Abstract
Lentigo Maligna is a benign subtype of melanoma in situ and can progress to lentigo maligna melanoma, which is invasive. Complete surgical excision is the gold standard of treatment but requires large margins. If affecting the peri-ocular region, surgical excision leads to extensive defects, complex reconstructions, and functional impairment of the protection of the ocular surface. Here we review the reported literature about the use of Imiquimod 5% topical cream for lentigo maligna of the eyelid, the treatment outcomes, side effects and tolerance. In addition, the side effects of imiquimod treatment of non-LM lesions are described to help better inform the decision-making process. Treatment for peri-ocular Lentigo maligna showed a 56–86% complete treatment response and a 90% tolerability rate. However, reported treatment protocols vary and histopathological confirmation of clearance was only obtained in 56%. Further studies are required to determine the optimal treatment protocol to maximise clearance rates. Overall, Imiquimod was well tolerated in the peri-ocular area.
摘要
雀斑样痣为原位黑色素瘤的良性亚型, 可进展为具有侵袭性的雀斑样恶性黑色素瘤。完全手术切除是治疗雀斑样痣的金标准, 但手术需要较大的切缘。如果累及眼周区域, 手术切除会导致眼表保护屏障的广泛缺损, 复杂重建和功能损坏。本文我们回顾分析了与5%咪喹莫特外用乳膏治疗睑缘雀斑样痣的治疗效果、副作用和耐受性相关的已发表文献。此外, 我们报道了咪喹莫特治疗非雀斑样痣的副作用, 以便更好地辅助临床决策。咪喹莫特治疗眼周雀斑样痣后, 有56–86%的病人表现出完全缓解, 90%的病人表现为耐受。然而, 研究报道的治疗方案多种多样, 且组织病理学证实仅有56%的雀斑样痣被彻底清除。为了使清除率最大化, 研究者需要进一步探索来确定最佳治疗方案。总之, 咪喹莫特在眼周区域耐受良好。
Similar content being viewed by others
Introduction
Lentigo Maligna (LM) is a subtype of melanoma in situ and can progress to lentigo maligna melanoma (LMM). Surgical excision is the gold standard of treatment. However, there can be a large non-pigmented area of the lentigo maligna lesion, which is not clinically apparent on inspection alone. On top of this, surgical clearance frequently requires more than 5 mm margins which leads to extensive defects, complex reconstructions, and high morbidity. Treatment alternatives are required in patients with extensive areas involved or who decline surgical treatment. Imiquimod 5% cream is licensed for treatment of genital warts, actinic keratosis and superficial basal cell carcinomas. Its off-label use is common for non-periocular lentigo maligna. Use on the eyelids is not recommended due to possible side effects to the ocular surface. However, its use in the periocular area has been reported. Here, we therefore review the reported literature about the use of Imiquimod 5% topical cream for lentigo maligna of the eyelids, the treatment outcomes, side effects and tolerance. In addition, the side effects of imiquimod treatment of periocular non-LM lesions are described to help better inform the decision-making process.
Lentigo maligna
LM is a subtype of melanoma in situ. It is most prevalent in the elderly, fair skinned population. It typically arises as a slowly progressive, variably pigmented macule in sun-damaged skin [1, 2]. In about 78% cases, it is located in the head and neck area [3]. The incidence of LM appears to be significantly rising over recent decades, for example, the age standardised incidence rate for LM has increased from 0.72 to 3.84 per 100,000 person-years from 1989 to 2013 in the Netherlands, while in Denmark it rose from 2.6 to 8.1 cases in women and from 1.4 to 5.6 in men from 1997 to 2011 [4,5,6].
While LM is benign, it has the potential to progress to invasive disease which is called LMM [1, 7]. LMM has the same prognosis and risk of metastasis and mortality as invasive melanoma [7]. The true progression rate of LM to LMM is unknown. Weinstock and Sober reported a risk of 3.3% for developing LMM by the age of 75 if LM was diagnosed at age 45 compared to a risk of 1.2% if LM was diagnosed at age 65 [8]. A more recent study from 2016 found that the cumulative incidence of LMM after 25-year follow-up was 2.0% for males and 2.6% for females in 10,545 patients with LM [4]. The risk may be underreported as areas of invasion, which were seen in 16% on histopathological examination in a study by Agarwal-Antal et al., may be missed due to low clinical suspicion and lack of biopsy [9]. On the other hand, LM itself is underreported, probably to a greater degree.
