Abstract
Breathlessness is a common symptom that may have multiple causes in any one individual and causes that may change over time. Breathlessness campaigns encourage people to see their General Practitioner if they are unduly breathless. Members of the London Respiratory Network collaborated to develop a tool that would encourage a holistic approach to breathlessness, which was applicable both at the time of diagnosis and during ongoing management. This has led to the development of the aide memoire “Breathing SPACE”, which encompasses five key themes—smoking, pulmonary disease, anxiety/psychosocial factors, cardiac disease, and exercise/fitness. A particular concern was to ensure that high-value interventions (smoking cessation and exercise interventions) are prioritised across the life-course and throughout the course of disease management. The approach is relevant both to well people and in those with an underling diagnosis or diagnoses. The inclusion of anxiety draws attention to the importance of mental health issues. Parity of esteem requires the physical health problems of people with mental illness to be addressed. The SPACE mnemonic also addresses the problem of underdiagnosis of heart disease in people with lung disease and vice versa, as well as the systematic undertreatment of these conditions where they do co-occur.
Similar content being viewed by others
Introduction
Breathlessness is one of the most common symptoms causing people to interact with the health-care system, present in about 10% of all adults and 30% of older people.1,2 It can be frightening and disabling, but many people ignore or normalise the symptom and fail to act on it. This can delay diagnosis and effective interventions, both medical and “lifestyle”. For example, data on patients with chronic obstructive pulmonary disease (COPD) show clearly that, for many individuals, opportunities are missed to make a diagnosis in the years prior to the condition finally being recognised.3,4 Multimorbidity is common5 and breathlessness in any individual is likely to be multifactorial.6 The London Respiratory Network wished to develop an aide memoire to facilitate a systematic approach to this. Consensus discussions identified smoking, pulmonary disease, anxiety, cardiac disease, and exercise level/unfitness as important and often interacting contributors to breathlessness, which can be encompassed by the acronym “Breathing SPACE” (Table 1). These items should be considered in any breathless patient, both during the diagnostic process and their subsequent management, though they may not all be addressed in a single consultation. The approach is intended to be relevant both to health-care practitioners and to commissioners of health-care services.
The application of this approach in two typical patients, one with COPD and one where deconditioning is the main issue, is illustrated in Fig. 1.
Application of Breathing SPACE in a typical patient with COPD (a) and in a patient where the main issue is deconditioning and lifestyle(b). In a typical patient with COPD, all five of the SPACE elements may be in play with attention required to Smoking cessation, treatments directly for the Pulmonary condition (vaccination, rehabilitation, inhaled medication), Anxiety about going outside for fear of being seen to be breathless, ensuring medication for a Cardiac co-morbidity is optimised, and a need to continue to consider increase Exercise levels following pulmonary rehabilitation and behaviour change
Smoking
Smoking is a leading preventable cause of ill health, but smoking cessation is also one of the most effective treatments for many long-term conditions.11,12,13,14 Ask breathless patients about smoking history, encourage smokers to quit and offer assistance to overcome their tobacco dependence. Brief smoking cessation advice is an effective intervention,15 but counselling support combined with pharmacotherapy is more so.16 For example, the cost per quality adjusted life year of combined smoking cessation counselling and pharmacotherapy in COPD is only €2400, compared with €8200 for intensive counselling and €16,900 for brief advice.17 Providing evidence-based smoking cessation for inpatients who smoke has been shown not only to significantly reduce readmissions at 30 days (by about half), but also to significantly reduce mortality at 1 year (again by about a half).13 Smoking is highly prevalent in socioeconomically deprived groups and in those with mental health problems,18 and support to these groups should be prioritised. The National Centre for Smoking Cessation and Training website (www.ncsct.co.uk/) is a useful resource, including online training.
