Abstract
The diagnosis and management of keratoconus in the paediatric age group presents additional challenges to those encountered in adults. The most significant of these, encountered in some young patients, are delayed presentation of unilateral disease, more advanced disease at diagnosis, difficulty in obtaining reliable corneal imaging, faster rates of disease progression and challenges in contact lens management. The stabilisation effect of corneal cross-linking (CXL), more extensively studied in adults with randomised trials and long-term follow-up, has been much less rigorously examined in children and adolescents. The high heterogeneity of published studies in younger patients, particularly in the choice of tomography parameters designated as primary outcome measures and the definitions of progression, indicates that improved standardisation for future studies on CXL will be necessary. There is no evidence that corneal transplant outcomes in young patients are poorer than those in adults. This review provides a current perspective on the optimal diagnosis and treatment of keratoconus in children and adolescents.
摘要
儿童年龄组圆锥角膜的诊断和治疗相较于成人面临更大的挑战。在一些年轻患者中, 最重要的是单眼患病的延迟表现、诊断时处于晚期的疾病、难以获得可靠的角膜图像、疾病进展速度快以及接触镜管理方面的挑战。通过随机试验和长期随访, 成人角膜交联术 (CXL) 的稳定作用已得到了广泛研究, 但关于儿童和青少年的研究要少得多。已发表的针对年轻患者的研究具有高度异质性, 尤其在选择指定断层扫描参数作为首要结果测定和进展定义方面, 这表明有必要改善未来CXL研究的标准化。没有证据表明年轻患者的角膜移植效果比成人更差。本综述对儿童和青少年圆锥角膜的最佳诊断和治疗提供了目前的观点。
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Liam Price, as the corresponding author have had full access to all the data in this review article and had final decision to submit for publication.
References
Torres Netto EA, Al-Otaibi WM, Hafezi NL, Kling S, Al-Farhan HM, Randleman JB, et al. Prevalence of keratoconus in paediatric patients in Riyadh, Saudi Arabia. Br J Ophthalmol. 2018;102:1436–41.
Chan E, Chong EW, Lingham G, Stevenson LJ, Sanfilippo PG, Hewitt AW, et al. Prevalence of keratoconus based on scheimpflug imaging: The raine study. Ophthalmology 2021;128:515–21.
Papali’i-Curtin AT, Cox R, Ma T, Woods L, Covello A, Hall RC. Keratoconus prevalence among high school Students in New Zealand. Cornea 2019;38:1382–9.
Godefrooij DA, de Wit GA, Uiterwaal CS, Imhof SM, Wisse RP. Age-specific incidence and prevalence of keratoconus: A nationwide registration study. Am J Ophthalmol. 2017;175:169–72.
Anitha V, Vanathi M, Raghavan A, Rajaraman R, Ravindran M, Tandon R. Pediatric keratoconus - Current perspectives and clinical challenges. Indian J Ophthalmol. 2021;69:214–25.
Pearson AR, Soneji B, Sarvananthan N, Sandford-Smith JH. Does ethnic origin influence the incidence or severity of keratoconus? Eye 2000;14:625–8.
Ferdi AC, Nguyen V, Gore DM, Allan BD, Rozema JJ, Watson SL. Keratoconus natural progression: A systematic review and meta-analysis of 11 529 eyes. Ophthalmology 2019;126:935–45.
Consejo A, Jiménez-García M, Issarti I, Rozema JJ. Detection of subclinical keratoconus with a validated alternative method to corneal densitometry. Transl Vis Sci Technol. 2021;10:32.
Olivo-Payne A, Abdala-Figuerola A, Hernandez-Bogantes E, Pedro-Aguilar L, Chan E, Godefrooij D. Optimal management of pediatric keratoconus: challenges and solutions. Clin Ophthalmol. 2019;13:1183–91.
Léoni-Mesplié S, Mortemousque B, Touboul D, Malet F, Praud D, Mesplié N, et al. Scalability and severity of keratoconus in children. Am J Ophthalmol. 2012;154:56–62.e1.
Chatzis N, Hafezi F. Progression of keratoconus and efficacy of pediatric [corrected] corneal collagen cross-linking in children and adolescents. J Refract Surg. 2012;28:753–8.
Naderan M, Rajabi MT, Zarrinbakhsh P, Farjadnia M. Is keratoconus more severe in pediatric population? Int Ophthalmol. 2017;37:1169–73.