To prevent transformation to invasive LMM, the current interdisciplinary European Consensus Guidelines from 2019 recommend complete surgical excision of LM as first-line management. Staged excision has been shown to have higher clearance and less recurrences than wide excision [9]. Mohs micrographic surgery with staged excision (often called “slow Mohs”) is reported to show the lowest rate of recurrence with 0.3% after 5 years and 2.2% after 10 years [10, 11].
Unfortunately, due to subclinical spread (with non-pigmented area involvement) and the difficulty of histological differentiation of LM from background atypical melanocytic hyperplasia, the standard surgical margins for clearance are insufficient [12, 13]. Multiple studies have demonstrated that a 5 mm margin is not adequate [9, 11, 14]. Kunishige et al. found 86% of LM was cleared with 6 mm margins while 9 mm margins were necessary to achieve a complete excision of 98.7% of LM [10]. Malhotra et al. reviewed mapped serial excisions in 141 cases of LM and LMM. 31% of lesions required more than 5 mm margins and 14% more than 10 mm margins for complete excision. Of these cases, 19% were involving the periocular area [15].
As LM predominantly affects the head and neck region, this extensive surgery can lead to severe cosmetic and functional impairment with associated morbidity, and clearance may be unachievable [12].
Especially in the periocular region, clearance can be exceptionally difficult and impair the most important function of the eyelids, ocular surface protection. Complex reconstructions with the aim to restore eyelid function may be required. Primary acquired melanosis (PAM) of the conjunctiva may be associated as a spillover disease and furthermore complicate clearance by surgery. When LM is located on the eyelids, it is likely that a greater proportion of patients refuse this surgery due to the eyelids’ critical function in maintaining sight and the highly noticeable location in the centre of the face. Furthermore, patients with co-morbidities may be unsuitable for surgery.
For these reasons, non-surgical management options are needed. The alternatives include cryotherapy, radiotherapy and topical Imiquimod.
Imiquimod for LM
Imiquimod is a topical immune response modifier of the imidazoquinolone drug family [16]. It stimulates the innate and acquired immune pathways which lead to recognition and destruction of viral infected or tumour cells in the skin [17].
The effects of imiquimod are mediated through Toll-like receptors 7 and 8 on cells of the immune system that lead to the release of cytokines and other mediators that trigger an inflammatory cascade [18, 19]. Imiquimod also leads to interferon-gamma production from T helper (Th)-1 cells that stimulate cytotoxic T lymphocytes for a cellular immune response [17, 18]. In addition, Imiquimod may induce tumour cell specific apoptosis independent of membrane-bound death receptors [7, 18].
Imiquimod 5% cream (AldaraTM) has shown efficacy and is licensed in the UK (United Kingdom) and US for the treatment of many conditions including genital warts (three times a week for up to 16 weeks), actinic keratosis (three times a week for one or two 4-week courses, with a 4-week gap) and superficial basal cell carcinoma (five times a week for 6 weeks, applied to the lesion and 1 cm around it), when other treatments cannot be used [20]. The treatment of LM with Imiquimod 5% topical cream in non-periocular areas is off label but commonly used [7]. A common treatment regime for non-periocular areas is once a day for 60 days.
The 2019 guidelines for the management of primary cutaneous melanoma from the American Academy of Dermatology state that topical imiquimod 5% cream may be used as second-line treatment for melanoma in situ, of LM type, when surgery is not possible or when optimal surgery has already been performed (adjuvant). They recommend careful discussion of the associated risks, benefits, and uncertainties of non-surgical treatment [21].
Results of response and recurrence vary due to different treatment regimes, assessment of outcome and duration of follow up. Reports about complete histopathological clearance vary from 37 to 92% [22, 23]. However, Imiquimod treatment protocols are highly variable between published studies. More intensive treatment protocols with multiple applications per week (more than 60 times over 12 weeks) show greater odds of histological clearance [24].
