Abstract
The pathogenesis of hypertension is multifactorial in patients with chronic kidney disease (CKD). We explored the relative contribution of arterial stiffness and fluid overload to blood pressure (BP) in these patients. We evaluated 1531 patients from a prospective observational cohort study of high-risk patients with cardiovascular disease. BP, arterial stiffness, and volume status expressed as the extracellular water/total body water ratio (ECW/TBW) were measured by 24-h BP monitoring, pulse-wave velocity (PWV), and bioelectrical impedance analysis, respectively. Multiple linear regression analysis showed that both PWV and ECW/TBW of the patients with CKD were significantly associated with 24-h systolic BP (SBP). The areas under the receiver-operating characteristic curve (AUCs) for predicting 24-h SBP ≥130 mm Hg significantly increased after PWV was added to conventional factors regardless of CKD status. However, the AUCs did not increase in the ECW/TBW-based models. When a cut-off 24-h SBP level of 140 mm Hg was used, the predictability of ECW/TBW for elevated BP significantly improved in patients with CKD (0.718 vs. 0.683, P = 0.034) but not in those without. Notably, a significant impact of arterial stiffness on high BP was consistently observed regardless of CKD status. This association was further confirmed by the net reclassification and integrated discriminant improvements, root mean squared error with adjusted R2, and interaction effects. As kidney function declines, fluid overload is significantly associated with high BP. The impact of fluid overload on BP is only observed in more severe hypertension in patients with CKD.
Similar content being viewed by others
Introduction
Cardiovascular morbidity and mortality rates markedly increase in patients with chronic kidney disease (CKD), and the presence of CKD worsens the prognosis of cardiovascular disease (CVD) [1, 2]. A meta-analysis of 80,098 patients with heart failure showed that cardiovascular mortality increases as kidney function declines [3]. Anavekar et al. [4] also demonstrated that cardiovascular complications, including mortality, reinfarction, congestive heart failure, and stroke, occur more frequently in patients with decreased renal function.
Hypertension is a crucial and modifiable risk factor in preventing CVD [5]. Lowering high blood pressure (BP) to an appropriate range can retard renal function deterioration and improve adverse cardiovascular outcomes [6]. However, maintaining optimal BP is difficult owing to many comorbidities that can affect BP and the highly variable responsiveness to antihypertensive medications in patients with renal failure [7].
In patients with hypertension with normal renal function, the factors related to increased BP are well established. In addition, arterial stiffness has gained attention as a key contributor to increased BP [8]. Arterial stiffness has long been considered a complication of hypertension. However, many researchers demonstrated a bidirectional interaction between arterial stiffness and hypertension [9]. In contrast, nontraditional factors in patients with CKD are also implicated in elevated BP [10]. Among these, fluid overload has been taken for granted as a major determinant of hypertension. However, it is uncertain whether fluid overload itself can increase BP. Surprisingly, to date, this issue has never been tested in depth using an objective fluid status measure.
Thus, we aimed to clarify the differential factors that determine BP in patients with and without CKD and explore the relative contribution of fluid overload to BP in these patients.
Methods
Detailed methods are provided in the supplemental data.
Ethics statement
This study was conducted in accordance with the Declaration of Helsinki principles, and the study protocol was approved by the Institutional Review Board (IRB) at Yonsei University Health System (YUHS) Clinical Trial Center. All patients provided written informed consent before participation (IRB no. 4-2013-0581).
