Abstract
Purpose
Fellow eyes of patients with unilateral neovascular age-related macular degeneration (nAMD) are at risk of developing macular neovascularisation (MNV). These eyes may first develop subclinical non-exudative MNV (neMNV) before they leak to form exudative MNV (eMNV). The EYE NEON study is a 2-year study aimed at estimating the prevalence and incidence of neMNV and evaluating its role as a predictor for conversion to neovascular AMD.
Methods
EYE NEON is a multicentre study that will run in retinal clinics across 25 National Health Service with the aim to recruit 800 patients with new onset nAMD in the first eye. The fellow-eye with no evidence of nAMD at baseline will be the study eye. All study eyes will have OCT and OCTA done at first and second year following first anti-VEGF treatment to the first eye (non-study eye), with new onset nAMD. We will estimate the prevalence and incidence of neMNV over 2 years, rate of conversion from neMNV to eMNV and numbers initiated on treatment for neovascular AMD in the study eye will be reported. Predictive models of conversion including neMNV with other demographic and imaging parameters will be developed.
Conclusion
The study design with proposed target sample size is sufficient to evaluate the retinal imaging characteristics of the study eyes with and without neMNV and develop predictive models to inform risk of conversion to nAMD.
Similar content being viewed by others
Introduction
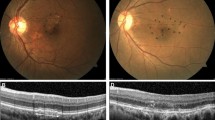
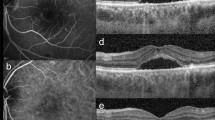
Active new onset neovascular age-related macular degeneration (nAMD) is characterized by the presence of macular neovascularisation (MNV) that leak fluid and/or blood. Exudation from MNV responds to anti-vascular endothelial growth factor (anti-VEGF) agents [1]. Nevertheless, prevention of conversion of fellow eyes with high-risk intermediate AMD to neovascular AMD with quarterly intravitreal injections of anti-VEGF agents has failed to show any benefit [2, 3]. On average, the risk of development of MNV in fellow eye increases at the rate of about 10% per year [4,5,6]. However, there is significant variations in the incidence of MNV in fellow eyes [7,8,9,10]. Therefore, intermediate AMD in the fellow eye per se is not sufficient to predict conversion. One marker of conversion identified on optical coherence tomography (OCT) is the presence or new onset double layer sign (DLS) defined as a localized separation of the retinal pigment epithelium from the Bruch’s membrane [11,12,13]. Some of these DLS fit the criterion of shallow, irregular retinal pigment epithelial elevation (SIRE) (defined as greatest transverse linear dimension of 1000μm or more, an irregular RPE layer with a height of predominantly less than 100 μm, and a nonhomogeneous internal reflectivity [14, 15]. In addition, some of these DLS may harbor subclinical non-exudative MNV (neMNV) detected by OCT-angiography (OCTA) and this sign may more accurately predict conversion to neovascular AMD compared to DLS without neMNV [16, 17]. The incidence and prevalence of neMNV is unclear with reports from studies with small sample sizes indicating ranges from 6 to 60% [17,18,19,20,21,22] at varying timepoints. It is also unclear whether any morphological features of neMNV may further aid the prediction of conversion to eMNV. Risk models for conversion to neovascular AMD need to be developed.
Objective
The primary objective of the study is to quantify the prevalence of neMNV in fellow eyes (study eyes) of patients with new onset unilateral neovascular AMD (non-study eye). Secondary objectives include estimating the incidence of neMNV over 2 years in study eyes, descriptive analysis of eyes with and without neMNV and developing a risk model for conversion to neovascular AMD incorporating both demographic and retinal imaging features over 2 years.
Study design
This multi-center cohort study was approved by London-City and East research ethics committee (REC reference 20/PR/0897) and will recruit ~800 patients with new onset unilateral nAMD that have been initiated on anti-VEGF therapy. This will include a retrospective cohort who were initiated on first anti-VEGF therapy in non-study eye not more than 15 months prior to date of consent to this study. The prospective cohort will include patients with new onset unilateral nAMD who will provide consent on date of first anti-VEGF agent. In both cohorts, there should be no evidence of any exudation due to nAMD in the fellow (study) eyes. They will be followed up for 2 years. Year 1 and 2 will be calculated from date of first anti-VEGF injection received in non-study eye.
