Abstract
Schizophrenia has been linked to polymorphism in genes encoding components of the complement system, and hyperactive complement activity has been linked to immune dysfunction in schizophrenia patients. Whether and how specific complement components influence brain structure and cognition in the disease is unclear. Here we compared 52 drug-naïve patients with first-episode schizophrenia and 52 healthy controls in terms of levels of peripheral complement factors, cortical thickness (CT), logical memory and psychotic symptoms. We also explored the relationship between complement factors with CT, cognition and psychotic symptoms. Patients showed significantly higher levels of C1q, C4, factor B, factor H, and properdin in plasma. Among patients, higher levels of C3 in plasma were associated with worse memory recall, while higher levels of C4, factor B and factor H were associated with thinner sensory cortex. These findings link dysregulation of specific complement components to abnormal brain structure and cognition in schizophrenia.
Similar content being viewed by others
Background
Schizophrenia is a severe psychiatric disorder that affects approximately 1% of the global population1, impairing their social function and shortening life expectancy2. The disease appears to have genetic and environmental causes3,4,5,6. Polymorphism in the gene encoding C4 in the complement system has been linked to risk of schizophrenia7, and excessive complement activity has been linked to immune dysfunction that may contribute to the disease8. In addition, a single-nucleotide polymorphism in the gene encoding CSMD1, which degrades the complement components C3 and C49, has been strongly associated with risk of the disease10.
Post-mortem analysis of brains from individuals with schizophrenia has revealed increased C4 expression in hippocampal subfields, para-hippocampal gyrus, insula entorhinal, medial orbitofrontal cortex, and posterior cingulate7,11. Consistently, the same regions show cortical thinning in studies of brains from living individuals with schizophrenia7,11,12,13. In addition, C4 overexpression in mice reduces the density of cortical synapses, increases microglial engulfment of synapses, and induces behavioral deficits14. The complement system as a whole promotes synaptic pruning11 and neuronal migration during development15, so it is tempting to speculate that hyperactive complement activity may lead to excessive synaptic pruning and other neuropathology that contribute to schizophrenia11,16.
Consistent with this hypothesis, C4 overexpression has been linked to worse memory in individuals with schizophrenia as well as in healthy controls17, and with more severe delusional symptoms in the disease18. C3 overexpression has been linked to memory loss and brain volume reduction in multiple sclerosis19, and polymorphism in genes encoding complement components other than C4 has been linked to worse memory in individuals with psychosis as well as in healthy controls20.
While substantial evidence links overexpression of C4 and C3 to greater risk or severity of schizophrenia and associated neuropathology, some studies have failed to detect elevated levels of either complement component in the plasma of affected individuals21,22,23. In addition, few studies have examined whether levels of other complement components are elevated in affected individuals24, which is an important question to address given that complement responses can proceed not only via the “classical” and “lectin” pathways involving C425, but also via the “alternative” pathway involving factor B, factor H and properdin26,27.
Here we systematically compared the levels of numerous key complement components in plasma between individuals with schizophrenia and healthy controls. We recruited only drug-naïve individuals who had experienced their first schizophrenic episode, allowing us to exclude potential confounding due to antipsychotic drug use and episode of disease28. We also explored potential associations of complement levels with memory, cortical thickness, and psychotic symptoms.
Methods
Participants
The study procedure was approved by the Ethics Committee of West China Hospital, Sichuan University. All participants were recruited between March 2014 and February 2019 from in- and outpatient psychiatric facilities at West China Hospital of Sichuan University. Individuals with schizophrenia were enrolled if they had experienced their first episode as determined by two experienced psychiatrists based on the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders and the Structured Clinical Interview for DSM-IV Disorders29. Symptom severity was measured using the Positive and Negative Symptom Rating Scale30. We excluded individuals who had ever taken antipsychotic drugs for more than three days, met the criteria for alcohol or substance abuse within one year prior to their screening for this study, reported a history of any significant medical illness, or had contraindications to magnetic resonance imaging (MRI). Healthy controls were screened for major psychiatric disorders using the “non-patient” version of the Structured Clinical Interview for DSM-IV Disorders. None reported being on psychotropic medication. All participants were right-handed, and all provided written informed consent before enrollment.