Study population
The study population was selected from the Cardiovascular and Metabolic Diseases Etiology Research Center-High Risk Cohort (CMERC-HI) at YUHS between November 2013 and November 2016. Briefly, the CMERC-HI is a prospective cohort study aiming at developing more specific preventive strategies for patients with a high cerebro-CVD risk (NCT02003781). Patients who fit at least one of the following descriptions were enrolled: high-risk patients with hypertension, namely patients with hypertension and an estimated glomerular filtration rate (eGFR) of ≥60 mL/min per 1.73 m2 and target organ damage or an eGFR of <60 mL/min/per 1.73 m2, and patients with diabetes and a random urine albumin–creatinine ratio of ≥30 mg/g; patients with end-stage renal disease (ESRD) undergoing dialysis; first-degree relatives of patients with early-onset acute myocardial infarction (MI); patients with asymptomatic atherosclerotic CVD; patients with rheumatoid arthritis aged >40 years taking methotrexate or steroid; patients with atrial fibrillation and CHA2DS2-VASc score of ≥1; and kidney transplant recipients (>3 months after transplantation). The exclusion criteria included: (i) acute MI history (ST-segment elevation MI or non-ST-segment elevation MI) or acute coronary syndrome (unstable angina); (ii) symptomatic peripheral artery disease; (iii) symptomatic heart failure; (iv) life expectancy of <6 months or severe non-CVD (e.g., metastatic cancer, sepsis, and liver cirrhosis); and (v) pregnancy or breastfeeding. We additionally excluded patients with ESRD undergoing dialysis or kidney transplantation, patients with no serum creatinine or 24-h ambulatory BP monitoring (ABPM) data, and patients using immunosuppressive drugs and NSAIDs that could increase BP. Finally, a total of 1,531 patients were analyzed (Supplemental Fig. 1).
Clinical and biochemical data collection
Demographic and clinical data were collected at the time of enrollment. These included age, sex, height, weight, and comorbidities. The participants were considered to have diabetes mellitus if they had a history of diabetes mellitus, were receiving antidiabetic treatment, or had fasting plasma glucose levels of ≥126 mg/dL. Hypertension was defined as a self-reported history of hypertension, antihypertensive medication use, or an office-based BP of ≥140/90 mm Hg. CKD was defined as an eGFR of <60 mL/min/per 1.73 m2[11]. eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation [12].
Measurement of BP, arterial stiffness, and fluid status
We measured both office-based and ambulatory BP. Office-based BP was measured three times at 5-min intervals. Ambulatory BP was the average value of the 24-h ABPM data. The patients were classified on the basis of the dipping pattern [13]. We used this averaged value of 24-h ABPM because ECW/TBW was significantly correlated with both daytime SBP and nighttime SBP (Supplemental Table 1). Arterial stiffness was determined by measuring the brachial to ankle pulse-wave velocity (baPWV) and carotid to femoral PWV (cfPWV) [14, 15]. Volume status was assessed using direct segmental multifrequency bioelectrical impedance analysis (BIA). Because excess fluid in the interstitial compartment, which is a component of extracellular water (ECW), results in edema, fluid overload was defined as the ECW to total body water (TBW) ratio (ECW/TBW) [16]. Both PWV and ECW/TBW were expressed as continuous variables and used to define arterial stiffness and water status, respectively. Further, overhydration was defined as an ECW/TBW of >0.400. All measurements were performed by trained staff according to the manufacturer’s recommendations.
Statistical analyses
The associations between BP and clinical and biochemical variables were assessed using Pearson’s correlation coefficient. Multiple linear regression analysis was performed to identify independent correlates of BP. In addition, three different multivariable logistic models were constructed to compare the predictability of arterial stiffness and ECW/TBW for a 24-h systolic BP (SBP) of ≥140 mm Hg. Significant variables in the univariable analysis (P <0.05) were included in the multivariable analyses. Model 1 included conventional risk factors for hypertension. baPWV and ECW/TBW were sequentially entered in Models 2 and 3, respectively. The predictive value of each multivariable model for high BP was determined using the receiver-operating characteristic (ROC) curves, net reclassification improvement (NRI), and integrated discrimination improvement (IDI). Furthermore, we calculated the root mean squared error (RMSE) and adjusted R-squared (R2) to assess the fit of the linear regression models in which 24-h SBP was entered as a continuous variable. Finally, we examined the interaction effects between CKD status and baPWV and ECW/TBW.
All analyses were performed using SPSS version 23.0 (SPSS Inc., Chicago, IL, USA), SAS version 9.4 (SAS Institute, Cary, NC, USA), or GraphPad Prism version 5.0 (GraphPad Software Inc., San Diego, CA, USA). The significance level was defined as P <0.05.
Results
Baseline characteristics
The baseline characteristics of the study subjects are presented in Table 1. The CKD group had more unfavorable features in most aspects than the non-CKD group. The CKD group had significantly higher 24-h SBP and pulse pressure than the non-CKD group, whereas the 24-h diastolic BP (DBP) did not differ between them. The CKD group had more non-dippers and reverse dippers, stiffer arteries, as evidenced by a higher baPWV, and greater volume overload than the non-CKD group.
