Abstract
Objectives
To investigate visual outcomes and prognostic factors of patients with Terson syndrome (TS) managed with observation or pars plana vitrectomy (PPV).
Methods
retrospective review of medical records of 117 eyes from 81 patients (43 females) with TS. Main outcome measures were final best corrected visual acuity (BCVA), intraoperative findings and long-term sequelae.
Results
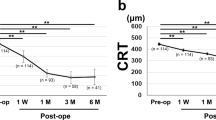
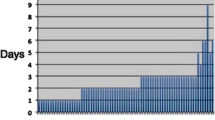
46 (39.3%) eyes were managed conservatively and 71 (60.7%) eyes underwent PPV. Median follow-up was 8.4 months. The PPV group had significantly worse (p < 0.001) baseline BCVA (median 2.3 versus 0.7 logMAR, Snellen equivalent 20/4000 versus 20/100). Final BCVA did not differ between the two groups (p = 0.38). Final BCVA ≥ 0.3 logMAR (20/40) in the surgery group was associated with post-operative retinal detachment (p = 0.013) and macular abnormalities (p = 0.014), and in the observation group with ocular comorbidity (p = 0.008). Retinal breaks were detected intraoperatively in 25 (35.2%) eyes and were associated with an interval longer than 3 months between ocular diagnosis and surgery (p = 0.04), but not with larger gauge instrumentation and posterior vitreous detachment. Incidence of ERM did not differ among patients managed conservatively and after PPV (p = 0.9) and between eyes undergoing early or delayed surgery (p = 0.09). The most common post-operative complications were cataract in 16 (22.5%) eyes and ERM in 8 (11.3%) eyes.
Conclusions
visual outcomes in TS are similar with both management strategies. Surgery allows faster and greater visual recovery but carries high risk of intraoperative retinal tears if delayed for longer than 3 months from initial presentation. ERM and retinal detachment are not correlated with timing of surgery or management strategy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Data supporting the findings of the current study are available from the corresponding author on reasonable request.
References
Litten M. Ueber Einige vom Allgemein-Klinischen Standpunkt aus Interessante Augenveränderungen. Berl Klin Wochenschr. 1881;18:23–7.
Terson A. De l’hémorrhagie dans le corps vitre au cours de l’hémorrhagie cerebrale. Clin Ophthalmol. 1900;6:309–12.
Aboulhosn R, Raju B, Jumah F, Majmundar N, Prenner J, Matin T, et al. Terson’s syndrome, the current concepts and management strategies: A review of literature. Clin Neurol Neurosurg. 2021;210:107008.
Garfinkle AM, Danys IR, Nicolle DA, Colohan AR, Brem S. Terson’s syndrome: a reversible cause of blindness following subarachnoid hemorrhage. J Neurosurg. 1992;76:766–71.
Spraul CW, Grossniklaus HE. Vitreous hemorrhage. Surv Ophthalmol. 1997;42:3–39.
Joswig H, Epprecht L, Valmaggia C, Leschka S, Hildebrandt G, Fournier JY, et al. Terson syndrome in aneurysmal subarachnoid hemorrhage - its relation to intracranial pressure, admission factors, and clinical outcome. Acta Neurochir (Wien). 2016;158:1027–36.
Medele RJ, Stummer W, Mueller AJ, Steiger HJ, Reulen H. Terson’s syndrome in subarachnoid hemorrhage and severe brain injury accompanied by acutely raised intracranial pressure. J Neurosurg. 1998;88:851–4.
Clarkson JG, Flynn HW, Daily MJ. Vitrectomy in Terson’s syndrome. Am J Ophthalmol. 1980;90:549–52.
Shaw HE, Landers MB III. Vitreous haemorrhage after intracranial haemorrhage. Am J Ophthalmol. 1975;80:207–13.
Gnanaraj L, Tyagi AK, Cottrell DG, Fetherston TJ, Richardson J, Stannard KP, et al. Referral delay and ocular surgical outcome in Terson syndrome. Retina. 2000;20:374–7.
Oyakawa RT, Michels RG, Blase WP. Vitrectomy for nondiabetic vitreous hemorrhage. Am J Ophthalmol. 1983;96:517–25.