In 2017 Tio et al. systematically reviewed 26 case reports, 11 retrospective studies, 3 prospective studies and one randomised controlled study about the use of topical Imiquimod for LM [24]. They found complete clinical clearance in 78% (369 of 471 patients) and histological clearance in 77% (285 of 370 patients). They report a recurrence rate of LM in 2% after a mean follow up of 18.6 months (range 9–37 months) and a progression to LMM in 1.8% at a mean of 3.9 months (0–11 months) after completion of treatment.
Imiquimod has also been successfully used as neoadjuvant therapy in LM to decrease the necessary margins for complete clearance [25].
Regarding reported adverse effects, a dose-dependent and possibly severe inflammatory reaction can be clinically observed in the treated area that ceases after stopping the treatment. Rarely flu-like symptoms have been observed [7].
The BNF [26] and patient information leaflet for Imiquimod 5% cream recommends avoiding contact with the eye. Therefore, use on the eyelids is not common. However, there are several publications that describe its use on the eyelids for both Lentigo maligna and non-melanocytic lesions such as actinic keratosis, basal cell carcinoma and squamous cell carcinoma.
Treatment protocols and success rates of Imiquimod for periocular lentigo maligna
There have been two case series and four case reports of imiquimod 5% treatment for periocular lentigo maligna published, with 21 patients in total (Table 1).
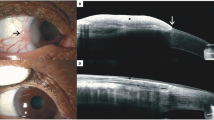
Elia et al. published the largest study, a retrospective case series of 12 patients with periocular LM treated with topical 5% imiquimod cream over a median treatment period of 3 months (range 1–10 months) [27]. In six patients this was primary treatment, and in the other 6 it was adjunctive treatment following local excision (n = 2), cryotherapy (n = 2) or both (n = 2). Erythromycin ointment was applied to the inferior fornix before using imiquimod to protect the ocular surface. Imiquimod was applied once daily except in one patient who only tolerated application every other day.
One patient discontinued treatment due to side-effects, the remaining 11 patients (92%) showed complete clinical and histological clearance.
Demirci et al. reported a case series of five patients treated with topical 5% Imiquimod for periocular LM over a mean duration of 9 months [28]. If the lesion was located within 5 mm of the lid margins, topical erythromycin eye ointment was applied to the eye before Imiquimod to protect the eye. However, their paper did not specify how many patients fell into this group. They clinically observed partial resolution of lesions in two patients and complete resolution in three patients. Yet, they did not report the post-treatment histological examinations.
Four singular case reports about the treatment of LM involving the eyelid with topical Imiquimod 5% have been published [29,30,31,32]. All four cases showed complete clinical resolution of pigmentation with different treatment periods (6 weeks, 2 months, 4 months, and four courses of 6 weeks treatments over 2 years).
Three of those four singular case reports described additional successful treatment of co-existing conjunctival disease.
Bratton et al. combined the treatment of Imiquimod for the eyelid LM with repeated cryotherapy of the periorbital disease, along with guttae interferon-α2β for the associated conjunctival primary acquired melanosis (PAM). The pigmentation of the eyelid skin and conjunctiva completely resolved. No postinterventional histopathology was obtained. 21 months later a mild stippled hyperpigmentation on the conjunctiva reoccurred, that is being observed [29].
Rodríguez-Martín et al. treated a patient with eyelid LM and pigmentation of conjunctiva and caruncle with excisional surgery for the larger skin lesions followed by guttae Mitomycin C for the conjunctival pigmentation and Imiquimod 5% for the caruncle pigmentation. A 6-week course resulted in complete regression of the caruncle lesion with no clinical or histopathological recurrence after 1 year [32].
O’Neill et al. reported clinical clearance of the conjunctival component with Imiquimod to the eyelid skin alone, likely from spillover of the ointment applied to the skin onto the conjunctiva. After 3 years there were no clinical signs of recurrence of both the skin pigmentation and conjunctival pigmentation. However, no histological assessment was performed [31].