Factors associated with 24-h SBP
The correlation between 24-h SBP and other clinical and biochemical variables is presented in Table 2 and Supplemental Table 2. In the multiple linear regression analyses after adjustment for confounders, baPWV was independently associated with 24-h SBP in both groups. However, ECW/TBW, but not baPWV, was associated with 24-h SBP in the CKD group. As fluid status can affect arterial stiffness [17], we also checked the variance inflation factor (VIF) for multicollinearity among baPWV, ECW/TBW, and 24-h SBP using multiple linear regression analysis. The VIFs for baPWV and ECW/TBW were <1.2 in all analyses, suggesting that collinearity among these factors was less likely (data not shown).
Factors associated with 24-h DBP
We then examined the factors affecting 24-h DBP. Pearson’s correlation coefficients for 24-h DBP are presented in Supplemental Table 3. Multivariable-adjusted regression analysis revealed that baPWV was significantly associated with 24-h DBP only in the CKD group (β = 0.682, P < 0.001). ECW/TBW was not associated with 24-h DBP in both groups (Supplemental Table 4).
Relative contribution of arterial stiffness and volume overload to high BP
Next, we evaluated the differential influence of arterial stiffness and volume overload on BP. Twenty-four-hour SBP is a more important determinant of hypertension in CKD [18]. No significant association between ECW/TBW and 24-h DBP was reported. In this study, baPWV and ECW/TBW differentially affected 24-h SBP, depending on CKD status. Therefore, we selected 24-h SBP as a target dependent variable. Thus, we first performed ROC curve analyses using three multivariable logistic regression models. Model 1 included conventional factors only. Models 2 and 3 additionally included baPWV and ECW/TBW, respectively.
By ambulatory monitoring, hypertension can be defined as a 24-h SBP of ≥130 mm Hg. Adding baPWV to Model 1 significantly increased the areas under the ROC curve (AUCs) for 24-h SBP of ≥130 mm Hg in the non-CKD (0.701 vs. 0.626, P < 0.001) and CKD groups (0.768 vs. 0.717, P < 0.001). This improvement in the predictability for high BP was not found when ECW/TBW was added. However, the baPWV-based model was superior to the ECW/TBW-based model in predicting a 24-h SBP of ≥130 mm Hg (P < 0.001 in non-CKD group and P = 0.028 in CKD group) (Fig. 1a, b). These findings suggest that arterial stiffness is more influential on the early stage of hypertension than fluid overload.
Receiver-operating characteristic curve analysis for 24-h systolic blood pressure ≥130 mm Hg in patients with and without CKD. Notes: 1Antihypertensive medications include angiotensin II receptor blockers, angiotensin-converting enzyme inhibitors, calcium channel blockers, β-blockers, α-blockers, and diuretics. Abbreviations: CKD, chronic kidney disease; AUC, area under the receiver-operating characteristic curve; BMI, body mass index; eGFR, estimated glomerular filtration rate; CVD, cardiovascular disease; LDL-C, low-density lipoprotein cholesterol; baPWV, brachial to ankle pulse-wave velocity; ECW/TBW, extracellular water to total body water ratio
We then evaluated whether fluid status can increase BP at more severe hypertension, which was defined as a 24-h SBP of ≥140 mm Hg. In the non-CKD group, the AUC for SBP ≥ 140 mm Hg did not increase when ECW/TBW was added to the conventional model. In contrast, the AUC of the ECW/TBW-based model significantly increased compared with that of Model 1 (0.733 vs. 0.709, P = 0.033) in the CKD group. Notably, a significant impact of arterial stiffness on high BP was consistently observed regardless of CKD status. The predictive power for SBP ≥ 140 mm Hg was comparable between baPWV and ECW/TBW in the CKD group (Fig. 2a, b). These findings suggest that fluid overload elevates BP at a later stage, particularly in patients with CKD.