Pulmonary disease
Breathlessness is a characteristic manifestation of pulmonary diseases such as COPD and asthma. Suggestive features may trigger a referral, or investigations such as a chest X-ray. Perform quality-assured spirometry promptly on any patient with symptoms of long-term breathlessness. This can be diagnostic for airflow obstruction and the demonstration of abnormal lung function provides an additional incentive for smokers to quit.19 Asthma is by definition variable so normal spirometry does not rule it out. Timely diagnosis of COPD also has good value—low diagnostic rates of COPD are associated with higher disease-specific costs20 and prevalence of undiagnosed COPD is strongly associated with rates of hospital admission for acute exacerbations.21 Prioritise high-value interventions, including flu vaccination, smoking cessation, and pulmonary rehabilitation, which have significantly lower costs per QALY than pharmacotherapy (Fig. 2).22
The pyramid of value for COPD interventions.The pyramid of value for COPD interventions developed by the London Respiratory Network with The London School of Economics (reproduced from22) gives estimates of cost per quality-adjusted life year gained. LABA long-acting β2 agonist, QALY quality-adjusted life year
Anxiety
Anxiety is taken here to represent a range of psychosocial problems. Anxiety disorders can present with breathlessness as a primary symptom. Alternatively, anxiety can aggravate the symptoms of a long-term condition such as COPD or heart failure.23,24,25 A key element of “parity of esteem” for mental health is that the physical health problems of people with mental health conditions are no longer neglected. Smoking rates are high in people with mental illness and contribute considerably to reduced life expectancy.18 Smoking cessation interventions are safe and likely to be as effective in people with a mental health diagnosis as those without.26,27,28
Pulmonary and cardiac rehabilitation improve mental as well as physical components of health status.29,30 Although patients with mental health problems benefit from rehabilitation, they may be less likely to attend or complete programmes31—identifying people who need additional support and encouragement to attend and continue rehabilitation is important. For some individuals, participation in peer support activities like British Lung Foundation Breathe Easy Groups may be beneficial. Consider referral for psychological therapy; cognitive-behavioural therapy is efficacious in people with respiratory disease and anxiety.32
Cardiac causes
A cardiac cause of breathlessness is suggested by a history of hypertension, diabetes, hypercholesterolaemia or ischaemic heart disease, and by physical findings such as lung crepitations, the presence of oedema, tachycardia, cardiac murmurs, or atrial fibrillation. A normal electrocardiogram (ECG) reduces the likelihood of cardiac disease but consider investigations such as blood natriuretic peptide (BNP) and echocardiography if there is clinical suspicion.33
Lung disease is also common in people with heart disease,5 so the possibility of a dual diagnosis should be considered. For example, 15–24% of people with COPD also have ischaemic heart disease5 and one-third of people with atrial fibrillation have a diagnosis of asthma or COPD.34 Evidence suggests systematic undertreatment of patients with COPD following myocardial infarction; they are less likely to receive beta blockers, although these can be safely administered.35
Hyperinflation caused by airflow obstruction restricts cardiac output36 and the “cardiac” aspects of lung diagnoses should be considered. In patients with COPD, low oxygen saturations, especially if they are disproportionate to the degree of airflow obstruction, may represent pulmonary hypertension that can lead to right-sided heart failure. Consider sleep-disordered breathing with nocturnal hypoxia in individuals with a high body mass index (BMI), oedema, or a history of type II respiratory failure. Ask about daytime somnolence, morning headaches, and confusion.
Exercise level and fitness
Many people find that their exercise capacity decreases as they get older and attribute this to aging when it is in fact a consequence of physical inactivity and deconditioning.37 Excluding the presence of a specific pulmonary, cardiac, or psychological pathology is likely to be the priority in a patient presenting with breathlessness, but even having done this there is evidence that brief interventions to increase physical activity in apparently healthy people are cost-effective.8,38
People aging with a sedentary lifestyle are at increased risk of developing many health conditions, including hypertension, obesity, diabetes, depression, osteoporosis, frailty, and falls. Adoption of walking and cycling, as well as improving the fitness of individuals and reducing their risk of future disease, also has other benefits.39 It reduces the emission of pollutants (particulates, NO2), which increase the risk of developing conditions like asthma and worsen outcomes in people who already have cardiorespiratory disease. The reduction in carbon emissions from adopting active transport also brings a climate change benefit.
Exercise rehabilitation is known to be an effective intervention in cardiorespiratory disease29,40,41,42 and pulmonary rehabilitation is one of the highest value interventions in COPD.22 Of note, activity levels are reduced even in early COPD43 and inactivity is associated with more rapid decline in lung function in healthy populations and with more rapid progression of COPD.44 Although it has not been subjected to prospective randomised controlled trials, these observations do suggest that, in people diagnosed at an early stage, robust encouragement to increase activity level with a clear explanation of the benefits of doing so may alter the way that their lung condition progresses as they age. Of equal importance, increasing physical activity should also limit the development and impact of multi-morbidities—including hypertension, diabetes, osteoporosis, depression, and cognitive dysfunction—that are known to accumulate through the impact of progressive sedentarism.45 A person who understands the need to push against the limits of their breathlessness as part of their self-management of a long-term condition, and believes in their capacity to do so, could be expected to maintain their performance better than someone who is slowly withdrawing from activities in the face of unexplained breathlessness due to progressive, undiagnosed, cardiorespiratory disease. A key message for patients is that it is not harmful to make yourself breathless. Pedometer-based interventions with a step count goal are effective.9,10
A coordinated approach—multimorbidity
Multimorbidity is the norm rather than the exception; only 20% of people with COPD have it as their only long-term condition.5 Exercise and smoking cessation will benefit other conditions such as hypertension and diabetes, as well as cardiac and pulmonary disease. Anaemia may present with breathlessness and is potentially reversible. Where a referral is made it should ideally be to a service that can function in a way that is symptom specific, dealing with “breathlessness”, rather than to one that can only investigate from a cardiac or respiratory perspective with the patient requiring a second referral if one or other condition is excluded. Table 2 includes recommendations for commissioners, and further recommendations are available in this European Respiratory Society Monograph.46
Conclusion
Breathlessness is an important and challenging symptom. The Breathing SPACE approach should help to ensure that underlying diagnoses will not be missed, especially if there is more than one, and also that these are considered as patients are followed up over time. Focus attention on high-value interventions, in particular smoking cessation and exercise rehabilitation, to optimise the sustainable and equitable utilisation of finite health-care resources.