Study population
It is anticipated that the study will run across 25 different National Health Service sites in the UK. Patients are eligible for the study if they are aged between ≥50 years and ≤100 years and have a diagnosis of unilateral treatment naïve exudative neovascular AMD at baseline and initiated on anti-VEGF therapy. The fellow eye is the study eye and may have any stage of non-neovascular AMD (early or intermediate AMD or geographic atrophy). The study eye had to have adequate media clarity, pupillary dilation, and patient cooperation for capturing OCT and OCTA imaging. The exclusion criteria included treatment initiation for unilateral neovascular AMD more than 15 months prior to recruitment, advanced AMD in the study eye (geographic atrophy or neovascular AMD or any other ocular condition that, in the opinion of the investigator, might affect or alter visual acuity during the course of the study. Other exclusion criteria included any patient who has opted out of their information being used for research nationally or locally at any site, study eyes treated with anti-VEGF for other causes of MNV or patients participating in a clinical trial with an ophthalmic experimental therapy.
Study procedures and schedule of assessments
All patients will provide consent to participate in the study. For the retrospective cohort, the baseline data and retinal images obtained during routine care will be collected and then prospectively imaged as per study protocol for their year 1 and 2 visits. The prospective cohort will have retinal images captured as per study protocol at all 3 visits. Participating sites will capture OCT and OCTA images with devices available in their clinics. The majority of the clinics have Spectralis OCT/HRA + OCT (Heidelberg Engineering, Germany), with software version 6.12.x.x). During all the study visits, OCT macula volume Scan: 20° × 20° (5.9 mm × 5.9 mm) with 97 Sections, High Speed, 15 Frames (Automated Realtime Averaging-ART) will be obtained. For OCTA, ideally two scans are preferred with one high resolution 10° scan (HR10): dense preset volume scan, 512 B-Scans: 10° × 10°, 512 Sections, 5 Frames (ART) and the other is high speed 20° scan (HS20): dense preset volume scan, 512 B-Scans: 20° × 20°, 512 Sections, 5 Frames (ART). If the patient is not compliant, at least HS 20° is required. The follow up images for year 1 and 2 must be acquired using the follow up mode. The scans should also meet the quality criteria of excellent signal strength (>30 dB) with correct positioning of the scan pattern centered at fovea. For those sites that obtain TRITON OCTA, Topcon 3D OCT-1000 or Topcon OCT-2000 series with version 11.1 or higher will be used. All the study visits required OCT 3D macula 7 × 7 mm cube scan and OCTA 6 × 6 mm cube scans.
Data collection, export and management
Data collected from baseline visit include visual acuity for both eyes, date of first injection in non-study eye, routine demographic data of age, gender, smoking history, and OCT and OCTA images. The baseline OCT of the non-study eye was also collected to confirm evidence of neovascular AMD. If OCTA was not captured at baseline as per routine care for the retrospectively collected data, it will be done within the first year of treatment to non-study eye. Visual acuity, OCT and OCTA images at year 1 and 2 have to be captured and collected within a window of ±3 months at year 1 and 2.
All study data will be handled in accordance with the Data Protection Act 2018 and General Data Protection Regulation (GDPR). The data collection tool for this study will be through an electronic data capture (EDC) system (Playon Ltd, Bengaluru, India). All access to the EDC system is through a password-protected security system. The patient identification number (PIN) will be generated by the EDC and no patient identifiable data will be entered in the database. The retinal images from the participating sites will be transferred to Moorfields Eye through encrypted NHS mail large file transfer service. For sites that do not have access to NHS mail, data will be transferred on an encrypted USB stick via courier. The retinal images will be first reviewed for data quality and study eligibility. The images will be graded by trained retinal fellows in Moorfields using a detailed grading format. Each retinal fellow will grade 50 test images and inter-grader agreement of a random 10% of OCT and OCTA images will be reported.
