Abstract
Background
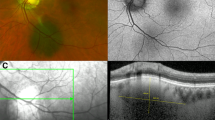
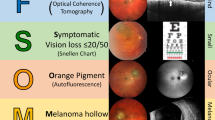
Risk factors for small choroidal melanocytic lesion growth to melanoma have been redefined using multimodal imaging. We explored provider ability to recognize risk factors for small choroidal melanocytic lesion growth to melanoma before and after image-based education and with and without multimodal imaging.
Methods
Providers were invited to participate in a survey assessing ability to identify risk factors for small choroidal melanocytic lesion growth to melanoma using either fundus imaging or multimodal imaging. Risk factors included thickness >2 mm on ultrasonography, subretinal fluid on optical coherence tomography, presence of orange pigment by autofluorescence, acoustic hollowness by ultrasonography, and diameter >5 mm by fundus imaging. Performance was assessed before and after reviewing an educational PowerPoint providing pictorial examples of risk factors. Comparison between groups was conducted using two-tailed Fisher’s exact test.
Results
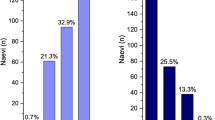
Thirty and 26 providers completed the pre-education and post-education assessments, respectively. Post-education participants were more accurate within ±1 risk factor for lesions with zero risk factors (77% vs. 100%, p = 0.01) or two risk factors (79% vs. 91%, p = 0.03). Following education, participants presented with multimodal imaging more often correctly identified lesions with four (12% vs. 42%, p = 0.03) or five (4% vs. 39%, p = 0.004) risk factors, demonstrated lower mean level of concern for lesions with zero risk factors (2.0 vs. 1.4, p < 0.001), and expressed higher level of concern for lesions with 5 risk factors (2.4 vs. 3.6, p < 0.001).
Conclusion
Use of multimodal imaging may be more beneficial than education itself to improve accuracy of risk factor identification for small choroidal melanocytic lesions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
More detailed data are not publicly available due to ethical reasons. Additional data requests can be submitted to the corresponding author. Lauren A. Dalvin, M.D. has had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
Qiu M, Shields CL. Choroidal Nevus in the United States Adult Population: Racial disparities and associated factors in the National Health and Nutrition Examination Survey. Ophthalmology 2015;122:2071–83. https://www.sciencedirect.com/science/article/pii/S0161642015005540
Kujala E, Mäkitie T, Kivelä T. Very long-term prognosis of patients with malignant Uveal Melanoma. Invest Ophthalmol Vis Sci. 2003;44:4651–9. https://doi.org/10.1167/iovs.03-0538
Eskelin S, Pyrhönen S, Summanen P, Hahka-Kemppinen M, Kivelä T. Tumor doubling times in metastatic malignant melanoma of the uvea11Received September 22, 1999. Accepted March 28, 2000.: Tumor progression before and after treatment. Ophthalmology. 2000;107:1443–9. Available from: https://www.sciencedirect.com/science/article/pii/S0161642000001822
Diener-West M, Reynolds SM, Agugliaro DJ, Caldwell R, Cumming K, Earle JD, et al. Development of metastatic disease after enrollment in the COMS trials for treatment of choroidal melanoma: Collaborative Ocular Melanoma Study Group Report No. 26. Arch Ophthalmol. 2005;123:1639–43. http://europepmc.org/abstract/MED/16344433
Shields CL, Lim LAS, Dalvin LA, Shields JA Small choroidal melanoma: detection with multimodal imaging and management with plaque radiotherapy or AU-011 nanoparticle therapy. Curr Opin Ophthalmol. 2019;30. Available from: https://journals.lww.com/co-ophthalmology/Fulltext/2019/05000/Small_choroidal_melanoma__detection_with.11.aspx
DeSimone JD, Dockery PW, Kreinces JB, Soares RR, Shields CL Survey of ophthalmic imaging use to assess risk of progression of choroidal nevus to melanoma. Eye. 2022; Available from: https://doi.org/10.1038/s41433-022-02110-6