References
Williams S., IMPRESS Breathlessness Working Party. Epidemiology of breathlessness—literature review. 2014.
Ho SF, O'Mahony MS, Steward JA, Breay P, Buchalter M, Burr ML. Dyspnoea and quality of life in older people at home. Age and Ageing 30, 155–9 (2001).
Jones RCM, Price D, Ryan D, et al. Opportunities to diagnose chronic obstructive pulmonary disease in routine care in the UK: a retrospective study of a clinical cohort. The Lancet Respiratory Medicine 2, 267–276 (2014).
Nacul, L. et al. COPD in England: a comparison of expected, model-based prevalence and observed prevalence from general practice data. J. Public Health 33, 108–116 (2011).
Barnett, K., Mercer, S. W., Norbury, M., Watt, G., Wyke, S. & Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 380, 37–43 (2012).
Chin C. & Booth S. Managing breathlessness: a palliative care approach. Postgrad. Med. J. 2016. doi:10.1136/postgradmedj-2015-133578.
London Respiratory Senate. Helping Smokers Quit: Adding Value to Every Clinical Contact by Treating Tobacco Dependence (2014).
National Institute for Health and Clinical Excellence. Implementation Advice—Four Commonly Used Methods to Increase Physical Activity (2006).
Bravata, D. M. et al. Using pedometers to increase physical activity and improve health: a systematic review. J. Am. Med. Assoc. 298(19), 2296–2304 (2007).
Mendoza, L. et al. Pedometers to enhance physical activity in COPD: a randomised controlled trial. Eur. Respir. J. 45(2), 347–354 (2015).
Pride, N. B. Smoking cessation: effects on symptoms, spirometry and future trends in COPD. Thorax 56(suppl 2), ii7–ii10 (2001).
Critchley J. A. & Capewell S. Smoking cessation for the secondary prevention of coronary heart disease. Cochrane Database Syst. Rev. 2003. doi:10.1002/14651858.CD003041.pub2.
Mullen K. A. et al. Effectiveness of a hospital-initiated smoking cessation programme: 2-year health and healthcare outcomes. Tob. Control 2016. doi:10.1136/tobaccocontrol-2015-052728.
London Clinical Senate. Helping smokers quit, http://www.londonsenate.nhs.uk/helping-smokers-quit/, accessed 28 November 2016 (2016).
Stead L. F. et al. Physician advice for smoking cessation. Cochrane Database Syst. Rev. 2013(5).
Stead L. F., Koilpillai P., Fanshawe T. R. & Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database Syst. Rev. 2016(3).
Hoogendoorn, M., Feenstra, T. L., Hoogenveen, R. T., Rutten-van, M. Ã. & lken, M. P. M. H. Long-term effectiveness and cost-effectiveness of smoking cessation interventions in patients with COPD. Thorax 65(8), 711–718 (2010).
Royal College of Physicians. Smoking and Mental Health (2014).
Parkes, G., Greenhalgh, T., Griffin, M. & Dent, R. Effect on smoking quit rate of telling patients their lung age: the Step2quit randomised controlled trial. Br. Med. J. 336(7644), 598–600 (2008).
Jansson, S. A. et al. Cost differences for COPD with and without physician-diagnosis. Chron. Obstruct. Pulmon. Dis. 2(4), 427–434 (2005).
Calderón-Larrañaga, A. et al. Association of population and primary healthcare factors with hospital admission rates for chronic obstructive pulmonary disease in England: national cross-sectional study. Thorax 66(3), 191–196 (2011).
Zoumot, Z., Jordan, S. & Hopkinson, N. S. Emphysema: time to say farewell to therapeutic nihilism. Thorax 69(11), 973–975 (2014).
von Leupoldt, A. & Dahme, B. Psychological aspects in the perception of dyspnea in obstructive pulmonary diseases. Respir. Med. 101(3), 411–422 (2007).
von Leupoldt, A. & Kenn, K. The psychology of chronic obstructive pulmonary disease. Curr. Opin. Psychiatry 26(5), 458–463 (2013).
Easton, K., Coventry, P., Lovell, K., Carter, L.-A. & Deaton, C. Prevalence and measurement of anxiety in samples of patients with heart failure: meta-analysis. J. Cardiovasc. Nurs. 31(4), 367–379 (2016).