Maharana PK, Sharma N, Vajpayee RB. Acute corneal hydrops in keratoconus. Indian J Ophthalmol. 2013;61:461–4.
Ahuja P, Dadachanji Z, Shetty R, Nagarajan SA, Khamar P, Sethu S, et al. Relevance of IgE, allergy and eye rubbing in the pathogenesis and management of Keratoconus. Indian J Ophthalmol. 2020;68:2067–74.
Weng SF, Jan RL, Wang JJ, Tseng SH, Chang YS. Association between atopic keratoconjunctivitis and the risk of keratoconus. Acta Ophthalmol. 2021;99:e54–e61.
Cavas-Martínez F, De La Cruz Sánchez E, Nieto Martínez J, Fernández Cañavate FJ, Fernández-Pacheco DG. Corneal topography in keratoconus: state of the art. Eye Vis. 2016;3:5.
Gomes JA, Tan D, Rapuano CJ, Belin MW, Ambrósio R Jr, Guell JL, et al. Global consensus on keratoconus and ectatic diseases. Cornea 2015;34:359–69.
Belin MW, Alizadeh R, Torres-Netto EA, Hafezi F, Ambrósio R Jr, Pajic B. Determining progression in ectatic corneal disease. Asia Pac J Ophthalmol (Philos). 2020;9:541–8.
Guber I, McAlinden C, Majo F, Bergin C. Identifying more reliable parameters for the detection of change during the follow-up of mild to moderate keratoconus patients. Eye Vis. 2017;4:24.
Kosekahya P, Caglayan M, Koc M, Kiziltoprak H, Tekin K, Atilgan CU. Longitudinal evaluation of the progression of keratoconus using a novel progression display. Eye Contact Lens. 2019;45:324–30.
Wisse RPL, Simons RWP, Van Der Vossen MJB, Muijzer MB, Soeters N, Nuijts RMMA, et al. Clinical evaluation and validation of the dutch crosslinking for keratoconus score. JAMA Ophthalmol. 2019;137:610.
Hashem AO, Roshdy MM, Wahba SS, Saleh MI, Elkitkat RS. Normative values of various pentacam HR parameters for pediatric corneas. Cornea 2020;39:1394–400.
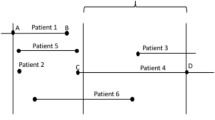
Larkin DFP, Chowdhury K, Burr JM, Raynor M, Edwards M, Tuft SJ, et al. Effect of corneal cross-linking versus standard care on keratoconus progression in young patients: The KERALINK randomized controlled trial. Ophthalmology 2021;128:1516–26.
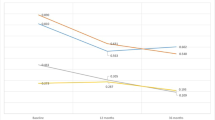
Gore DM, Leucci MT, Koay SY, Kopsachilis N, Nicolae MN, Malandrakis MI, et al. Accelerated pulsed high-fluence corneal cross-linking for progressive keratoconus. Am J Ophthalmol. 2021;221:9–16.
O’Brart D, Zarei-Ghanavati M, Vasquez-Perez A, Liu C. Comment on: “What are the costs, capacity, and clinical implications of “waiting for documented progression” in young West of Scotland patients prior to collagen cross linking?”. Eye. 2022;36:1512.
Maile H, Li J-PO, Gore D, Leucci M, Mulholland P, Hau S, et al. Machine learning algorithms to detect subclinical keratoconus: systematic review. JMIR Med Inform. 2021;9:e27363.
Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–7.
Hayes S, Boote C, Kamma-Lorger CS, Rajan MS, Harris J, Dooley E, et al. Riboflavin/UVA collagen cross-linking-induced changes in normal and keratoconus corneal stroma. PLoS ONE. 2011;6:e22405.
Wollensak G. Histological changes in human cornea after cross-linking with riboflavin and ultraviolet A. Acta Ophthalmologica. 2010;88:e17–e8.
Kobashi H, Hieda O, Itoi M, Kamiya K, Kato N, Shimazaki J, et al. Corneal cross-linking for paediatric keratoconus: A systematic review and meta-analysis. J Clin Med. 2021;10:2626.
Meyer JJ, Gokul A, Vellara HR, McGhee CNJ. Progression of keratoconus in children and adolescents. Br J Ophthalmol. 2023;107:176–80
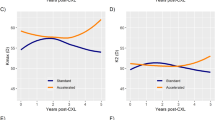
Baenninger PB, Bachmann LM, Wienecke L, Thiel MA, Kaufmann C. Pediatric corneal cross-linking: Comparison of visual and topographic outcomes between conventional and accelerated treatment. Am J Ophthalmol. 2017;183:11–6.