Cochrane T, Laidlaw A. Management of unexplained vitreous haemorrhage. RCOphth Focus Winter 2014.
Garweg JG, Koerner F. Outcome indicators for vitrectomy in Terson syndrome. Acta Ophthalmol. 2009;87:222–6.
Liu X, Yang L, Cai W, Gao L, Li Y. Clinical feautures and visual prognostic indicators after vitrectomy for Terson syndrome. Eye. 2020;34:650–6.
Narayanan R, Taylor SC, Nayaka A, Deshpande R, St Aubin D, Hrisomalos FN, et al. Visual outcomes after vitrectomy for Terson syndrome secondary to traumatic brain injury. Ophthalmology. 2017;124:118–22.
Nazarali S, Kherani I, Hurley B, Williams G, Fielden M, Adatia F, et al. Outcomes of vitrectomy in Terson Syndrome. A Multicenter Canadian Perspective. Retina. 2019;00:1–6.
Mao X, You Z. 25 g compared to 20 g vitrectomy under Resight non-contact wide-angle lenses for Terson syndrome. Exp Ther Med. 2017;14:1193–7.
Kuhn F, Morris R, Witherspoon CD, Mester V. Terson syndrome. Results of vitrectomy and the significance of vitreous hemorrhage in patients with subarachnoid hemorrhage. Ophthalmol. 1998;105:472–7.
Huang Y, Tian B, Wei W. Timely vitrectomy and inner limiting membrane peeling is effective and safe for Terson syndrome with vitreous haemorrhage and sub-inner limiting membrane haemorrhage. Asia Pac J Ophthalmol (Philos). 2022;11:392–3.
Muslubas IS, Karacorlu M, Hocaoglu M, Ersoz MG, Arf S. Anatomical and functional outcomes following vitrectomy for dense vitreous haemorrhage related to Terson syndrome in children. Graefes Arch Clin Exp Ophthalmol. 2018;256:503–10.
Murjaneh S, Hale JE, Mishra S, Ling RH, Simcock PR. Terson’s syndrome: surgical outcome in relation to entry site pathology. Br J Ophthalmol. 2006;90:512–3.
Schultz PN, Sobol WM, Weingeist TA. Long-term visual outcomes in Terson syndrome. Ophthalmology. 1991;98:1814–9.
Isernhagen RD, Smiddy WE, Michels RG, Glaser BM, de Bustros S. Vitrectomy for nondiabetic vitreous haemorrhage. Not Associated Vasc Dis Retin. 1988;8:81–87.
Ehrlich R, Goh YW, Ahmad N, Polkinghorne P. Retinal breaks in small-gauge pars plana vitrectomy. Am J Ophthalmol. 2012;153:868–72.
Chen GH, Tzekov R, Jiang FZ, Mao SH, Tong YH, Li WS. Iatrogenic retinal breaks and postoperative retinal detachments in microincision vitrectomy surgery compared with conventional 20- gauge vitrectomy: a meta-analysis. Eye (Lond). 2019;33:785–95. (2019)
Ritland JS, Syrdalen P, Eide N, Vatne HO, Overgaard R. Outcome of vitrectomy in patients with Terson syndrome. Acta Ophthalmol Scand. 2002;80:172–5.
Yokoi M, Kase M, Hyodo T, Horimoto M, Kitagawa F, Nagata R. Epiretinal membrane formation in Terson syndrome. Jpn J Ophthalmol. 1997;41:168–73.
Stewart MW, Hasan SA, Collins C, Stanko C, Summer J, Brazis PW, et al. Can baseline computed tomography scans be used to identify patients at high risk of vision loss due to Terson Syndrome? Am J Ophthalmol. 2019;211:217–28.
Acknowledgements
The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Contributions
Study concept and design: EA and PS. Acquisition, analysis and interpretation of data: BG, RK, JFS. Drafting the manuscript and critical revision for important intellectual content: BG, EA, PS. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gallo, B., Khader, R., Fajardo-Sanchez, J. et al. Factors affecting anatomical and visual outcomes in Terson syndrome managed by surgery or observation. Eye (2024). https://doi.org/10.1038/s41433-024-03113-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41433-024-03113-1