Logical memory recall
Immediate and delayed logical memory recall were assessed using the Chinese version of the short form of the revised Wechsler Adult Intelligence Scale31 containing the following seven subtests: information, arithmetic, digital symbol, digital span test, block design, picture completion, and similarities. Scores for immediate and delayed logical memory recall ranged from 0 to 25, with higher scores indicating greater recall32. The intelligence quotient (IQ), verbal IQ (VIQ) and performance IQ (PIQ) were also measured. The Supplementary Methods contain additional details about cognitive assessment.
Cortical thickness by MRI
All participants underwent MRI scanning on a 3.0-T Achieva system (Philips, Amsterdam, The Netherlands) equipped with an eight-channel phased-array head coil. To minimize head movement and scanner noise, foam padding and earplugs were used. High-resolution T1 images were acquired using a 3D magnetization-prepared rapid gradient-echo sequence with the following parameters: repetition time, 8.37 ms; echo time, 3.88 ms; flip angle, 7°; in-plane matrix resolution, 256 × 256; field of view, 24 × 24 cm2; and number of slices, 188. T1-weighted MRI scans from all participants were processed using the standardized pipeline of CAT12 and smoothed using a Gaussian kernel with full-width at half-maximum of 12 mm, generating brain maps of cortical thickness.
Levels of complement components in plasma
The concentrations of complement components in plasma were assayed as described33. Briefly, blood samples were collected via venipuncture at 4.00–4.30 p.m. into tubes containing ethylenediaminetetraacetic acid. Blood was centrifuged at 1000 g for 10 min at 4 °C to remove peripheral blood mononuclear cells, and the plasma was immediately divided into 0.5-mL aliquots and stored at −80 °C. Plasma factors were assayed using MILLIPLEX® MAP kits (Merck, Darmstadt, Germany), while the complement components C1q, C3, C3b/iC3b, C4, factor B, properdin, and factor H were assayed using the Human Complement Panel 2-Immunology Multiplex Assay (catalog no. HCMP2MAG-19K, Merck Millipore, Billerica, MA, USA). Kits were used according to the manufacturer’s instructions, and data were analyzed using a FLEXMAP 3D® instrument (Luminex, Merck Millipore) and xPONENT® 4.0 software (Luminex). Standard curves were generated using the standards in the kit. Median fluorescence intensity was converted into concentrations using a weighted 5-parameter logistic method. Supplementary Figs. 1–2 show additional details of complement assay in plasma.
Statistical analysis
All analyses were performed using SPSS 24.0 (SPSS, Chicago, IL, USA) and STATA 14.0 (Stata Corporation, College Station, Texas, USA). Differences between individuals with schizophrenia and healthy controls in continuous demographic variables were assessed for significance using a two-sample t test, while differences in categorical variables were assessed using a chi-squared test. Normal distribution of all variables was verified using the Shapiro-Wilk test. Scores for immediate or delayed logic memory recall were compared between individuals with schizophrenia and healthy controls using analysis of covariance that took into account age, sex, and education level based on Bonferroni correction. Concentrations of complement components were log10-transformed to normalize their distributions, then compared between individuals with schizophrenia and healthy controls while controlling for age, sex, and body mass index.
Vertex-wise cortical thickness was compared between individuals with schizophrenia and healthy controls using a two-sample t test in which we controlled for age, sex, education level and total intracranial volume. Potential associations of cortical thickness with levels of complement components were explored separately among individuals with schizophrenia, among healthy controls, and among all participants in regression that controlled for age, sex, education level, body mass index and total intracranial volume34,35. Stepwise multiple linear regressions were performed between logical memory recall and complement components among individuals with schizophrenia, among healthy controls, and among all participants. Before regression, we used the “least absolute shrinkage and selection operator” (LASSO) in STATA36 to select the complement factors that were associated with logical memory recall in order to avoid multicollinearity: levels of complement components correlated strongly with one another, with correlation coefficients >0.7 (Supplementary Table 1). After LASSO selection, immediate logical memory recall across all participants was analyzed using stepwise multiple linear regression in which the independent variables were age, sex, education, body mass index, and log10-transformed concentrations of C4 and factor H. Delayed logical memory recall across all individuals with schizophrenia was analyzed in stepwise multiple linear regression in which the independent variables were age, education, body mass index, and log10-transformed concentrations of C1q, C3, C4, and properdin. Insignificant variables were removed sequentially until only significant ones remained. Potential associations of cortical thickness with logical memory recall were explored to determine whether brain cortical thickness associated with complement factors could potentially mediate the relationship between plasma complement components and logical memory; this analysis controlled for age, sex, education level, and body mass index. In addition, partial correlation analysis was used to evaluate the correlation between plasma complement measurements and clinical parameters after controlling for age, sex, education level, and body mass index. Significance was defined as p < 0.05. During analysis of MRI images, significance was defined as vertex-wise p < 0.001 after correction for family-wise error rate at the cluster level.