Shields CL, Dalvin LA, Ancona-Lezama D, Yu MD, di Nicola M, Williams BKJ, et al. CHOROIDAL NEVUS IMAGING FEATURES IN 3,806 CASES AND RISK FACTORS FOR TRANSFORMATION INTO MELANOMA IN 2,355 CASES: The 2020 Taylor R. Smith and Victor T. Curtin Lecture. RETINA. 2019;39. Available from: https://journals.lww.com/retinajournal/Fulltext/2019/10000/CHOROIDAL_NEVUS_IMAGING_FEATURES_IN_3,806_CASES.2.aspx
Flanagan JPM, O’Day RF, Roelofs KA, McGuinness MB, van Wijngaarden P, Damato BE The MOLES system to guide the management of melanocytic choroidal tumours: can optometrists apply it? Clin Exp Optom. 2022;1–5. https://doi.org/10.1080/08164622.2022.2029685
Maganty N, Ilyas M, Zhang N, Sharma A. Online, game-based education for melanoma recognition: A pilot study. Patient Educ Couns. 2018;101:738–42. https://www.sciencedirect.com/science/article/pii/S073839911730602X
Goulart JM, Dusza S, Pillsbury A, Soriano RP, Halpern AC, Marghoob AA. Recognition of melanoma: A dermatologic clinical competency in medical student education. J Am Acad Dermatol. 2012;67:606–11. https://www.sciencedirect.com/science/article/pii/S0190962211022705
Roelofs KA, O’Day R, al Harby L, Arora AK, Cohen VML, Sagoo MS, et al. The MOLES system for planning management of melanocytic choroidal tumors: is it safe? Cancers. 2020;12:1311.
Salehi O, van Wijngaarden P, Keel S, Foreman J, Dirani M, Damato B, et al. Estimating malignancy risk of melanocytic choroidal tumours detected in the Australian National Eye Health Survey. Clin Exp Optom. 2021;104:854–8.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inf. 2019;95:103208.
Dalvin LA, Shields CL, Ancona-Lezama DA, Yu MD, di Nicola M, Williams Jr BK, et al. Combination of multimodal imaging features predictive of choroidal nevus transformation into melanoma. Br J Ophthalmol. 2019;103:1441. Available from: http://bjo.bmj.com/content/103/10/1441.abstract
Damato BE Can the MOLES acronym and scoring system improve the management of patients with melanocytic choroidal tumours? Eye. 2022;1–7.
Funding
This publication was made possible through the support of the Leonard and Mary Lou Hoeft Career Development Award Fund in Ophthalmology Research, Grant Number P30 CA015083 from the National Cancer Institute, and CTSA Grant Number KL2 TR002379 from the National Center for Advancing Translational Science (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
LAD and AAT were responsible for identifying the knowledge gap investigated in this manuscript, designing the survey questions, choosing representative images for both survey and review materials, determining an appropriate population to recruit from, and providing input for both data analysis and writing of this manuscript. RAC was responsible for design of pre- and post-education surveys, recruitment of participants, data analysis, drawing conclusions from the analysis, and writing of the manuscript. TYC was responsible for drawing conclusions from data analysis and contributed meaningfully to manuscript writing. OMH and AM provided feedback and impactful edits during the revision process.
Corresponding author
Ethics declarations
Competing interests
This manuscript was submitted as a poster presentation for The Association of Research in Vision and Ophthalmology 2023 Annual Meeting. This manuscript has not been published elsewhere. The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Churchill, R.A., Pecoraro, T.Y.C., Tooley, A.A. et al. Multimodal imaging risk factors predictive of small choroidal melanocytic lesion growth to melanoma: An educational study and pictorial guide. Eye 38, 798–805 (2024). https://doi.org/10.1038/s41433-023-02782-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02782-8