochemistry 50, 6295–6300 (2011).
De Rutte, J. M., Koh, J. & Di Carlo, D. Scalable high-throughput production of modular microgels for in situ assembly of microporous tissue scaffolds. Adv. Funct. Mater. 29, 1900071 (2019).
Motter, A. L. & Ahern, G. P. TRPA1 is a polyunsaturated fatty acid sensor in mammals. PLoS ONE 7, e38439 (2012).
Kong, X. et al. Roux-en-Y gastric bypass enhances insulin secretion in type 2 diabetes via FXR-mediated TRPA1 expression. Mol. Metab. 29, 1–11 (2019).
Derbenev, A. V. & Zsombok, A. Potential therapeutic value of TRPV1 and TRPA1 in diabetes mellitus and obesity. Semin. Immunopathol. 38, 397–406 (2016).
Li, M. et al. Transient receptor potential V channels are essential for glucose sensing by aldolase and AMPK. Cell Metab. 30, 508–524.e12 (2019).
Zsombok, A. & Derbenev, A. V. TRP channels as therapeutic targets in diabetes and obesity. Pharmaceuticals 9, 50 (2016).
Ahn, J., Lee, H., Im, S. W., Jung, C. H. & Ha, T. Y. Allyl isothiocyanate ameliorates insulin resistance through the regulation of mitochondrial function. J. Nutr. Biochem. 25, 1026–1034 (2014).
Lee, E. et al. Transient receptor potential vanilloid type-1 channel regulates diet-induced obesity, insulin resistance, and leptin resistance. FASEB J. 29, 3182–3192 (2015).
Jönsson, T. J., Schäfer, H.-L., Herling, A. W. & Brönstrup, M. A metabolome-wide characterization of the diabetic phenotype in ZDF rats and its reversal by pioglitazone. PLoS ONE 13, e0207210 (2018).
Ashburner, M. et al. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat. Genet. 25, 25–29 (2000).
Mi, H., Muruganujan, A., Ebert, D., Huang, X. & Thomas, P. D. PANTHER version 14: more genomes, a new PANTHER GO-slim and improvements in enrichment analysis tools. Nucleic Acids Res. 47, D419–D426 (2019).
Li, B. & Dewey, C. N. RSEM: accurate transcript quantification from RNA-seq data with or without a reference genome. BMC Bioinformatics 12, 323 (2011).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005).
Kalsbeek, A., la Fleur, S. & Fliers, E. Circadian control of glucose metabolism. Mol. Metab. 3, 372–383 (2014).
Kettner, N. et al. Circadian dysfunction induces leptin resistance in mice. Cell Metab. https://doi.org/10.1016/j.cmet.2015.06.005 (2015).
Li, A.-J. et al. Leptin-sensitive neurons in the arcuate nuclei contribute to endogenous feeding rhythms. Am. J. Physiol. Regul. Integr. Comp. Physiol. 302, R1313–R1326 (2012).
Wiater, M. F. et al. Circadian integration of sleep-wake and feeding requires NPY receptor-expressing neurons in the mediobasal hypothalamus. Am. J. Physiol. Regul. Integr. Comp. Physiol. 301, R1569–R1583 (2011).
Khan, S., Duan, P., Yao, L. & Hou, H. Shiftwork-mediated disruptions of circadian rhythms and sleep homeostasis cause serious health problems. Int. J. Genomics 2018, 8576890 (2018).
Park, S.-J. et al. DNA-PK promotes the mitochondrial, metabolic, and physical decline that occurs during aging. Cell Metab. 25, 1135–1146.e7 (2017).
Hvid, H. et al. Diabetic phenotype in the small intestine of zucker diabetic fatty rats. Digestion 94, 199–214 (2016).
Kakimoto, P. A. & Kowaltowski, A. J. Effects of high fat diets on rodent liver bioenergetics and oxidative imbalance. Redox Biol. 8, 216–225 (2016).
Karanth, S. et al. FOXN3 controls liver glucose metabolism by regulating gluconeogenic substrate selection. Physiol. Rep. 7, e14238 (2019).
Mullins, G. R. et al. Catecholamine-induced lipolysis causes mTOR complex dissociation and inhibits glucose uptake in adipocytes. Proc. Natl Acad. Sci. USA 111, 17450–17455 (2014).
Dungan, K. 1,5-Anhydroglucitol (GlycoMark) as a marker of short-term glycemic control and glycemic excursions. Expert Rev. Mol. Diagn. 8, 9–19 (2008).