Receiver-operating characteristic curve analysis for 24-h systolic blood pressure ≥140 mm Hg in patients with and without CKD. Notes: 1 Antihypertensive medications include angiotensin II receptor blockers, angiotensin-converting enzyme inhibitors, calcium channel blockers, β-blockers, α-blockers, and diuretics. Abbreviations: CKD, chronic kidney disease; AUC, area under the receiver-operating characteristic curve; BMI, body mass index; eGFR, estimated glomerular filtration rate; CVD, cardiovascular disease; LDL-C, low-density lipoprotein cholesterol; baPWV, brachial to ankle pulse-wave velocity; ECW/TBW, extracellular water to total body water ratio
Discrimination ability of arterial stiffness and fluid status for SBP ≥140 mm Hg according to CKD status
To confirm the differential impact of arterial stiffness and fluid overload on BP, we performed reclassification analyses using a cut-off value of 140 mm Hg. In the CKD group, NRI and IDI significantly improved after adding baPWV to Model 1. These indices also significantly improved when ECW/TBW was added to Model 1. However, in the non-CKD group, adding only baPWV to Model 1 improved its risk classification (Table 3).
These relationships were further ascertained through the RMSE and adjusted R2 calculation. In the CKD group, adding baPWV or ECW/TBW to Model 1 similarly and significantly revealed lower RMSE and higher adjusted R2 compared to Model 1, suggesting that both components improved the predictive power for high BP. In the non-CKD group, only baPWV decreased the RMSE and increased the adjusted R2 compared to Model 1 (Table 4).
Finally, we tested the interactions between CKD status and baPWV and ECW/TBW using multivariable-adjusted linear regression for 24-h SBP. There was a significant interaction between CKD status and ECW/TBW (β = 2.730, P < 0.001). However, no interaction was found between CKD status and baPWV. Thus, 24-h SBP was significantly affected by arterial stiffness irrespective of CKD status, whereas there was a differential influence of fluid overload on BP depending on CKD status (Supplemental Table 5).
Sensitivity analyses
cfPWV is often considered the gold standard variable for central arterial stiffness and predicts future cardiovascular outcomes better than baPWV [19]. Therefore, we performed a sensitivity analysis in 1386 patients with cfPWV data. The analysis showed similar findings to the baPWV-based models (Supplemental Figs. 2 and 3). We also performed an additional sensitivity analysis after excluding patients with hypertension with target organ damage in the non-CKD group because the hypertension burden is already high; thus, the vascular stiffness may be higher in high-risk patients with hypertension. The results were consistent with those of our primary analysis (Supplemental Table 6).
Subgroup analyses
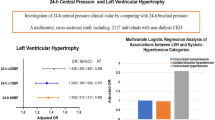
First, we further evaluated the contribution degree of arterial stiffness and fluid status to BP in subgroups stratified by age, sex, diabetes mellitus, smoking, and body mass index (BMI). Forest plots clearly showed that in all subgroups, the differential influence of ECW/TBW on BP depending on CKD status remained unaltered (Fig. 3), whereas baPWV significantly elevated BP in both groups (Fig. 4). Second, to identify the contributions of arterial stiffness and fluid overload to 24-h SBP according to CKD status, we compared the relative contribution of arterial stiffness and fluid status to 24-h SBP between CKD stage 3 and CKD stage 4. The impact of fluid overload was more evident in advanced CKD stages 4 and 5, particularly when 24-h SBP ≥140 mm Hg (Supplemental Fig. 4 and 5). Finally, we analyzed the possible association of fluid overload with nocturnal hypertension in non-dipper patients. Nocturnal hypertension was defined as a 24-h nighttime SBP ≥120 mm Hg according to the current guidelines [19]. The results showed that arterial stiffness significantly contributed to nocturnal hypertension in both non-CKD and CKD patients. However, fluid overload slightly increased the AUCs for the increased BP in CKD patients, but this did not reach statistical significance (Supplemental Figure 6).