Kobashi H, Tsubota K. Accelerated versus standard corneal cross-linking for progressive keratoconus: A meta-analysis of randomized controlled trials. Cornea 2020;39:172–80.
Henriquez MA, Hernandez-Sahagun G, Camargo J, Izquierdo L Jr. Accelerated epi-on versus standard Epi-Off corneal collagen cross-linking for progressive keratoconus in pediatric patients: Five years of follow-up. Cornea 2020;39:1493–8.
Achiron A, El-Hadad O, Leadbetter D, Hecht I, Hamiel U, Avadhanam V, et al. Progression of Pediatric Keratoconus After Corneal Cross-Linking: A Systematic Review and Pooled Analysis. Cornea. 2022;41:874–8.
Simantov I, Or L, Gazit I, Dubinsky-Pertzov B, Zadok D, Pras E, et al. Seven years follow-up of corneal cross-linking (CXL) in pediatric patients: Evaluation of treated and untreated eye. Eur J Ophthalmol. 2022;32:1482–90.
Ahmad TR, Pasricha ND, Rose-Nussbaumer J, J TO, J MS, Indaram M. Corneal collagen cross-linking under general anesthesia for pediatric patients with keratoconus and developmental delay. Cornea 2020;39:546–51.
Kanellopoulos AJ, Vingopoulos F, Sideri AM. Long-term stability with the athens protocol (Topography-Guided Partial PRK Combined With Cross-Linking) in pediatric patients with keratoconus. Cornea 2019;38:1049–57.
Downie LE, Lindsay RG. Contact lens management of keratoconus. Clin Exp Optom. 2015;98:299–311.
Jones-Jordan LA, Walline JJ, Mutti DO, Rah MJ, Nichols KK, Nichols JJ, et al. Gas permeable and soft contact lens wear in children. Optom Vis Sci. 2010;87:414–20.
Alipour F, Jamshidi Gohari S, Azad N, Mehrdad R. Miniscleral contact lens in pediatric age group: indications, safety, and efficacy. Eye Contact Lens. 2021;47:408–12.
Severinsky B, Lenhart P. Scleral contact lenses in the pediatric population-Indications and outcomes. Cont Lens Anterior Eye. 2022;45:101452.
Alfonso JF, Fernández-Vega-Cueto L, Lisa C, Monteiro T, Madrid-Costa D. Long-term follow-up of intrastromal corneal ring segment implantation in pediatric keratoconus. Cornea 2019;38:840–6.
Mendez EA, Roys N, Mejia ME, Plata MC, Rosenstiehl SM. Results of follow-up in pediatric keratoconus treated with intracorneal ring segments implantation alone or in combination with corneal cross-linking. J Pediatr Ophthalmol Strabismus. 2022;59:118–27.
Kelly T-L. Corneal transplantation for keratoconus. Arch Ophthalmol. 2011;129:691.
Wajnsztajn D, Hopkinson CL, Larkin DFP. National health service b, transplant ocular tissue advisory g, contributing o. keratoplasty for keratoconus in young patients: demographics, clinical features, and post-transplant outcomes. Am J Ophthalmol. 2021;226:68–75.
Feizi S, Javadi MA, Karimian F, Abolhosseini M, Moshtaghion SM, Naderi A, et al. Penetrating keratoplasty versus deep anterior lamellar keratoplasty in children and adolescents with keratoconus. Am J Ophthalmol. 2021;226:13–21.
Acknowledgements
Supported in part by the National Institute for Health Research (NIHR) Efficacy and Mechanism Evaluation Programme (reference. [14, 18, 23]), an MRC and NIHR partnership. The trial was otherwise supported in part by the NIHR Moorfields Biomedical Research Centre and NIHR Moorfields Clinical Research Facility. The funding organisation had no role in design or conduct of this research.
Funding
This review article received no specific funding.
Author information
Authors and Affiliations
Contributions
L.P. and D.L. had equal involvement in producing this manuscript in all of the following criteria: 1. Conceived and/or designed the work that led to the submission, acquired data, and/or played an important role in interpreting the results. 2. Drafted or revised the manuscript. 3. Approved the final version. 4. Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Price, L.D., Larkin, D.F.P. Diagnosis and management of keratoconus in the paediatric age group: a review of current evidence. Eye 37, 3718–3724 (2023). https://doi.org/10.1038/s41433-023-02600-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02600-1