Results
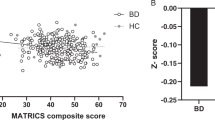
We screened 62 individuals with schizophrenia and 54 healthy controls who visited our in- or outpatient facilities during the enrollment period. In the end, we enrolled 52 drug-naïve individuals with first-episode schizophrenia (24 men) and 52 healthy controls (21 men) (Supplementary Fig. 3). Individuals with schizophrenia were younger than healthy controls and obtained lower verbal, performance and total IQ scores37. They also showed significantly worse immediate and delayed logical memory recall than controls, and they showed significantly higher levels of C1q, C4, factor B, factor H and properdin in plasma, but similar levels of C3 as controls (Table 1, Fig. 1).
Peripheral protein concentrations of complement components show significant increases in C1q, C4, factor B, factor H, and properdin in first-episode schizophrenia (FES) patients compared to controls. No difference was observed for C3. Bars represent the mean ± SD, and p-values are adjusted for age, sex, and body mass index (BMI). Abbreviations: FES: first episode schizophrenia; HC: healthy control; SD: standard deviation.
Associations between levels of complement components and memory recall
We examined potential associations between levels of complement factors and immediate logical memory scores across all study participants. In Step 1, education level significantly explained the variance in scores (F = 10.86, p < 0.01; R2 = 0.10; β = 0.39), which did not change in Step 2 after inclusion of C4 concentration (F = 8.10, p < 0.05; R2 = 0.15; β = −7.94; Table 2, Supplementary Table 2). Our results indicate that higher levels of C4 were associated with worse scores for immediate logical memory recall.
Similarly, we examined potential associations between levels of complement factors and delayed logical memory scores across individuals with schizophrenia but not in healthy controls. We found that higher C3 concentration was associated with worse scores for delayed logical memory recall (Table 3, Supplementary Table 2).
Associations between levels of complement components and cortical thickness
Among individuals with schizophrenia, thickness of the left primary sensory cortex was inversely associated with levels of C4, factor B, and factor H after controlling for age, sex, education level, body mass index, and total intracranial volume (Fig. 2a–c). Among healthy controls, thickness of the left dorsolateral prefrontal cortex was positively associated with levels of C1q, C3 and C4 after controlling for age, sex, education level, body mass index, and total intracranial volume (Fig. 2d–f).
a–c Linear regression analyses (adjusting for age, sex, education years, BMI and TIV) in FES revealed a significant negative correlation between the complement component 4, factor B and factor H with individual frontal thickness regions that made up the left primary sensorimotor cortex (PSC). The peak Montreal Neurological Institute (MNI) coordinates of left PSC associated with C4 is X = −57/−60, Y = −18/−14, Z = 32/39, t = −4.02/−4.01, cluster size = 121, corrected p < 0.01; factor B is X = −57/−60, Y = −18/−14, Z = 31/39, t = −4.14/−3.98, cluster size = 103, corrected p < 0.01; factor H is X = −57/−60, Y = −18/−14, Z = 32/39, t = −4.21/−3.87, cluster size = 103, corrected p < 0.01. Blue-colored regions (in dark circle) show areas with a significantly negative correlation of CT with complement factors in participants with FES (cluster p < 0.05, FWE corrected; vertex level puncorrected < 0.001). No significant positive correlations were detected in FES patients. d–f Linear regression analyses (adjusting for age, gender, education years, BMI and TIV) in healthy controls revealed a significant positive correlation between the plasma complement C1q, complement component 4, and complement component 3 with the left dorsal lateral prefrontal cortex (DLPFC). The peak MNI coordinates of left DLPFC associated withC1q is X = −23/−21, Y = 27/10, Z = 54/50, t = 4.42/4.34, cluster size = 132, corrected p < 0.01; C3 is X = −34/−22/−20, Y = 31/43/29, Z = 38/34/40, t = 5.31/4.69/3.82, corrected p < 0.001; C4 is X = −20/−23/−20,Y = 41/17/30, Z = 34/43/38, t = −4.01/3.56/3.42, cluster size = 100, corrected p < 0.05. Red-colored region (in the white circle) shows the area with a significantly positive correlation of CT with complement factors in control participants (cluster p < 0.05, FWE corrected; vertex level puncorrected < 0.001). No significant negative correlations were detected in the controls. Abbreviations: FES first episode schizophrenia, BMI body mass index, TIV total intracranial volume, PSC primary sensory cortex, CT cortical thickness, DLPFC dorsolateral prefrontal cortex, FWE family wise error.