In total, 21 patients with periocular lentigo maligna treated with Imiquimod 5% have been published [27,28,29,30,31,32]. However, the treatment protocols in the reported cases vary considerably, making it difficult to interpret the most beneficial regime with the least side effects. In addition, some patients received combined treatments with surgical excision, cryotherapy, topical Interferon-αhβ or topical Mitomycin C. This makes assessment of the efficacy of Imiquimod treatment more difficult.
The dermatology literature shows that complete treatment success of LM with imiquimod is more likely when more than 60 applications are made over 12 weeks [24].
57% (12/21) of patients included in this review received periocular imiquimod in this recommended regime, suggesting that this could be a useful initial prescribing regime, with the caveat of close monitoring by an ophthalmologist.
Overall, the cases showed a 86% (18/21) clinical clearance rate, albeit only 56% (N = 12) had histological post treatment confirmation of clearance, and none had confocal microscopy follow up. This periocular LM success rate with imiquimod treatment is reassuringly similar to the histological clearance rates of 77% [13] with off-label Imiquimod in non-periocular LM lesions. This means that Imiquimod is a very encouraging second-line treatment to that of surgical excision in the periocular area.
Side effects of imiquimod treatment for eyelid lesions
It is important to establish the safety of Imiquimod 5% for lesions of the eyelid, as it is designed to be applied to the skin and not the ocular surface. However, when applied near the lid margin, it is likely that a small amount reaches the ocular surface.
In total, imiquimod has been used periocularly in 81 published cases (21 for lentigo maligna and 60 non-melanocytic lesions) [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. Table 2 details those 16 publications which describe the use of periocular imiquimod and the reported side effects.
The main side effects of imiquimod described were redness (72/81)(not reported if ocular or skin), discomfort (18/81) (not reported if ocular of skin), conjunctival redness/chemosis/conjunctivitis (9/81), swelling (9/81), excoriation/crusting at the application site (9/81). Corneal staining was observed in five cases, epiphora in three cases and a preseptal cellulitis in two cases. There was one reported case each of a staphylococcal keratitis, temporary corneal oedema, ectropion.
73 (90%) patients were able to tolerate treatment and complete their prescribed course. Although 7 (8.6%) needed a treatment holiday (range 3 days to 4 weeks) to reduce side effect severity, and one (1.2%) needed a dose reduction. There was also one non-responder.
These cases have demonstrated safe use in all, and in the majority a tolerable use of 90% (73/82) of topical Imiquimod 5% on the lid margin. Only 9.9% (8/81) of patients had to stop treatment due to intolerable side effects and a further 8.6% required a treatment holiday. Reassuringly all side effects completely resolved once treatment was ceased.
Redness and irritation or even excoriation with crusting of the skin at the application site is to be expected with imiquimod treatment and is believed to indicate a good efficacy of the treatment [27]. Patients without any local reactions are more likely to be poor or non-responders with a lower rate of complete treatment success. It is therefore questionable whether this should be included in the side effects if not requiring a treatment pause, and because of this, it was inconsistently reported across all of the publications.
This review suggests that the small amount of Imiquimod that is likely reaching the ocular surface is well tolerated. If, however, a mistake occurs and a large volume of Imiquimod is applied directly to the ocular surface, it would seem sensible to irrigate the eye with saline or lubricants to reduce the risk of ocular toxicity. It seems sensible to follow Elia et al. [27] and Demirci et al. [28] by prescribing an ocular ointment to be used prior to imiquimod application, such as chloramphenicol or a lubricating ointment, to create a protective barrier for the ocular surface. However, a prospective trial would be needed to clearly demonstrate any benefit in side effect reduction.
The timing of the treatment holiday, cessation or dose reduction was only reported clearly in four patients. This was needed at 1 month in three cases and at 3 months in the other case. This suggests that an ophthalmic examination at 3–4 weeks into treatment is imperative.
Conclusion
With a rising incidence of LM, second-line treatment options need to be investigated especially if patients are unfit for or decline surgical management [4,5,6].
Current literature on retrospective cases shows that 5% imiquimod is a promising treatment modality with a 56–86% complete treatment response and a 90% tolerability rate in the peri-ocular area. In the dermatological literature, Tio et al. found a recurrence of LM after Imiquimod treatment in 2% after a mean follow up of 18.6 months (range 9–37 months) [13].
