Abstract
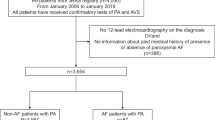
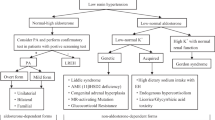
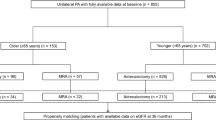
Data on the prognosis of clinically undiagnosed hypertensive patients who are aldosterone-to-renin ratio (ARR) positive are still scarce. Therefore, we investigated the clinical characteristics of clinically undiagnosed hypertensive patients who were ARR-positive and the influence of their different treatments on the occurrence and development of complications. A total of 285 hypertensive patients data with ARR ≥ 3.8 in the Second People’s Hospital of Huai’an from January 2019 to December 2021 were collected, and 135 undiagnosed hypertensive patients were ultimately included in the analysis. According to their treatment strategy in various clinical departments, 135 patients were divided into the operation, spironolactone and control groups. Then, the clinical characteristics and the occurrence and development of complications in the three groups were compared. The results suggested that: (1) Only 34 (11.9%) of 285 hypertensive patients with ARR ≥ 3.8 were clearly diagnosed with Primary aldosteronism (PA) through functional tests, and the blood pressure (BP) compliance rate was only 50.30% during follow-up. (2) Based on exclusion criteria, 135 undiagnosed hypertensive patients were eventually included in the analysis. Patients in the surgery group had lower blood potassium levels and higher aldosterone levels than those in the other two groups, and their risk of new cerebrovascular complications was lower than that of the patients in the spironolactone group. (3) The risk of new cerebrovascular complications in the spironolactone group was 9.520 times higher than that of the control group, and this risk mainly occurred in patients with ARR values of 3.8–5.7. On the whole, surgery remains a good option for hypertensive patients with severe hyperaldosteronism and hypokalemia and those unable to undergo confirmatory tests; however, spironolactone therapy in patients with clinically undiagnosed hypertension, especially those with 3.8 ≤ ARR < 5.7, confered a higher risk of new cerebrovascular complications.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The Management of Primary Aldosteronism: Case Detection, Diagnosis, and Treatment: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Athimulam S, Lazik N, Bancos I. Low-Renin Hypertension. Endocrinol Metab Clin North Am. 2019;48:701–15.
Ruhle BC, White MG, Alsafran S, Kaplan EL, Angelos P, Grogan RH. Keeping primary aldosteronism in mind: Deficiencies in screening at-risk hypertensives. Surgery. 2019;165:221–7.
Lin X, Ullah MHE, Wu X, Xu F, Shan SK, Lei LM, et al. Cerebro-Cardiovascular Risk, Target Organ Damage, and Treatment Outcomes in Primary Aldosteronism. Front Cardiovasc Med. 2021;8:798364.
Young WJ. Diagnosis and treatment of primary aldosteronism: practical clinical perspectives. J Intern Med. 2019;285:126–48.
Catena C, Lapenna R, Baroselli S, Nadalini E, Colussi G, Novello M, et al. Insulin sensitivity in patients with primary aldosteronism: a follow-up study. J Clin Endocrinol Metab. 2006;91:3457–63.
Hundemer GL, Curhan GC, Yozamp N, et al. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6:51–9.
Johnson DW, Jones GR, Mathew TH, Ludlow MJ, Doogue MP, Jose MD. Chronic kidney disease and automatic reporting of estimated glomerular filtration rate: new developments and revised recommendations. Med J Aust. 2012;197:224–5.
Adrenal Group of the Endocrinology Branch of the Chinese Medical Association. Expert consensus on the diagnosis and treatment of primary aldosteronism [J][J]. Chin J Endocrine Metabol. 2016;32:188–95.
American Diabetes Association Professional Practice Committee. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022;45:S17–S38.
Vogt A, Weingärtner O. Management of dyslipidaemias: The New 2019 ESC/EAS-Guideline. Dtsch Med Wochenschr. 2021;146:75–84.
Cheung AK, Chang TI, Cushman WC, Furth SL, Hou FF, Ix JH, et al. Executive summary of the KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int. 2021;99:559–69.
Sang X, Jiang Y, Wang W, Yan L, Zhao J, Peng Y, et al. Prevalence of and risk factors for primary aldosteronism among patients with resistant hypertension in China. J Hypertens. 2013;31:1465–71.
Xu Z, Yang J, Hu J, Song Y, He W, Luo T, et al. Primary Aldosteronism in Patients in China With Recently Detected Hypertension. J Am Coll Cardiol. 2020;75:1913–22.
Li YM, Ren Y, Chen T, Tian HM. Update and Research Progress in the Diagnosis of Primary Aldosteronism. Sichuan Da Xue Xue Bao Yi Xue Ban. 2020;51:267–77.
Reincke M, Bancos I, Mulatero P, Scholl UI, Stowasser M, Williams TA. Diagnosis and treatment of primary aldosteronism. Lancet Diabetes Endocrinol. 2021;9:876–92.
Qian N, Xu J, Wang Y. Stroke Risks in Primary Aldosteronism with Different Treatments: A Systematic Review and Meta-Analysis. J Cardiovasc Dev Dis. 2022;9:300.
Jing Y, Liao K, Li R, Yang S, Song Y, He W, et al. Cardiovascular events and all-cause mortality in surgically or medically treated primary aldosteronism: A Meta-analysis. J Renin Angiotensin Aldosterone Syst. 2021;22:1148438405.
Chang YH, Chung SD, Wu CH, Chueh JS, Chen L, Lin PC, et al. Surgery decreases the long-term incident stroke risk in patients with primary aldosteronism. Surgery. 2020;167:367–77.
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and Clinical Manifestations of Primary Aldosteronism Encountered in Primary Care Practice. J Am Coll Cardiol. 2017;69:1811–20.
McCarthy J, Yang J, Clissold B, Young MJ, Fuller PJ, Phan T. Hypertension Management in Stroke Prevention: Time to Consider Primary Aldosteronism. Stroke. 2021;52:e626–34.
Acknowledgements
The authors thank all participants for their cooperation and sample contribution.
Funding
This work was supported by Grant HAWJ202014 from the Huai’an Natural Science Research Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, R., Hao, H., Dai, Y. et al. Effects of different treatment modalities on cardiovascular disease in ARR-positive hypertensive patients. Hypertens Res (2024). https://doi.org/10.1038/s41440-024-01676-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41440-024-01676-w