When we analyzed individuals with schizophrenia and healthy controls together, we did not detect any significant relationships between the level of any complement component and thickness of any cortical brain region. We did not observe any significant association between cortical thickness and either immediate or delayed logical memory recall among individuals with schizophrenia, among healthy controls or among all subjects together after controlling for age, sex, education level, body mass index, and total intracranial volume. Our results suggest that variations in cortical thickness in our sample did not contribute to the association between levels of complement factors and logical memory recall.
Associations between levels of complement components and psychotic symptoms
Among individuals with schizophrenia, we did not observe any significant correlations between levels of complement components and illness duration or total score or sub-scale scores on the Positive and Negative Symptom Rating Scale after controlling for age, sex, education level and body mass index (Supplementary Table 3).
Discussion
Our controlled analysis of drug-naïve individuals with first-episode schizophrenia suggests hyperactivation of all three complement cascades in the disease and links such hyperactivation to thinning of the primary sensory cortex in affected individuals. It also links such hyperactivation to impairment of logical memory in affected and healthy individuals, consistent with a study involving individuals with psychosis and healthy controls17. In the present work, levels of different complement components showed different relationships to cortical thickness in the brain depending on whether schizophrenia was present or not: in affected individuals, higher levels of C4, factor B and factor H were associated with thinner primary sensory cortex; in healthy controls, higher levels of C1q, C4 and factor H were associated with thicker left dorsolateral prefrontal cortex. To our knowledge, this is the first report linking the complement cascade to abnormalities in the primary sensorimotor network.
Our findings of elevated levels of complement components in drug-naïve, first-episode schizophrenia are consistent with previous studies reporting upregulation of C47,11,14 and factor B38 in individuals with multi-episode schizophrenia, upregulation of C1q in individuals with first-episode schizophrenia39, increased activity of C1 in patients with multiple-episode schizophrenic in the acute stage of the disease40, and upregulation of factor H in the hippocampus of individuals with stable schizophrenia who had been ill for fewer than five years41. Thus, substantial evidence points to hyperactivation of the classical, lectin and alternative complement pathways in schizophrenia. This is a key contribution of our study given that components of the alternative pathway, such as factor B, factor H and properdin, have not been extensively explored in schizophrenia.
Our findings contrast with studies reporting normal activation of the lectin complement pathway in multiple-episode, drug-treated schizophrenia42 or normal levels of properdin in individuals with first-episode psychosis28. We consider that our results may be more reliable because we eliminated confounding due to medication, disease episode and factors known to influence complement levels such as body mass index and smoking status43. Our work suggests that previously reported associations between complement hyperactivation and multi-episode schizophrenia also apply to drug-naïve, first-episode disease.
Our work also strengthens the idea that complement hyperactivation contributes to immune dysregulation in the condition11. Indeed, the genomic region most strongly associated with schizophrenia risk contains genes of the major histocompatibility complex as well as the gene encoding C444, and this genomic region has been implicated in various autoimmune diseases11. Prenatal exposure to maternal immune activation in mice has been linked to disruption of cytoarchitecture in the primary somatosensory cortex45; such disruption, together with brain activation, may help explain the abnormal behavior of mouse models of autism and other neurodevelopmental disorders. The disrupted cortical cytoarchitecture in that previous work is reminiscent of our present finding of cortical thinning in the primary sensory cortex of individuals with schizophrenia.