Adjusted odds ratio for high 24-h systolic blood pressure associated with fluid status in the subgroups derived from the adjusted logistic regression analysis in patients without CKD (a) and with CKD (b). Model adjusted for age, sex, smoking history, hypertension, DM, CVD, BMI, serum LDL-C, eGFR, and baPWV. Abbreviations: OR, odds ratio; CI, confidence interval; DM, diabetes mellitus; BMI, body mass index; CKD, chronic kidney disease; CVD, cardiovascular disease; BMI, body mass index; LDL-C, low-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate; baPWV, brachial to ankle pulse-wave velocity
Adjusted odds ratio for high 24-h systolic blood pressure associated with arterial stiffness in the subgroups derived from the adjusted logistic regression analysis in patients without CKD (a) and with CKD (b). Model adjusted for age, sex, smoking history, hypertension, DM, CVD, BMI, serum LDL-C, eGFR, and ECW/TBW. Abbreviations: OR, odds ratio; CI, confidence interval; DM, diabetes mellitus; BMI, body mass index; SBP, systolic blood pressure; CKD, chronic kidney disease; CVD, cardiovascular disease; BMI, body mass index; LDL-C, low-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate; ECW/TBW, extracellular water to total body water
Discussion
We investigated the factors affecting BP in patients with and without CKD and demonstrated a consistent role of arterial stiffness in elevated BP regardless of CKD status; however, the distinct contribution of fluid status to BP was observed only in the CKD group. Moreover, the degree of influence on BP was comparable between arterial stiffness and fluid overload in the CKD group. Finally, the impact of fluid overload on high BP was more evident in more severe hypertension. Our findings are robust because we yielded the same results using various statistical models to evaluate the predictive power of each component for high BP.
The pathogenesis of hypertension is multifactorial [20]. Among the many factors associated with hypertension, we particularly focused on arterial stiffness and volume overload because these are the most important factors affecting BP and can be modulated using pharmacologic therapy. Volume overload has been undoubtedly presumed to have a substantial effect on BP. However, to date, the role of volume overload in hypertension has never been tested using objective fluid status measures. We addressed this issue for the first time using BIA to assess fluid status and substantiated the previous notion that volume factor is important in determining hypertension, particularly in patients with CKD.
Regardless of the primary etiology, an increase in peripheral vascular resistance leads to elevated BP [21]. Therefore, an important determinant of BP in patients with and without CKD. Moreover, renal dysfunction and arterial stiffness have a negative synergic effect on high BP, thus making hypertension more difficult to treat [22, 23]. On the other hand, fluid retention, the hallmark of renal insufficiency, counteracts the inherent effects of other antihypertensive medications in patients with CKD by inducing intravascular volume expansion [20]. Therefore, fluid overload, renal dysfunction, and arterial stiffness work together in a vicious cycle of uncontrolled hypertension and aggravation of kidney injury. In this study, the impact of fluid overload emerged from a higher BP and was equal to that of arterial stiffness at this late stage of hypertension. This intriguing finding is informative in managing hypertension in these patients. Resistant hypertension is highly prevalent in patients with CKD (30-40%) [24], and many physicians empirically prescribe antihypertensive medications without precisely assessing vascular health and volume status. In this regard, a stepwise approach by assessing arterial stiffness and fluid status can help us to understand potential mechanisms for increased BP as kidney function declines.
In our study, fluid overload did not contribute to hypertension in patients with normal renal function or early stage CKD. In contrast, its significant impact became evident in patients with advanced CKD stage, particularly in patients with SBP ≥140 mm Hg. Notably, meaningful fluid overload is unlikely to occur with preserved renal function because of renal-body fluid feedback system [25] and fluid overload is exacerbated as renal function deteriorates. In Guyton’s experiment using large animals and isolated perfused kidneys [26], they demonstrated that the injected fluid was retained only in cases that had ablated 70% of the renal mass. Recently, Hung SC et al. [27] showed an increased ECW volume in uninephrectomized rats than in normal rats in animal experiment and these rats became more volume overloaded by severely impaired kidney function, which was consistent with our findings (ECW/TBW from CKD stage 3–5: 0.388, 0.391, and 0.392, P for trend <0.001; data not shown). Moreover, in patients with advanced stages of CKD, the left ventricular chamber dilates and remodels in an eccentric manner and levels of proinflammatory cytokines such as interleukin-6 or tumor necrosis factor-alpha are increased [27, 28]. Such unfavorable conditions together with fluid overload can work in vicious cycle of accelerated vascular dysfunction, thus resulting in more elevated BP. All these findings taken together can explain our results, the significant impact of fluid overload on more severe hypertension in patients with advanced CKD.