Prawitt, J., Caron, S. & Staels, B. Bile acid metabolism and the pathogenesis of type 2 diabetes. Curr. Diab. Rep. 11, 160–166 (2011).
Bergman, B. C. et al. Serum sphingolipids: relationships to insulin sensitivity and changes with exercise in humans. Am. J. Physiol. Metab. 309, E398–E408 (2015).
Michalczyk, A., Dołęgowska, B., Heryć, R., Chlubek, D. & Safranow, K. Associations between plasma lysophospholipids concentrations, chronic kidney disease and the type of renal replacement therapy. Lipids Health Dis. 18, 85 (2019).
Sandoval, D. A., Obici, S. & Seeley, R. J. Targeting the CNS to treat type 2 diabetes. Nat. Rev. Drug Discov. 8, 386–398 (2009).
Rykkje, A., Carlsen, J. F. & Nielsen, M. B. Hand-held ultrasound devices compared with high-end ultrasound systems: a systematic review. Diagnostics 9, 61 (2019).
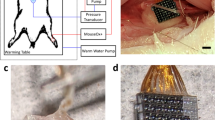
Pashaei, V. et al. Flexible body-conformal ultrasound patches for image-guided neuromodulation. IEEE Trans. Biomed. Circuits Syst. 14, 305–318 (2020).
Al-Battal, A. F. et al. A CNN segmentation-based approach to object detection and tracking in ultrasound scans with application to the vagus nerve detection. Preprint at https://doi.org/10.48550/arXiv.2106.13849 (2021).
Scarlett, J. M. et al. Central injection of fibroblast growth factor 1 induces sustained remission of diabetic hyperglycemia in rodents. Nat. Med. 22, 800–806 (2016).
Scarlett, J. M. et al. Peripheral mechanisms mediating the sustained antidiabetic action of fgf1 in the brain. Diabetes 68, 654–664 (2019).
Kuhre, R. E. et al. Bile acids are important direct and indirect regulators of the secretion of appetite- and metabolism-regulating hormones from the gut and pancreas. Mol. Metab. 11, 84–95 (2018).
Kraft, G. et al. Sympathetic denervation of the common hepatic artery lessens glucose intolerance in the fat- and fructose-fed dog. Diabetes 68, 1143–1155 (2019).
Shimizu, N., Oomura, Y., Novin, D., Grijalva, C. V. & Cooper, P. H. Functional correlations between lateral hypothalamic glucose-sensitive neurons and hepatic portal glucose-sensitive units in rat. Brain Res. 265, 49–54 (1983).
Jensen, J. F. I. E. L. D. A program for simulating ultrasound systems. Med. Biol. Eng. Comput. 34, 351–352 (1996).
Jensen, J. A. & Svendsen, N. B. Calculation of pressure fields from arbitrarily shaped, apodized, and excited ultrasound transducers. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 39, 262–267 (1992).
Nykonenko, A., Vávra, P. & Zonča, P. Anatomic peculiarities of pig and human liver. Exp. Clin. Transplant. 15, 21–26 (2017).
Morley, L. A., Gomez, T. H., Goldman, J. L., Flores, R. & Robinson, M. A. Accuracy of 5 point-of-care glucometers in C57BL/6J mice. J. Am. Assoc. Lab. Anim. Sci. 57, 44–50 (2018).
Mlinar, B., Marc, J., Janež, A. & Pfeifer, M. Molecular mechanisms of insulin resistance and associated diseases. Clin. Chim. Acta 375, 20–35 (2007).
DeFronzo, R. A., Tobin, J. D. & Andres, R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am. J. Physiol. 237, E214 (1979).
O’Connor, K. A. et al. Effect of diazepam and yohimbine on neuronal activity in sham and hemiparkinsonian rats. Neuroscience 351, 71–83 (2017).
Sutton, A. C., O’Connor, K. A., Pilitsis, J. G. & Shin, D. S. Stimulation of the subthalamic nucleus engages the cerebellum for motor function in parkinsonian rats. Brain Struct. Funct. 220, 3595–3609 (2015).
Sutton, A. C. et al. Deep brain stimulation of the substantia nigra pars reticulata improves forelimb akinesia in the hemiparkinsonian rat. J. Neurophysiol. 109, 363–374 (2012).
Gee, L. E., Walling, I., Ramirez-Zamora, A., Shin, D. S. & Pilitsis, J. G. Subthalamic deep brain stimulation alters neuronal firing in canonical pain nuclei in a 6-hydroxydopamine lesioned rat model of Parkinson’s disease. Exp. Neurol. 283, 298–307 (2016).