Despite the strong evidence for hyperactivation of the classical complement pathway in schizophrenia, levels of C3 were not significantly higher in our individuals with schizophrenia than in healthy controls, which is consistent with a meta-analysis comparing individuals with schizophrenia and controls24 and with a study of individuals with first-episode psychosis43. In contrast, another study reported higher levels of C3 in chronic schizophrenia patients than in healthy controls11,46. One potential explanation for these discrepant reports is that C3 is not related to risk of schizophrenia in Han Chinese, among whom individuals with schizophrenia and healthy controls do not appear to differ significantly in frequencies of polymorphisms in the gene encoding C3 or in plasma levels of C347.
The aforementioned study of individuals with first-episode psychosis28,43 found no significant abnormality in levels of C1q or C4, both of which were elevated in our participants with schizophrenia. This difference may reflect that many subjects in the psychosis study did not have schizophrenia or were taking medication, and we cannot exclude the influence of differences in smoking status, ethnicity or body mass index43. Our analysis links upregulation of C3 and C4 to worse logical memory recall not only in individuals with first-episode schizophrenia but also in healthy controls, consistent with studies involving healthy individuals17,48 or those with multiple sclerosis or stroke17,19,49. A possible explanation for these findings is that complement proteins, especially C4, aid in synaptic pruning14,50 and that excessive pruning can lead to synaptic loss like that observed in schizophrenia51. C3 hyperactivity in a mouse model of autoimmune encephalomyelitis has been linked to early dendritic loss and microglia-mediated phagocytosis of synapses in the hippocampus, and inhibiting C3 in these animals mitigates memory impairment19. Our work supports the idea that inhibiting complement pathways may ameliorate memory deficits in schizophrenia17 and other neurological disorders52,53.
On the other hand, our work does not shed light on whether and how the logical memory defect in our individuals with schizophrenia may be related to their cortical thinning. Similarly, a study of individuals with psychosis failed to find an association between cognitive function (including digital number memory) and brain cortical thickness54. Further work is needed to clarify whether and how complement levels influence brain structure, and whether and how the altered structure affects cognitive function. Assuming that the elevated complement levels in our individuals with schizophrenia contribute to the observed cortical thinning, we suggest that complement hyperactivation is a chronic, not acute, feature of the disease, given that neuroanatomical changes take time to appear11.
Our work failed to find significant associations between levels of complement components and severity of schizophrenia symptoms measured on the Positive and Negative Symptom Rating Scale. A previous study also found no significant association of levels of C3 or C4 with scores on the same scale among individuals with multiple-episode, drug-treated schizophrenia55,56, while an analysis of 7000 children found no association between C4 expression and occurrence of psychotic experiences during childhood57. These negative findings highlight the complexity of elucidating whether and how the complement system contributes to the clinical manifestations of schizophrenia. Given that levels of interleukins 1β, 6 and 8 as well as tumor necrosis factor-α have been linked to psychotic symptoms in schizophrenia58, we recommend that future research explore whether and how not only complement components but also inflammatory markers—and perhaps their interactions with one another—influence onset and symptoms of schizophrenia.
Our finding of a positive association of levels of classical complement components C1q, C3 and C4 with thickness of the dorsolateral prefrontal cortex in healthy controls may reflect a normal function of the classical pathway in clearing away excess neurotransmitters, removing aged proteins, pruning synapses and modulating adult neurogenesis27,59. Higher levels of C4 have been linked to greater surface area and thickness of the insular and middle temporal cortices in healthy individuals12. Presumably, activation of complement pathways must be tightly regulated to prevent harmful excesses, similar to inflammatory and immune responses. Future research should elucidate the pathways that regulate complement activation and explain why they fail in schizophrenia.
Limitations
We did not genotype the study participants, which prevents us from determining to what extent the observed differences in expression of complement components is due to one or more genetic mutations11. The cross-sectional study design prevents us from establishing cause-effect relationships among complement levels, cortical thinning, and logical memory. Indeed, we failed to detect significant links between cortical thinning and worse logical memory. Clearly much more work is needed into whether and how complement pathways contribute to schizophrenia, preferably through large, longitudinal studies.
Conclusion
Our results strengthen the evidence for a role of the complement system in the pathophysiology of schizophrenia by linking hyperactivation of the classical, lectin and alternative pathways to deficits in logical memory and cortical thinning in the brain. At the same time, our work highlights many questions that remain to be resolved about the interplay of complement responses and neural processes in schizophrenia.
Availability of data and materials
The data in this study cannot be deposited in a public repository because of privacy regulations and the conditions of the informed consent provided by study participants. Instead, data in this study are available from the corresponding author on reasonable request.