Safety reporting
All adverse events and serious adverse events related to this project in terms of image capture will be collected and reported. The OCT and OCTA are non-invasive diagnostic techniques that utilize reflected light waves. There are no known side effects or complications related to these assessments.
Statistical considerations
Sample size calculation: due to the nature of this epidemiological study, there is no (confirmatory) hypothesis testing foreseen. The study size is based on achieving sufficient precision for prevalence of neMNV and conversion from neMNV to nAMD. The recommended number of patients is ~800 patients in total. The primary objective is to understand the prevalence of neMNV. Table 1 shows several scenarios for prevalence, ranging from 5 to 70%. While the literature is limited, we expect an overall prevalence of neMNV of 20–40%. Calculations were performed using nQuery + nTermin 4.0.
For estimating conversion from neMNV to nAMD, based on assumptions of patients diagnosed with neMNV and participation rates, we expect that 150–200 patients will have follow-up data. Both scenarios are considered in Table 2. While the literature is limited, we expect an overall conversion of neMNV to nAMD of 40–60% in 24 months. Those rows are highlighted in gray. Calculations were performed using nQuery + nTermin 4.0.
Based on the above scenarios, the recommended number of patients is about 800 in total is sufficient to achieve adequate precision for both prevalence and conversion estimates.
Statistical analysis
At baseline, we will report the prevalence of neMNV in study eyes of patients with nAMD in the non-study eye when first initiated on anti-VEGF therapy. We will compare the correlates of having neMNV diagnosis or not in the study eye at baseline. At follow-up, we will report the percent of neMNV eyes who converted to nAMD. These will include patients who have been graded as nAMD on OCT and OCTA and those initiated on anti-VEGF treatment. Cumulative incidence will be reported and time to event may be plotted. For risk models, we will evaluate risk factors that determine conversion. Subgroup analysis may be done based on duration from diagnosis of nAMD in non-study eye, first record of neMNV and other key baseline demographic and clinical characteristics.
Outcomes
The primary outcome is to estimate the prevalence of neMNV in the study eye of patients with a diagnosis of nAMD in the first eye on the first anti-VEGF injection visit. Secondary outcomes include reporting the incidence of neMNV over the period of 2 years; conversion rate to nAMD at 1 and 2 years with and without neMNV; demographic and baseline retinal risk factors associated with converting from neMNV (as diagnosed at baseline) to nAMD during follow-up; the diagnostic accuracy of DLS, SIRE and other imaging markers to detect neMNV; changes in visual acuity during follow-up; survival analysis of time to occurrence of DLS, conversion of DLS to neMNV and neMNV to eMNV. For predictive models for neMNV and eMNV, we will evaluate risk factors for faster/slower time to progression or conversion. Subgroup analysis may be done based on other key baseline characteristics. A detailed statistical analysis plan will be developed.
Trial management and monitoring
The trial management group (TMG) consisting of Chief Investigator, associate principal investigator, sub-Investigators, trial manager and other delegates of the group, will oversee the setting up and conduct of the study. The TMG will regularly review quality of images to assess need for further training.
Discussion
This study is aimed to address the gap in knowledge on the prevalence and incidence of neMNV in study (fellow eyes) of people with nAMD. As fellow eyes of unilateral nAMD are at higher risk of conversion than eyes with bilateral intermediate AMD, we included this group of patients to achieve a higher event rate. Most studies on neMNV in AMD have limited sample sizes [17,18,19,20,21,22]. The strength of this study is the large sample size allowing at least a quarter of the patients to have 2-year data to accurately provide the incidence data of neMNV in unilateral nAMD patients. Previous studies have relied on DLS or SIRE as a surrogate marker of neMNV. The use of OCTA to confirm neMNV in eyes with DLS or SIRE in this study is another strength of this study.
Our definition of conversion to eMNV includes both OCT evidence of any macular fluid as well as initiation of anti-VEGF injection in the fellow eye. This is to avoid small new pockets of subretinal fluid or tiny intraretinal cysts to be mis-represented as conversion.
We also aim to look at the diagnostic accuracy of the DLS and to provide descriptive features of a DLS that has a neMNV [4,5,6,7,8].
The strengths of the study are the sample size that is expected to provide sufficient event rate to develop predictive models on risk of conversion and that OCTA is used to confirm neMNV in all visits.