Paxinos, G. & Watson, C. The Rat Brain in Stereotaxic Coordinates (Academic Press, 1982).
Quiroga, R. Q., Nadasdy, Z. & Ben-Shaul, Y. Unsupervised spike detection and sorting with wavelets and superparamagnetic clustering. Neural Comput. 16, 1661–1687 (2004).
Gennisson, J.-L., Deffieux, T., Fink, M. & Tanter, M. Ultrasound elastography: principles and techniques. Diagn. Interv. Imaging 94, 487–495 (2013).
Sandrin, L. et al. Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med. Biol. 29, 1705–1713 (2003).
Griffin, D. R., Weaver, W. M., Scumpia, P. O., Di Carlo, D. & Segura, T. Accelerated wound healing by injectable microporous gel scaffolds assembled from annealed building blocks. Nat. Mater. 14, 737–744 (2015).
Metabolon Reporting and Interpretation (Metabolon, 2021); https://www.metabolon.com/solutions/reporting-interpretation/
Roswell Park Cancer Center - Shared Genomics Resource (Roswell Park Cancer Center, 2021); https://www.roswellpark.org/shared-resources/genomics
Andrews, S. FastQC: A Quality Control Tool for High Throughput Sequence Data http://www.bioinformatics.babraham.ac.uk/projects/fastqc (2010)
Dobin, A. & Gingeras, T. R. Mapping RNA-seq reads with STAR. Curr. Protoc. Bioinformatics 51, 11.14.1–11.14.19 (2015).
Liberzon, A. et al. The molecular signatures database hallmark gene set collection. Cell Syst. 1, 417–425 (2015).
Flannick, J. et al. Exome sequencing of 20,791 cases of type 2 diabetes and 24,440 controls. Nature 570, 71–76 (2019).
Li, M. J. et al. GWASdb: a database for human genetic variants identified by genome-wide association studies. Nucleic Acids Res. 40, D1047–D1054 (2012).
Rouillard, A. D. et al. The harmonizome: a collection of processed datasets gathered to serve and mine knowledge about genes and proteins. Database 2016, baw100 (2016).
Ruud, J., Steculorum, S. M. & Brüning, J. C. Neuronal control of peripheral insulin sensitivity and glucose metabolism. Nat. Commun. 8, 15259 (2017).
Myers, M. G. J. & Olson, D. P. Central nervous system control of metabolism. Nature 491, 357–363 (2012).
Acknowledgements
We thank G. Petter Fosse (University Hospital of Northern Norway) for helpful discussions on large-animal experiments. Experiments in this study were partially funded with Federal funds from the Defense Advanced Research Project Agency (United States Department of Defense; DARPA DoD; DARPA HR0011-18-C-0040). R.I.H. was supported by the NIH via UL1 TR001863; P30 DK045735; R01 DK101984; R01 DK020495; and DARPA 401126008. The views, opinions and/or findings expressed herein are those of the authors and should not be interpreted as representing the official views or policies of the Department of Defense or the US Government.
Author information
Authors and Affiliations
Contributions
V.C. performed chronic stimulation experiments in ZDF and DIO models, data analysis and short-term stimulation experiments involving chemical lesioning and in vivo blocking; H.M. performed the in vitro stimulation experiments and data analysis; Z.H., K.A., M.D., L.B. and T.M. performed in vivo electrical recording experiments and contributed to data analysis; K.Q., J.N.T. and W.S. performed swine model experiments and data analysis; T.S.H., A.D. and T.T. performed western diet model experiments; N.T., Y.D. and K.J.-C. performed rodent H/E clamp experiments; J.G. performed transcriptomic and metabolomic analyses, data presentation and statistical analysis across manuscript data; R.M. performed analysis of electrical nerve recording data; K.W., T.-J.K. and Y.F. installed, set-up and calibrated ultrasound equipment and contributed experimental results from the mechanical piston stimulation data; E.L. and C.M. assisted in sample collection, storage and analysis of DIO and ZDF biological samples; J.A., K.J.T., T.R.C., D.D.C., D.S., S.Z., S.S.C., R.I.H. and C.P. designed the research and experiments, performed data analysis, edited and co-wrote sections of the manuscript; C.P. wrote the manuscript, including the assembly of sections from the collaborating institutions.