Data availability
The statistical maps that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to them containing information that could compromise research participant privacy or consent. Explicit consent to deposit raw-imaging data was not obtained from the patients.
References
Laidi, C. et al. Factors associated with direct health care costs in schizophrenia: results from the FACE-SZ French dataset. Eur. Neuropsychopharmacol. 28, 24–36 (2018).
Charlson, F. J. et al. Global epidemiology and burden of Schizophrenia: findings from the global burden of disease study 2016. Schizophr. Bull. 44, 1195–1203 (2018).
Na, K.-S., Jung, H.-Y. & Kim, Y.-K. The role of pro-inflammatory cytokines in the neuroinflammation and neurogenesis of schizophrenia. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 48, 277–286 (2014).
Hilker, R. et al. Heritability of Schizophrenia and Schizophrenia spectrum based on the nationwide danish twin register. Biol. Psychiatry 83, 492–498 (2018).
Tsuang, M. Schizophrenia: genes and environment. Biol. Psychiatry 47, 210–220 (2000).
Stilo, S. A. & Murray, R. M. Non-genetic factors in Schizophrenia. Cur Psychiatry Rep. 21, 100 (2019).
Sekar, A. et al. Schizophrenia risk from complex variation of complement component 4. Nature 530, 177–183 (2016).
Chauhan, P., Kaur, G., Prasad, R. & Singh, H. Pharmacotherapy of schizophrenia: immunological aspects and potential role of immunotherapy. Expert Rev. Neurother. 21, 1441–1453 (2021).
Escudero-Esparza, A., Kalchishkova, N., Kurbasic, E., Jiang, W. G. & Blom, A. M. The novel complement inhibitor human CUB and Sushi multiple domains 1 (CSMD1) protein promotes factor I-mediated degradation of C4b and C3b and inhibits the membrane attack complex assembly. FASEB J. 27, 5083–5093 (2013).
Biological insights from 108 schizophrenia-associated genetic loci. Nature 511, 421-427 (2014).
Ji, E. et al. Peripheral complement is increased in schizophrenia and inversely related to cortical thickness. Brain Behav. Immun. 101, 423–434 (2022).
O’Connell, K. S. et al. Association between complement component 4A expression, cognitive performance and brain imaging measures in UK Biobank. Psychol. Med. 52, 1–11 (2021).
Qiu, A. et al. Hippocampal-cortical structural connectivity disruptions in schizophrenia: an integrated perspective from hippocampal shape, cortical thickness, and integrity of white matter bundles. NeuroImage 52, 1181–1189 (2010).
Yilmaz, M. et al. Overexpression of schizophrenia susceptibility factor human complement C4A promotes excessive synaptic loss and behavioral changes in mice. Nat. Neurosci. 24, 214–224 (2021).
Gorelik, A. et al. Developmental activities of the complement pathway in migrating neurons. Nat. Commun. 8, 15096 (2017).
Gallego, J. A., Blanco, E. A., Morell, C., Lencz, T. & Malhotra, A. K. Complement component C4 levels in the cerebrospinal fluid and plasma of patients with schizophrenia. Neuropsychopharmacology 46, 1140–1144 (2021).
Donohoe, G. et al. Genetically predicted complement component 4A expression: effects on memory function and middle temporal lobe activation. Psychol. Med. 48, 1608–1615 (2018).
Hatzimanolis, A. et al. Deregulation of complement components C4A and CSMD1 peripheral expression in first-episode psychosis and links to cognitive ability. Eur. Arch. Psychiatry Clin. Neurosci. 272, 1219–1228 (2022).
Bourel, J. et al. Complement C3 mediates early hippocampal neurodegeneration and memory impairment in experimental multiple sclerosis. Neurobiol. Dis. 160, 105533 (2021).
Holland, J. F. et al. Effects of complement gene-set polygenic risk score on brain volume and cortical measures in patients with psychotic disorders and healthy controls. Am. J. Med. Genet. Part B, Neuropsychiatr. Genet. 183, 445–453 (2020).
Ji, R. N. et al. Decreased serum complement component 4 levels in patients with schizophrenia. Psychiatr. Genet. 29, 127–129 (2019).
Su, J., Feng, X., Chen, K., Fang, Z. & Zhang, H. Plasma complement component 4 alterations in patients with schizophrenia before and after antipsychotic treatment. Asian J. Psychiatry 73, 103110 (2022).