The main limitation of the study design is that we have only three timepoints within 2 years when OCT and OCTA will be assessed. Therefore, the exact time of conversion cannot be estimated.
Summary
What was known before
-
Subclinical non-exudative macular neovascularisation (neMNV) detected by OCTA may be present before an eye converts to neovascular AMD. But the incidence and prevalence of neMNV is unclear. Moreover, it is also unclear whether it is the strongest predictor for conversion to neovascular AMD.
What this study adds
-
Evaluating the OCT and OCTA images captured from fellow eyes of patients over 2 years from date of first anti-VEGF injection for unilateral neovascular AMD will provide both the prevalence and incidence of neMNV and the time to conversion to eMNV. Predictive models incorporating new imaging characteristics such as neMNV may provide more information on whether neMNV is indeed a risk factor for conversion of neovascular AMD.
References
Scott AW, Bressler SB. Long-term follow-up of vascular endothelial growth factor inhibitor therapy for neovascular age-related macular degeneration. Curr Opin Ophthalmol. 2013;24:190–6.
Heier JS, Brown DM, Shah SP, Saroj N, Dang S, Waheed NK, et al. Intravitreal aflibercept injection vs sham as prophylaxis against conversion to exudative age-related macular degeneration in high-risk eyes: a randomized clinical trial. JAMA Ophthalmol. 2021;139:542–7.
Chan CK, Lalezary M, Abraham P, Elman M, Beaulieu WT, Lin SG,PREVENT Study Group, et al. Prophylactic ranibizumab to prevent neovascular age-related macular degeneration in vulnerable fellow eyes: a randomized clinical trial. Ophthalmol Retin. 2022;6:484–94.
Risk factors for choroidal neovascularization in the second eye of patients with juxtafoveal or subfoveal choroidal neovascularization secondary to age-related macular degeneration. Macular Photocoagulation Study Group. Arch Ophthalmol. 1997;115:741–7.
Solomon SD, Jefferys JL, Hawkins BS, Bressler NM. Incident choroidal neovascularization in fellow eyes of patients with unilateral subfoveal choroidal neovascularization secondary to agerelated macular degeneration: SST report No. 20 from the Submacular Surgery Trials Research Group. Arch Ophthalmol. 2007;125:1323–30.
van Leeuwen R, Klaver CC, Vingerling JR, Hofman A, de Jong PT. The risk and natural course of age-related maculopathy: follow-up at 6 1/2 years in the Rotterdam study. Arch Ophthalmol. 2003;121:519–26.
Five-year follow-up of fellow eyes of patients with age-related macular degeneration and unilateral extrafoveal choroidal neovascularization. Macular Photocoagulation Study Group. Arch Ophthalmol. 1993;111:1189–99.
Cascella R, Strafella C, Caputo V, Errichiello V, Zampatti S, Milano F, et al. Towards the application of precision medicine in age-related macular degeneration. Prog Retin Eye Res. 2018;63:132–46.
Cascella R, Strafella C, Longo G, Ragazzo M, Manzo L, De Felici C, et al. Uncovering genetic and non-genetic biomarkers specific for exudative age-related macular degeneration: significant association of twelve variants. Oncotarget. 2018;9:7812–21.
Hallak JA, de Sisternes L, Osborne A, Yaspan B, Rubin DL, Leng T. Imaging, genetic, and demographic factors associated with conversion to neovascular age-related macular degeneration: secondary analysis of a randomized clinical trial. JAMA Ophthalmol. 2019;137:738–44.
Hagag AM, Rasheed R, Chandra S, Jeffery G, Sivaprasad S. The diagnostic accuracy of double-layer sign in detection of macular neovascularization secondary to central serous chorioretinopathy. Am J Ophthalmol. 2022;236:271–80.
Sheth J, Anantharaman G, Chandra S, Sivaprasad S. “Double-layer sign” on spectral domain optical coherence tomography in pachychoroid spectrum disease. Indian J Ophthalmol. 2018;66:1796–801.