Importantly, 5% imiquimod offers a superior cosmetic outcome to that of surgical excision, can be used in patients with systemic co-morbidities, is easy to use at home [24], and does not preclude future surgical excision should treatment be unsuccessful or not tolerated.
Further studies are required to assess the optimal treatment protocol to maximise clearance rates of periocular LM with topical 5% imiquimod but with minimal ocular side effects. However, this review shows that 60 applications over 12 weeks (as recommended in non-periocular skin) can be tolerated in many. Treatment holidays or dose reductions should be utilised to enable course completion.
As disease recurrence can occur despite initial clearance of LM [43, 44], follow up is essential. This ideally should ideally include confocal microscopy [45], however this is technically difficult close to the lid margin. When in doubt, repeat biopsies must be performed.
Concerns remain regarding clinical clearance of the pigmentation without histological clearance due to potentially unrecognised progression of the disease. There is speculation that Imiquimod has a limited effect on hair follicles, which is especially important for eyelid LM as the eyelash line is thought to be a source of recurrence [28]. Vice versa, residual pigmentation does not necessarily mean residual LM [46]. Therefore, post-treatment biopsies or at least confocal microscopy, which has been reported to be a useful screening tool with significant correlation to biopsies [45], seem imperative, rather than clinical inspection alone.
Tio et al. recommended a 5 year follow up [13]. Albeit they recommend a follow up for 5 years. Thus, post treatment monitoring is required to cover this period.
References
Shain AH, Bastian BC. From melanocytes to melanomas. Nat Rev Cancer. 2016;16:345–58.
Tannous ZS, Lerner LH, Duncan LM, Mihm MC Jr, Flotte TJ. Progression to invasive melanoma from malignant melanoma in situ, lentigo maligna type. Hum Pathol. 2000;31:705–8.
Fröhlich SM, Cazzaniga S, Kaufmann LS, Hunger RE, Seyed Jafari SM. Retrospective Cohort Study on Patients with Lentigo Maligna Melanoma. Dermatology. 2019;235:340–5.
Greveling K, Wakkee M, Nijsten T, van den Bos R, Hollestein LM. Epidemiology of Lentigo Maligna and Lentigo Maligna Melanoma in the Netherlands. 1989-2013. J Investig Dermatol. 2016;136:1955–60.
Toender A, Kjær SK, Jensen A. Increased incidence of melanoma in situ in Denmark from 1997 to 2011: results from a nationwide population-based study. Melanoma Res. 2014;24:488–95.
Swetter SM, Boldrick JC, Jung SY, Egbert BM, Harvell JD. Increasing incidence of lentigo maligna melanoma subtypes: northern California and national trends 1990-2000. J Investig Dermatol. 2005;125:685–91.
Iznardo H, Garcia-Melendo C, Yélamos O. Lentigo maligna: clinical presentation and appropriate management. Clin Cosmet Investig Dermatol. 2020;13:837–55.
Weinstock MA, Sober AJ. The risk of progression of lentigo maligna to lentigo maligna melanoma. Br J Dermatol. 1987;116:303–10.
Agarwal-Antal N, Bowen GM, Gerwels JW. Histologic evaluation of lentigo maligna with permanent sections: implications regarding current guidelines. J Am Acad Dermatol. 2002;47:743–8.
Kunishige JH, Brodland DG, Zitelli JA. Surgical margins for melanoma in situ. J Am Acad Dermatol. 2012;66:438–44.
Moyer JS, Moyer JS, Rudy S, Boonstra PS, Kraft C, Chinn SB, et al. Efficacy of Staged Excision With Permanent Section Margin Control for Cutaneous Head and Neck Melanoma. JAMA Dermatol. 2017;153:282–8.
Fosko SW, Navarrete-Dechent CP, Nehal KS. Lentigo Maligna-Challenges, Observations, Imiquimod, Confocal Microscopy, and Personalized Treatment. JAMA Dermatol. 2018;154:879–81.