National Institute for Clinical Excellence. Smoking: Acute, Maternity and Mental Health Services (2013).
UK Department of Health. No Health without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages—A Call to Action (2011).
Anthenelli, R. M. et al. Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. Lancet 387(10037), 2507–2520 (2016).
Anderson, L. et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 1, CD001800 (2016).
McCarthy B. et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2015(2):CD003793.
Boutou A. K. et al. An evaluation of factors associated with completion and benefit from pulmonary rehabilitation in COPD. BMJ Open Respir. Res. 1, (2014). doi:10.1136/bmjresp-2014-000051.
Livermore, N., Sharpe, L. & McKenzie, D. Prevention of panic attacks and panic disorder in COPD. Eur. Respir. J. 35(3), 557–563 (2010).
National Institute for Clinical Excellence. Chronic Heart Failure: The Management of Chronic Heart Failure in Adults in Primary and Secondary Care (2010).
Wilke, T. et al. Incidence and prevalence of atrial fibrillation: an analysis based on 8.3 million patients. Europace 15(4), 486–493 (2013).
Minor, D. S., Meyer, A. M., Long, R. C. & Butler, K. R. β-Blockers and chronic obstructive pulmonary disease: inappropriate avoidance? J. Clin. Hypertens. 15(12), 925–930 (2013).
Faisal, A. et al. Effective bronchoscopic lung volume reduction accelerates exercise oxygen uptake kinetics in Emphysema. Chest 149, 435–446 (2016).
Kelly J. L., Elkin S. L., Fluxman J., MI P., Soljak M. & NS H. Breathlessness and skeletal muscle weakness in patients undergoing lung health screening in primary care. Chron. Obstruct. Pulmon. Dis. 10, 40–54 (2013).
Vijay G., Wilson E. C., Suhrcke M., Hardeman W. & Sutton S. Are brief interventions to increase physical activity cost-effective? A systematic review. Br. J. Sports Med. (2015). doi:10.1136/bjsports-2015-094655.
Aitsi-Selmi, A. & Hopkinson, N. S. Breathlessness, physical activity and sustainability of healthcare. Eur. Respir. J. 45(1), 284–285 (2015).
British Thoracic Society. IMPRESS Guide to the Relative Value of COPD Interventions (2012).
Sagar, V. A. et al. Exercise-based rehabilitation for heart failure: systematic review and meta-analysis. Open Heart 2(1), e000163 (2015).
Gielen, S., Laughlin, M. H., O’Conner, C. & Duncker, D. J. Exercise training in patients with heart disease: review of beneficial effects and clinical recommendations. Prog. Cardiovasc. Dis. 57(4), 347–355 (2015).
Shrikrishna, D. et al. Quadriceps wasting and physical inactivity in patients with COPD. Eur. Respir. J. 40(5), 1115–1122 (2012).
Hopkinson, N. S. & Polkey, M. I. Does physical inactivity cause chronic obstructive pulmonary disease? Clin. Sci. 118(9), 565–572 (2010).
Lee I. M. et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 380(9838):219–229.
Williams S. & De Poli C. in Palliative Care in Respiratory Disease (ERS Monograph) (eds Bausewein C., Currow D. C., Johnson M. J.) 172–196 (2015).
Acknowledgements
The Breathing SPACE approach was developed in discussions within the London Respiratory Network (https://www.networks.nhs.uk/nhs-networks/london-lungs/london-respiratory-clinical-leadership-group). This includes nursing, physiotherapy, pharmacy, ambulance service, and health and social care commissioner members, as well as patient input and representatives from the British Lung Foundation and Asthma UK. We would like to thank Margaret McCartney and Martin Brunet for their thoughtful comments and suggestions during the development of this paper.
Author contributions
N.S.H. produced the first draft following discussions within the London Respiratory Network Board. N.B. contributed to a subsequent draft and both authors approved the final version, which was also reviewed by a patient.
Competing interests
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Hopkinson, N.S., Baxter, N. & on behalf of the London Respiratory Network. Breathing SPACE—a practical approach to the breathless patient. npj Prim Care Resp Med 27, 5 (2017). https://doi.org/10.1038/s41533-016-0006-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-016-0006-6
This article is cited by
-
Mediating role of coping styles on the relationship between personality types and mental disorders in cardiovascular patients: a cross-sectional study in Iran
BMC Psychiatry (2023)
-
Assessment and diagnosis of chronic dyspnoea: a literature review
npj Primary Care Respiratory Medicine (2022)
-
Pulmonary rehabilitation in patients with mustard gas lung disease: a study protocol for a randomized controlled trial
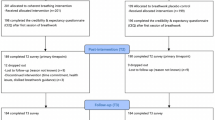
Trials (2019)