Shi Y, Motulsky EH, Goldhardt R, Zohar Y, Thulliez M, Feuer W, et al. Predictive value of the OCT double-layer sign for identifying subclinical neovascularization in age-related macular degeneration. Ophthalmol Retin. 2019;3:211–9.
Narita C, Wu Z, Rosenfeld PJ, Yang J, Lyu C, Caruso E, et al. Structural OCT signs suggestive of subclinical nonexudative macular neovascularization in eyes with large drusen. Ophthalmology. 2020;127:637–47.
Chen L, Messinger JD, Sloan KR, Swain TA, Sugiura Y, Yannuzzi LA, et al. Nonexudative macular neovascularization supporting outer retina in age-related macular degeneration: a clinicopathologic correlation. Ophthalmology. 2020;127:931–47.
Querques G, Srour M, Massamba N, Georges A, Ben Moussa N, Rafaeli O, et al. Functional characterization and multimodal imaging of treatment-naive “quiescent” choroidal neovascularization. Invest Ophthalmol Vis Sci. 2013;54:6886–92.
de Oliveira Dias JR, Zhang Q, Garcia JMB, Zheng F, Motulsky EH, Roisman L, et al. Natural history of subclinical neovascularization in nonexudative age-related macular degeneration using swept-source OCT angiography. Ophthalmology. 2018;125:255–66.
Palejwala NV, Jia Y, Gao SS, Liu L, Flaxel CJ, Hwang TS, et al. Detection of nonexudative choroidal neovascularization in age-related macular degeneration with optical coherence tomography angiography. Retina. 2015;35:2204–11.
Yanagi Y, Mohla A, Lee WK, Lee SY, Mathur R, Chan CM, et al. Prevalence and risk factors for nonexudative neovascularization in fellow eyes of patients with unilateral age-related macular degeneration and polypoidal choroidal vasculopathy. Invest Ophthalmol Vis Sci. 2017;58:3488–95.
Roisman L, Zhang Q, Wang RK, Gregori G, Zhang A, Chen CL, et al. Optical coherence tomography angiography of asymptomatic neovascularization in intermediate age-related macular degeneration. Ophthalmology. 2016;123:1309–19.
Heiferman MJ, Fawzi AA. Progression of subclinical choroidal neovascularization in age-related macular degeneration. PLoS ONE. 2019;14:e0217805.
Capuano V, Miere A, Querques L, Sacconi R, Carnevali A, Amoroso F, et al. Treatment-naïve quiescent choroidal neovascularization in geographic atrophy secondary to nonexudative age related macular degeneration. Am J Ophthalmol. 2017;182:45–55.
Acknowledgements
EYENEON study group.
Funding
Boehringer Ingelheim International GmbH, Germany.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: ST, SC, SG, AnG and SS; Funding acquisition: AnG, TCNY, EC, SS, SC and SG; Methodology: SC, SG, ST, AnG and SS; Project administration: AnG, ST, TCNY, WST, EC and SS; Resources: EYENEON study group, ST, SC and SS; Supervision: SS; Visualization: ST and SS; Writing—original draft: ST and SS; Writing—review and editing: AnG, TCNY, EC, WST, SC and SS; Review and approval of final manuscript: ST, SC, SG, WST, AG, EC, TCNY and SS.
Corresponding author
Ethics declarations
Competing interests
SS has received funding/fees from Bayer, Novartis, Allergan, Roche, Boehringer Ingelheim, Optos, Oxurion, Oculis, Biogen, Eyebiotech and Apellis and is a trial steering committee member for FOCUS study (Novo Nordisk).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thottarath, S., Chandra, S., Gurudas, S. et al. Study protocol on prevalence of non-exudative macular neovascularisation and its contribution to prediction of exudation in fellow eyes with unilateral exudative AMD (EYE-NEON). Eye 37, 3004–3008 (2023). https://doi.org/10.1038/s41433-023-02460-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02460-9
This article is cited by
-
Optical Coherence Tomography Angiography: A 2023 Focused Update on Age-Related Macular Degeneration
Ophthalmology and Therapy (2024)
-
Biomarkers for the Progression of Intermediate Age-Related Macular Degeneration
Ophthalmology and Therapy (2023)