Corresponding author
Ethics declarations
Competing interests
V.C., J.G., R.M., K.W., E.L., C.M., Y.F., T.-J.K., J.A. and C.P. are employees of General Electric and declare that GE has filed US and international patent applications describing methods, devices and systems for precision organ-based ultrasound neuromodulation. H.M., Z.H., K.Q., T.S.H., N.T., Y.D., K.J.-C., J.-N.T., A.D., T.T., K.A., M.D., L.B., T.M., K.J.T., T.R.C., D.D.C., D.S., S.Z., S.S.C. and R.I.H. have received research funding from GE to investigate the effects of ultrasound on metabolism. W.S. declares no competing interests.
Peer review
Peer review information
Nature Biomedical Engineering thanks Gin-Shin Chen, Harald Stauss and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Hepatic pFUS attenuates hyperglycemia in mice.
a. Hepatic pFUS attenuates hyperglycemia in western diet-fed mice. Blood glucose levels were measured at week 9 (white plots), prior to the stimulation period and week 16 (grey plots), post-stimulation period. Daily stimulated western diet-fed mice had significantly reduced blood glucose levels across the stimulation period (WD–pFUS, week 9 vs week 16; p-values shown are derived using nonparametric Wilcoxon rank-sum test and corrected using the Bonferroni method (n = 14 per group; Box plot presents the data median, first and third quartiles and the whiskers are the 1.5 x range (IQR). If no points exceed 1.5 x IQR distance, then the whiskers are simply the minimum and maximum values). b. Hepatic pFUS attenuates hyperinsulinemia in western diet-fed mice. Insulin levels were measured at week 9 (white plots), prior to the stimulation period, and at week 16 (grey plots), post-stimulation period. WD–pFUS mice had significantly reduced insulin levels across the stimulation period (WD–pFUS, week 9 vs week 16, p-values shown are derived using nonparametric Wilcoxon rank-sum test (two-sided) and corrected using the Bonferroni method (n = 10 per group; Box plot presents the data quartiles and whiskers are the minimum and maximum values unless value exceeds the 1.5 x IQR distance).
Extended Data Fig. 2 Effect of pulsed focused ultrasound (pFUS) of the porta hepatis on insulin sensitivity in STZ-induced diabetic diet-induced obesity (DIO) rats, as quantified through hyperinsulinemic-euglycemic clamp121 (HEC).
a) Timeline of experimental interventions. Glucose infusion rate (GIR) during standardized hyperinsulinemic clamp (glucose values shown in b; n = 7)) revealing higher steady state glucose infusion requirement after pFUS treatment and c) glucose infusion rate area under the curve (AUC) for steady state (n = 7; Box plot presents the data median, first and third quartiles and the whiskers are the 1.5 x range (IQR). If no points exceed 1.5 x IQR distance, then the whiskers are simply the minimum and maximum values). Plasma hormone change during the clamp including d) glucagon e) epinephrine, f) norepinephrine and g) corticosterone. Values are mean ± SEM; p-values from 2-way ANOVA (GIR); multiple t-tests (hormones); or Wilcoxon rank sum (AUC); n = 6 per measurement for D-G.
Extended Data Fig. 3 Effect of pulsed focused ultrasound (pFUS) of the porta hepatis on insulin sensitivity in STZ-induced T1D rats, as quantified through hyperinsulinemic-euglycemic clamp121 (HEC).
a) Timeline of experimental interventions (see material and methods for experimental description). Glucose infusion rate (GIR) during standardized hyperinsulinemic clamp (glucose values shown in b; n = 6)) revealing higher steady state glucose infusion requirement after pFUS treatment and c) glucose infusion rate area under the curve (AUC) for steady state (n = 6; Box plot presents the data median, first and third quartiles and the whiskers are the 1.5 x range (IQR). If no points exceed 1.5 x IQR distance, then the whiskers are simply the minimum and maximum values). Plasma hormone change during the clamp including d) glucagon, e) epinephrine, f) norepinephrine and g) corticosterone. Values are mean ± SEM.; p-values from 2-way ANOVA (GIR); multiple t-tests (hormones); or Wilcoxon rank sum (AUC); n = 5 per measurement for D-G.