Another interesting finding of our study is no significant impact of fluid overload on nighttime BP in non-dipper CKD patients. This result is consistent with previous studies in patients undergoing hemodialysis. In a study by Amar et al. [29], there was no significant difference in interdialytic weight gain according to nighttime BP pattern. In addition, Luik et al. [30] reported that fluid overload did not play a role in blunting BP differences between daytime and nighttime. On the other hand, arterial stiffness can disrupt the circadian timing system, thus resulting in the non-dipping pattern of BP and nocturnal hypertension [31, 32]. Therefore, it can be inferred that nighttime BP in non-dipper CKD patients is more affected by arterial stiffness than fluid status. Fluid retention fluctuates between day and night and is generally attenuated in the morning because approximately 80% of weight loss during nighttime is from water, not including urine or feces [33]. In this regard, it is possible that fluid retention contributes less to nocturnal hypertension.
Elderly patients with hypertension are more likely to have fluid retention [24]. However, they have low renin levels and contracted volume rather than volume expansion. Despite these, BP is well controlled by diuretics, suggesting sodium-dependent hypertension in the elderly. Arterial stiffness was more important in an elevated BP than fluid status in patients without CKD aged >60 years. Notably, arterial stiffness is a consequence of the aging process [34]. baPWV correlated well with age in patients without CKD aged >60 years (γ = 0.227, P < 0.001; data not shown) in our study, whereas ECW/TBW did not (γ = 0.002, P = 0.966, data not shown). This association was not affected by diuretic use. Therefore, attenuating arterial stiffness should be considered in resistant hypertension in elderly patients who are already treated with diuretics.
This study has distinct strengths. The data were obtained from a prospective, large-scale cohort that enrolled approximately 1500 patients. Fluid status, PWV, and 24-h ABPM data were assessed in all patients by following a standardized protocol. Therefore, these accurate measurements made our findings highly reliable. There are also important limitations. First, we used BIA to assess the volume status and did not directly measure ECW and TBW [35, 36]. Moreover, fluid overload measured by BIA cannot distinguish between true ECW increase and muscle mass decrease (i.e., lean body mass) [37, 38]. However, volumes assessed using BIA correlate well with those measured using tracer dilution methods, which are the gold standard for assessing fluid status [39]. Further, no subjects had any muscle mass depletion consistent with sarcopenia set by the Asian Working Group for Sarcopenia [40]. Second, our analysis did not incorporate the elements of vasoconstriction that may be present in patients. Unfortunately, we did not have detailed information on vasoconstrictive factors such as temperature change, caffeine intake, or other drugs that can cause vasoconstriction. However, all measurements such as PWV and bioelectrical impedance analysis were done at the same room under the same conditions and patients were instructed to avoid medications affecting vasoconstriction at least 12 h prior to the tests. Third, because this was a cross-sectional study, we could not confirm whether fluid status or arterial stiffness improvement can decrease BP. Forth, we did not have data on 24-h urine sodium excretion; thus, the effect of salt intake on BP could not be evaluated. As mentioned above, sodium sensitivity increases BP independently of volume overload. However, there is no definite diagnostic tool to test salt sensitivity accurately, and 24-h urine sodium is only a modest surrogate of sodium consumption and poorly reflects total body sodium [41, 42]. Finally, we did not analyze in detail the role of heart rate on BP although this issue is beyond our study scope. In general, increased resting heart rate can elevate BP [43, 44]. In fact, in our study, heart rate was significantly associated with BP in both non-CKD and CKD patients. Nevertheless, inclusion of heart rate in the multivariable models did not change our main findings (data not shown). Despite these limitations, our findings deserve attention because this is the first study to clarify the differential contribution of arterial stiffness and fluid status to an elevated BP using an objective fluid status measure.
In conclusion, factors affecting BP vary depending on renal function. Arterial stiffness is associated with elevated BP regardless of CKD status. Fluid overload is more influential on more severe hypertension and equally important to arterial stiffness in determining BP of patients with CKD. Thus, our findings help us to understand potential mechanisms for increased BP as kidney function declines.
References
Darabian S, Rattanasompattikul M, Hatamizadeh P, Bunnapradist S, Budoff MJ, Kovesdy CP, et al. Cardiorenal syndrome and vitamin D receptor activation in chronic kidney disease. Kidney Res Clin Pract. 2012;31:12–25.