Tio D, van Montfrans C, Ruijter CGH, Hoekzema R, Bekkenk MW. Effectiveness of 5% Topical Imiquimod for Lentigo Maligna Treatment. Acta Derm Venereol. 2019;99:884–8.
Kunishige JH, Doan L, Brodland DG, Zitelli JA. Comparison of surgical margins for lentigo maligna versus melanoma in situ. J Am Acad Dermatol. 2019;81:204–12.
Malhotra R, Chen C, Huilgol SC, Hill DC, Selva D. Mapped serial excision for periocular lentigo maligna and lentigo maligna melanoma. Ophthalmology. 2003;110:2011–8.
Hurwitz DJ, Pincus L, Kupper TS. Imiquimod: a topically applied link between innate and acquired immunity. Arch Dermatol. 2003;139:1347–50.
Garland SM. Imiquimod. Curr Opin Infect Dis. 2003;16:85–9.
Schön MP, Schön M. Imiquimod: mode of action. Br J Dermatol. 2007;157:8–13.
Kasprzak JM, Xu YG. Diagnosis and management of lentigo maligna: a review. Drugs Context. 2015;4:212281.
European Medicines Agency. Human medicine European public assessment report (EPAR): Aldara. 2021; https://www.ema.europa.eu/en/documents/productinformation/aldara-epar-product-information_en.pdf.
Swetter SM, Tsao H, Bichakjian CK, Curiel-Lewandrowski C, Elder DE, Gershenwald JE, et al. Guidelines of care for the management of primary cutaneous melanoma. J Am Acad Dermatol. 2019;80:208–50.
Kirtschig G, van Meurs T, van Doorn R. Twelve-week treatment of lentigo maligna with imiquimod results in a high and sustained clearance rate. Acta Derm Venereol. 2015;95:83–5.
Marsden JR, Fox R, Boota NM, Cook M, Wheatley K, Billingham LJ, et al. Effect of topical imiquimod as primary treatment for lentigo maligna: the LIMIT-1 study. Br J Dermatol. 2017;176:1148–54.
Tio D, van der Woude J, Prinsen CAC, Jansma EP, Hoekzema R, van Montfrans C. A systematic review on the role of imiquimod in lentigo maligna and lentigo maligna melanoma: need for standardization of treatment schedule and outcome measures. J Eur Acad Dermatol Venereol. 2017;31:616–24.
Donigan JM, Hyde MA, Goldgar DE, Hadley ML, Bowling M, Bowen GM. Rate of Recurrence of Lentigo Maligna Treated With Off-Label Neoadjuvant Topical Imiquimod, 5%, Cream Prior to Conservatively Staged Excision. JAMA Dermatol. 2018;154:885–9.
Committee, JF British National Formulary (online) London: BMJ Group and Pharmaceutical Press. 13.02.2022]; https://bnf.nice.org.uk/drug/imiquimod.html.
Elia MD, Lally SE, Hanlon AM, Choi JN, Servat JJ, Shields JA, et al. Periocular Melanoma In Situ Treated With Imiquimod. Ophthalmic Plast Reconstr Surg. 2016;32:371–3.
Demirci H, Shields CL, Bianciotto CG, Shields JA. Topical imiquimod for periocular lentigo maligna. Ophthalmology. 2010;117:2424–9.
Bratton EM, Knutsen-Larson S, Durairaj VD, Gregory DG, Mellette JR. Combination topical therapy for conjunctival primary acquired melanosis with atypia and periocular lentigo maligna. Cornea. 2015;34:90–3.
Murchison AP, Washington CV, Soloman AR, Bernardino CR. Ocular effects of imiquimod with treatment of eyelid melanoma in situ. Dermatol Surg. 2007;33:1136–8.
O’Neill J, Ayers D, Kenealy J. Periocular lentigo maligna treated with imiquimod. J Dermatol Treat. 2011;22:109–12.
Rodríguez-Martín M, Rodríguez-Martín J, Merino de Paz N, Contreras Ferrer P, Rocha Cabrera P, Rodríguez, Martínet B, et al. Conjunctival melanoma: a new clinical and therapeutical approach. Case Rep Dermatol. 2010;2:149–55.