Woo, J. J., Pouget, J. G., Zai, C. C. & Kennedy, J. L. The complement system in schizophrenia: where are we now and what’s next? Mol. Psychiatry 25, 114–130 (2020).
Mongan, D. et al. Peripheral complement proteins in schizophrenia: a systematic review and meta-analysis of serological studies. Schizophr. Res. 222, 58–72 (2020).
Rosbjerg, A. et al. Complementary roles of the classical and lectin complement pathways in the defense against aspergillus fumigatus. Front. Immunol. 7, 473 (2016).
Kouser, L. et al. Properdin and factor h: opposing players on the alternative complement pathway “see-saw”. Front. Immunol. 4, 93 (2013).
Dalakas, M. C., Alexopoulos, H. & Spaeth, P. J. Complement in neurological disorders and emerging complement-targeted therapeutics. Nat. Rev. Neurol. 16, 601–617 (2020).
Kopczynska, M. et al. Complement system biomarkers in first episode psychosis. Schizophr. Res. 204, 16–22 (2019).
Spitzer, R. L., Williams, J. B., Gibbon, M. & First, M. B. The structured clinical interview for DSM-III-R (SCID). I: history, rationale, and description. Arch. Gen. Psychiatry 49, 624–629 (1992).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
Wechsler, D. WAIS-R Manual: Wechsler Adult Intelligence Scale-revised. (Psychological Corporation, 1981).
Gavett, B. E. et al. Practice effects on story memory and list learning tests in the neuropsychological assessment of older adults. PLoS One 11, e0164492 (2016).
Yu, H. et al. Association of the plasma complement system with brain volume deficits in bipolar and major depressive disorders. Psychol. Med. 53, 6102–6112 (2023).
Askari, M. et al. A study of the association between cognitive abilities and dietary intake in young women. Nutr. Health 26, 263–270 (2020).
Tseng, H. H. et al. Peripheral inflammation is associated with dysfunctional corticostriatal circuitry and executive dysfunction in bipolar disorder patients. Brain Behav. Immun. 91, 695–702 (2021).
Cai, J., Luo, J., Wang, S. & Yang, S. Feature selection in machine learning: a new perspective. Neurocomputing 300, 70–79 (2018).
Caldiroli, A. et al. The relationship of IQ and emotional processing with insula volume in schizophrenia. Schizophr. Res. 202, 141–148 (2018).
Yang, Y. et al. Altered levels of acute phase proteins in the plasma of patients with schizophrenia. Anal. Chem. 78, 3571–3576 (2006).
Maes, M., Vojdani, A., Sirivichayakul, S., Barbosa, D. S. & Kanchanatawan, B. Inflammatory and oxidative pathways are new drug targets in multiple episode Schizophrenia and Leaky Gut, Klebsiella pneumoniae, and C1q immune complexes are additional drug targets in first episode Schizophrenia. Mol. Neurobiol. 58, 3319–3334 (2021).
Hakobyan, S., Boyajyan, A. & Sim, R. B. Classical pathway complement activity in schizophrenia. Neurosci. Lett. 374, 35–37 (2005).
Zhang, C., Lv, Q., Fan, W., Tang, W. & Yi, Z. Influence of CFH gene on symptom severity of schizophrenia. Neuropsychiatr. Dis. Treat 13, 697–706 (2017).
Mayilyan, K. R., Arnold, J. N., Presanis, J. S., Soghoyan, A. F. & Sim, R. B. Increased complement classical and mannan-binding lectin pathway activities in schizophrenia. Neurosci. Lett. 404, 336–341 (2006).
Laskaris, L. et al. Investigation of peripheral complement factors across stages of psychosis. Schizophr. Res. 204, 30–37 (2019).
Purcell, S. M. et al. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 460, 748–752 (2009).
Shin Yim, Y. et al. Reversing behavioural abnormalities in mice exposed to maternal inflammation. Nature 549, 482–487 (2017).
Santos Sória, L., Moura Gubert, C., Ceresér, K. M., Gama, C. S. & Kapczinski, F. Increased serum levels of C3 and C4 in patients with schizophrenia compared to eutymic patients with bipolar disorder and healthy. Revista brasileira de psiquiatria 34, 119–120 (2012).