Lee JW, Cho E, Kim MG, Jo SK, Cho WY, Kim HK. Proinflammatory CD14(+)CD16(+) monocytes are associated with vascular stiffness in predialysis patients with chronic kidney disease. Kidney Res Clin Pract. 2013;32:147–52.
Smith GL, Lichtman JH, Bracken MB, Shlipak MG, Phillips CO, DiCapua P, et al. Renal impairment and outcomes in heart failure: systematic review and meta-analysis. J Am Coll Cardiol. 2006;47:1987–96.
Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–95.
Buckalew VM Jr., Berg RL, Wang SR, Porush JG, Rauch S, Schulman G. Prevalence of hypertension in 1,795 subjects with chronic renal disease: the modification of diet in renal disease study baseline cohort. Modification of Diet in Renal Disease Study Group. Am J Kidney Dis. 1996;28:811–21.
Chiang HP, Lee JJ, Chiu YW, Tsai JC, Hung CC, Hwang SJ, et al. Systolic blood pressure and outcomes in stage 3-4 chronic kidney disease patients: evidence from a Taiwanese cohort. Am J Hypertens. 2014;27:1396–407.
Zuber K, Gilmartin C, Davis J. Managing hypertension in patients with chronic kidney disease. JAAPA. 2014;27:37–46.
Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D, et al. A risk score for predicting near-term incidence of hypertension: the Framingham Heart Study. Ann Intern Med. 2008;148:102–10.
Galis ZS, Thrasher T, Reid DM, Stanley DV, Oh YS. Investing in high blood pressure research: a national institutes of health perspective. Hypertension. 2013;61:757–61.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003;108:2154–69.
Inker LA, Astor BC, Fox CH, Isakova T, Lash JP, Peralta CA, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63:713–35.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
O’Brien E, Sheridan J, O’Malley K. Dippers and non-dippers. Lancet. 1988;2:397.
Kim JS, Kang TS, Kim JB, Seo HS, Park S, Kim C, et al. Significant association of C-reactive protein with arterial stiffness in treated non-diabetic hypertensive patients. Atherosclerosis. 2007;192:401–6.
Rajzer MW, Wojciechowska W, Klocek M, Palka I, Brzozowska-Kiszka M, Kawecka-Jaszcz K. Comparison of aortic pulse wave velocity measured by three techniques: Complior, SphygmoCor and Arteriograph. J Hypertens. 2008;26:2001–7.
McManus ML, Churchwell KB, Strange K. Regulation of cell volume in health and disease. N Engl J Med. 1995;333:1260–6.
Kocyigit I, Sipahioglu MH, Orscelik O, Unal A, Celik A, Abbas SR, et al. The association between arterial stiffness and fluid status in peritoneal dialysis patients. Perit Dial Int. 2014;34:781–90.
Minutolo R, Agarwal R, Borrelli S, Chiodini P, Bellizzi V, Nappi F, et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch Intern Med. 2011;171:1090–8.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–87.
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510–526.
Post WS, Larson MG, Levy D. Hemodynamic predictors of incident hypertension. The Framingham Heart Study. Hypertension. 1994;24:585–90.
Nagano S, Takahashi M, Miyai N, Oka M, Utsumi M, Shiba M, et al. Association of serum uric acid with subsequent arterial stiffness and renal function in normotensive subjects. Hypertens Res. 2017;40:620–4.
van Varik BJ, Vossen LM, Rennenberg RJ, Stoffers HE, Kessels AG, de Leeuw PW, et al. Arterial stiffness and decline of renal function in a primary care population. Hypertens Res. 2017;40:73–78.
De Nicola L, Gabbai FB, Agarwal R, Chiodini P, Borrelli S, Bellizzi V, et al. Prevalence and prognostic role of resistant hypertension in chronic kidney disease patients. J Am Coll Cardiol. 2013;61:2461–7.
Schrier RW, Howard RL. Unifying hypothesis of sodium and water regulation in health and disease. Hypertension. 1991;18:Iii164–168.
Guyton AC, Coleman TG, Young DB, Lohmeier TE, DeClue JW. Salt balance and long-term blood pressure control. Annu Rev Med. 1980;31:15–27.