Extended Data Fig. 4 Short-term effect of focused ultrasound (pFUS) of the porta hepatis on insulin sensitivity in healthy swine, as quantified through hyperinsulinemic-euglycmic clamp (HEC).
a. Representative data from an HEC experiment. Under continuous, constant infusion of insulin at a rate of 0.5 mU/kg/min, glucose infusion rate (GIR) was adjusted every 5 minutes according to a formula121 to achieve euglycemia (defined as baseline glucose concentration ±10%) and maintained for ≥ 30 min (grey shaded area). In this example, GIR at euglycemic equilibrium was 3.5 mg/kg/min. The quality of the HEC was assessed by calculating the normalized coefficient of variation (CV) of the glucose concentration and GIR for the duration of euglycemic equilibrium. In this experiment, CV for glucose was 6.92% and for GIR was 6.51%. b. In step-clamp experiments, euglycemic equilibrium GIR values were calculated for different insulin infusion rates (IIR) in 2 animals. Based on this data, we decided to conduct pFUS experiments at IIR of 0.5 mU/kg/min, as the slope of the GIR curves, and therefore the sensitivity of the method to resolve changes in insulin sensitivity, decreased at higher IIRs. c. Example of a pFUS experiment, after establishing HEC (CV for glucose 2.85%, for GIR 0%). pFUS of the porta hepatis was applied for 4 minutes (blue shaded area), after which GIR was adjusted, just like before, to maintain euglycemia. Increase in GIR after pFUS reflects increased insulin sensitivity. d. Imaging of the porta hepatis in swine. Left: Noninvasive imaging (probe placed on skin). Right: Invasive imaging (probe placed on top of PH after it was surgically accessed). e. Example of a sham-stimulation experiment in an animal that previously underwent pFUS stimulation. In the sham-stimulation experiment, once HEC was established, the US probe was operated in imaging mode (with ultrasound power off). In the pFUS experiment (results previously shown in Fig. 3) performed in the same animal 3 days later, HEC was established like before and noninvasive pFUS stimulation was delivered. See Methods for experimental descriptions.
Extended Data Fig. 5 Histochemical analysis of hypothalamic neural pathways associated with response to pFUS after 20 days of daily stimulation in the ZDF model.
a. cFOS immunohistochemistry images show the number of activated neurons in unstimulated (left) versus pFUS stimulated (right) animals. Images were segmented on the paraventricular nucleus (PVN; green), dorsal medial nucleus (DMN; yellow), ventromedial nucleus (VMN; red), arcuate nucleus (ARC; blue), and lateral hypothalamus (LH; purple) Scale bar = 200 microns. b. Data showing the percent change in the number of cFos expressing cells with pFUS compared to sham controls in each segmented hypothalamic region (PVN, DMN, VMN, ARC, LH), images shown represent one set of sham versus stimulated paired (n = 3; data shown as mean ± s.e.). c. Histochemical analysis of paraffin-embedded rat brain tissue labeling BDNF antibody showing the unstimulated control (left) and pFUS stimulated animals (right). As observed an increase in BDNF staining was visible in the hypothalamus (with prominence in the arcuate and ventromedial hypothalamus), thalamic and hippocampal brain regions. Images are included as partial coronal sections to demonstrate total BDNF activation by pFUS across a number of brain regions. d. Histochemical analysis of paraffin embedded rat brain tissue labeling GLUT-4 receptor antibody showing hypothalamic (left) and hippocampal (right) staining patterns. As observed an increase in both hypothalamic and hippocampal GLUT-4 translocation occurred following hepatic pFUS (right) as compared to unstimulated sham controls (left).
Supplementary information
Supplementary Information
Supplementary figures, tables and references.
Source data
SD for Fig. 1
Source data.
SD for Fig. 2
Source data.
SD for Fig. 3
Source data.
SD for Fig. 4
Source data.
SD for Fig. 5
Source data.
SD for Fig. 6
Source data.
SD for Fig. 7
Source data.
SD for Fig. 8
Source data.
SD for ED Fig. 1
Source data.
SD for ED Fig. 2
Source data.
SD for ED Fig. 3
Source data.
SD for ED Fig. 4
Source data.
SD for ED Fig. 5
Source data.
Rights and permissions
About this article
Cite this article
Cotero, V., Graf, J., Miwa, H. et al. Stimulation of the hepatoportal nerve plexus with focused ultrasound restores glucose homoeostasis in diabetic mice, rats and swine. Nat. Biomed. Eng 6, 683–705 (2022). https://doi.org/10.1038/s41551-022-00870-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-022-00870-w
This article is cited by
-
Functional nanoparticle-enabled non-genetic neuromodulation
Journal of Nanobiotechnology (2023)
-
Rib detection using pitch-catch ultrasound and classification algorithms for a novel ultrasound therapy device
Bioelectronic Medicine (2023)
-
Magneto-mechanical effect of magnetic microhydrogel for improvement of magnetic neuro-stimulation
Nano Research (2023)
-
Strategies for precision vagus neuromodulation
Bioelectronic Medicine (2022)
-
Wireless neuromodulation with porous silicon
Nature Materials (2022)