Ni, J. et al. A preliminary genetic analysis of complement 3 gene and Schizophrenia. PloS One 10, e0136372 (2015).
Wang, C. et al. Microglia mediate forgetting via complement-dependent synaptic elimination. Science 367, 688–694 (2020).
Hammond, J. W. et al. Complement-dependent synapse loss and microgliosis in a mouse model of multiple sclerosis. Brain Behav. Immun. 87, 739–750 (2020).
Presumey, J., Bialas, A. R. & Carroll, M. C. in Advances in immunology Vol. 135 (ed F. W. Alt) 53-79 (Academic Press, 2017).
Gomez-Arboledas, A., Acharya, M. M. & Tenner, A. J. The role of complement in synaptic pruning and neurodegeneration. ImmunoTargets Ther. 10, 373–386 (2021).
Carpanini, S. M., Torvell, M. & Morgan, B. P. Therapeutic inhibition of the complement system in diseases of the central nervous system. Front. Immunol. 10, 362–362 (2019).
Alawieh, A. M., Langley, E. F., Feng, W., Spiotta, A. M. & Tomlinson, S. Complement-dependent synaptic uptake and cognitive decline after stroke and reperfusion therapy. J. Neurosci. 40, 4042–4058 (2020).
Lizano, P. et al. Multivariate relationships between peripheral inflammatory marker subtypes and cognitive and brain structural measures in psychosis. Mol. Psychiatry 26, 3430–3443 (2021).
Ali, F. T. et al. Redox dysregulation, immuno-inflammatory alterations and genetic variants of BDNF and MMP-9 in schizophrenia: pathophysiological and phenotypic implications. Schizophr. Res. 188, 98–109 (2017).
Li, H. et al. Plasma levels of Th17-related cytokines and complement C3 correlated with aggressive behavior in patients with schizophrenia. Psychiatry Res. 246, 700–706 (2016).
Hernandez, L. M. et al. Multi-ancestry phenome-wide association of complement component 4 variation with psychiatric and brain phenotypes in youth. Genome Biol. 24, 42 (2023).
Prestwood, T. R. et al. Roles of inflammation in intrinsic pathophysiology and antipsychotic drug-induced metabolic disturbances of schizophrenia. Behav. Brain Res.402, 113101 (2021).
Stevens, B. et al. The classical complement cascade mediates CNS synapse elimination. Cell 131, 1164–1178 (2007).
Acknowledgements
The authors are grateful for valuable contributions from their coworkers at the Affiliated Mental Health Centre, Hangzhou Seventh People’s Hospital and West China Hospital of Sichuan University.
Funding
This work was supported by the National Natural Science Foundation of China Key Project (81630030 and 81920108018 to T.L.), National Natural Science Foundation of China (81871054 and 81501159 to P.N., 82101598 to H.Y.), Special Foundation for Brain Research in the Science and Technology Program of Guangdong (2018B030334001 to T.L.), 2021 Project for Hangzhou Medical Disciplines of Excellence & Key Project for Hangzhou Medical Disciplines, 1.3.5 Project for Disciplines of Excellence at West China Hospital of Sichuan University (ZY2016103, ZY2016203, and ZYGD20004 to T.L.), and Introductory Project of the Suzhou Clinical Expert Team (SZYJTD201715 to T.L.).
Author information
Authors and Affiliations
Contributions
H.Y., P.N., J.C. and T.L. conceptualized and designed the study, had full access to all data, and take responsibility for its integrity and accuracy. W.W., J.W., W.D. and X.M. were responsible for data collection, and Y.T., L.Z., M.L. and X.L. performed all data analyses. H.Y., P.N., Q.W. and W.G. drafted the manuscript. All authors critically revised and approved the final version of the manuscript. All authors agree to be held accountable for all aspects of the work and to ensure that questions related to the accuracy or integrity of the data and results are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of West China Hospital, Sichuan University, and it complied with the principles of the Declaration of Helsinki. All participants were fully informed about the study’s purpose and procedures, and they provided written informed consent. A copy of the written consent form is available for review from the Editor of this journal.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yu, H., Ni, P., Tian, Y. et al. Association of elevated levels of peripheral complement components with cortical thinning and impaired logical memory in drug-naïve patients with first-episode schizophrenia. Schizophr 9, 79 (2023). https://doi.org/10.1038/s41537-023-00409-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-023-00409-1