Cannon PS, O’Donnell B, Huilgol SC, Selva D. The ophthalmic side-effects of imiquimod therapy in the management of periocular skin lesions. Br J Ophthalmol. 2011;95:1682–5.
Ross AH, Kennedy CTC, Collins C, Harrad RA. The use of imiquimod in the treatment of periocular tumours. Orbit. 2010;29:83–7.
Brannan PA, Anderson HK, Kersten RC, Kulwin DR. Bowen disease of the eyelid successfully treated with imiquimod. Ophthalmic Plast Reconstr Surg. 2005;21:321–2.
Choontanom R, Thanos S, Busse H, Stupp T. Treatment of basal cell carcinoma of the eyelids with 5% topical imiquimod: a 3-year follow-up study. Graefes Arch Clin Exp Ophthalmol. 2007;245:1217–20.
Blasi MA, Giammaria D, Balestrazzi E. Immunotherapy with imiquimod 5% cream for eyelid nodular basal cell carcinoma. Am J Ophthalmol. 2005;140:1136–9.
Karabulut GO, Kaynak P, Ozturker C, Fazil K, Ocak OB, Taskapili M. Imiquimod 5% cream for the treatment of large nodular basal cell carcinoma at the medial canthal area. Indian J Ophthalmol. 2017;65:48–51.
Prokosch V, Thanos S, Spaniol K, Stupp T. Long-term outcome after treatment with 5% topical imiquimod cream in patients with basal cell carcinoma of the eyelids. Graefes Arch Clin Exp Ophthalmol. 2011;249:121–5.
Leppälä J, Kaarniranta K, Uusitalo H, Kontkanen M. Imiquimod in the treatment of eyelid basal cell carcinoma. Acta Ophthalmol Scand. 2007;85:566–8.
Rowlands MA, Giacometti JN, Servat J, Materin MA, Levin F. Topical Imiquimod in the Treatment of Conjunctival Actinic Keratosis. Ophthalmic Plast Reconstr Surg. 2017;33:e21–e23.
Singh M, Singh H, Kakkar N, Zadeng Z, Gupta P. Treatment of squamous cell carcinoma of the eyelid with imiquimod 5% cream. Can J Ophthalmol. 2019;54:e24–e27.
van Meurs T, van Doorn R, Kirtschig G. Recurrence of lentigo maligna after initial complete response to treatment with 5% imiquimod cream. Dermatol Surg. 2007;33:623–6. discussion 626-7
Woodmansee CS, McCall MW. Recurrence of lentigo maligna and development of invasive melanoma after treatment of lentigo maligna with imiquimod. Dermatol Surg. 2009;35:1286–9.
Brand FL, Seyed Jafari SM, Hunger RE. Confocal microscopy and lentigo maligna: an in vivo pilot study for the assessment of response to imiquimod therapy. Dermatology. 2019;235:150–5.
Powell AM, Russell-Jones R, Barlow RJ. Topical imiquimod immunotherapy in the management of lentigo maligna. Clin Exp Dermatol. 2004;29:15–21.
Author information
Authors and Affiliations
Contributions
IN: Conceived and designed the analysis, Collected the data, Contributed data or analysis tools, Performed the analysis, Wrote the paper, Other contribution; HT: Conceived and designed the analysis, Collected the data, Contributed data or analysis tools, Performed the analysis, Wrote the paper, Other contribution; RP: Conceived and designed the analysis, Collected the data, Contributed data or analysis tools, Performed the analysis, Wrote the paper, Other contribution; MK: Conceived and designed the analysis, Collected the data, Contributed data or analysis tools, Performed the analysis, Wrote the paper, Other contribution; CD: Conceived and designed the analysis, Collected the data, Contributed data or analysis tools, Performed the analysis, Wrote the paper, Other contribution.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Neumann, I., Patalay, R., Kaushik, M. et al. Treatment of periocular lentigo maligna with topical 5% Imiquimod: a review. Eye 37, 408–414 (2023). https://doi.org/10.1038/s41433-022-02165-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02165-5
This article is cited by
-
Rare Cutaneous Side Effects of Imiquimod: A Review on Its Mechanisms, Diagnosis, and Management
Dermatology and Therapy (2023)