Hung SC, Lai YS, Kuo KL, Tarng DC. Volume overload and adverse outcomes in chronic kidney disease: clinical observational and animal studies. J Am Heart Assoc. 2015;4:e001918.
Kapadia SR, Oral H, Lee J, Nakano M, Taffet GE, Mann DL. Hemodynamic regulation of tumor necrosis factor-alpha gene and protein expression in adult feline myocardium. Circ Res. 1997;81:187–95.
Amar J, Vernier I, Rossignol E, Lenfant V, Conte JJ, Chamontin B. Influence of nycthemeral blood pressure pattern in treated hypertensive patients on hemodialysis. Kidney Int. 1997;51:1863–6.
London GM, Zins B, Pannier B, Naret C, Berthelot JM, Jacquot C, et al. Vascular changes in hemodialysis patients in response to recombinant human erythropoietin. Kidney Int. 1989;36:878–82.
Li Y, Wang JG. Isolated nocturnal hypertension: a disease masked in the dark. Hypertension. 2013;61:278–83.
Rahman A, Hasan AU, Nishiyama A, Kobori H. Altered Circadian Timing System-Mediated Non-Dipping Pattern of Blood Pressure and Associated Cardiovascular Disorders in Metabolic and Kidney Diseases. Int J Mol Sci. 2018;19:E400.
Weissenberg S. Insensible water loss during sleep: a theoretical exercise. Adv Physiol Educ. 2005;29:213–5.
McEniery CM, Yasmin, Hall IR, Qasem A, Wilkinson IB, Cockcroft JR. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol. 2005;46:1753–60.
Chamney PW, Wabel P, Moissl UM, Muller MJ, Bosy-Westphal A, Korth O, et al. A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr. 2007;85:80–89.
Moissl UM, Wabel P, Chamney PW, Bosaeus I, Levin NW, Bosy-Westphal A, et al. Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas. 2006;27:921–33.
Chan C, McIntyre C, Smith D, Spanel P, Davies SJ. Combining near-subject absolute and relative measures of longitudinal hydration in hemodialysis. Clin J Am Soc Nephrol. 2009;4:1791–8.
Hur E, Usta M, Toz H, Asci G, Wabel P, Kahvecioglu S, et al. Effect of fluid management guided by bioimpedance spectroscopy on cardiovascular parameters in hemodialysis patients: a randomized controlled trial. Am J Kidney Dis. 2013;61:957–65.
Raimann JG, Zhu F, Wang J, Thijssen S, Kuhlmann MK, Kotanko P, et al. Comparison of fluid volume estimates in chronic hemodialysis patients by bioimpedance, direct isotopic, and dilution methods. Kidney Int. 2014;85:898–908.
Yamada M, Moriguch Y, Mitani T, Aoyama T, Arai H. Age-dependent changes in skeletal muscle mass and visceral fat area in Japanese adults from 40 to 79 years-of-age. Geriatr Gerontol Int. 2014;14(Suppl 1):8–14.
Felder RA, White MJ, Williams SM, Jose PA. Diagnostic tools for hypertension and salt sensitivity testing. Curr Opin Nephrol Hypertens. 2013;22:65–76.
Lerchl K, Rakova N, Dahlmann A, Rauh M, Goller U, Basner M, et al. Agreement between 24-hour salt ingestion and sodium excretion in a controlled environment. Hypertension. 2015;66:850–7.
Liu L, Mizushima S, Ikeda K, Nara Y, Yamori Y. Resting heart rate in relation to blood pressure: results from the World Health Organization-Cardiovascular Disease and Alimentary Comparison study. Int J Cardiol. 2010;145:73–74.
Gillum RF. The epidemiology of resting heart rate in a national sample of men and women: associations with hypertension, coronary heart disease, blood pressure, and other cardiovascular risk factors. Am Heart J. 1988;116:163–74.
Acknowledgements
Grant support: This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute funded by the Ministry of Health & Welfare, Republic of Korea (grant no. HI13C0715) and by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT, and Future Planning (NRF-2015R1A2A2A01007346).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Park, S., Lee, C.J., Lee, M. et al. Differential effects of arterial stiffness and fluid overload on blood pressure according to renal function in patients at risk for cardiovascular disease. Hypertens Res 42, 341–353 (2019). https://doi.org/10.1038/s41440-018-0151-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0151-0