Abstract
Objectives
To investigate the long-term outcomes of oral doxycycline as first-line treatment in patients with conjunctival extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma).
Methods
In this case series, the medical records of 67 patients with conjunctival MALT lymphoma who received doxycycline as their primary treatment and were followed up for at least 5 years were retrospectively reviewed. Progression-free survival (PFS) was analysed at 3, 5, and 10 years after the initial doxycycline treatment. A Cox proportional hazards model was used to assess the independent risk factors for progression.
Results
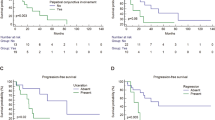
After the initial treatment, 25 patients (37.3%) achieved a complete response, 8 patients (11.9%) achieved a partial response, 30 patients (44.8%) showed stable disease, and 4 patients (6.0%) showed disease progression. The median PFS in all patients was 168 months, and the 3-, 5- and 10-year PFS rates for all patients were 70%, 65%, and 62%, respectively. No further progression was observed 6 years after the initial doxycycline treatment. Younger age and TNM stage T1c were significant risk factors for the time to progression in the multivariate Cox regression analysis (p < 0.05). Additional doxycycline (>2 cycles) showed no benefit. There were no serious adverse events associated with doxycycline therapy, and most patients were successfully salvaged by second-line treatments, including radiotherapy and chemotherapy.
Conclusion
In this case series, oral doxycycline treatment yielded acceptable long-term PFS with minimal complications. Especially in patients with stage T1a or T1b conjunctival MALT lymphoma, first-line doxycycline treatment could be considered under close monitoring for at least 6 years.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All data relevant to the study are included in the article or uploaded as supplementary information.
Change history
18 August 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41433-023-02690-x
References
Yen MT, Bilyk JR, Wladis EJ, Bradley EA, Mawn LA. Treatments for ocular adnexal lymphoma: a report by the american academy of ophthalmology. Ophthalmology. 2018;125:127–36.
Stefanovic A, Lossos IS. Extranodal marginal zone lymphoma of the ocular adnexa. Blood. 2009;114:501–10.
McKelvie PA. Ocular adnexal lymphomas: a review. Adv Anat Pathol. 2010;17:251–61.
Kirkegaard MM, Coupland SE, Prause JU, Heegaard S. Malignant lymphoma of the conjunctiva. Surv Ophthalmol. 2015;60:444–58.
Tanenbaum RE, Galor A, Dubovy SR, Karp CL. Classification, diagnosis, and management of conjunctival lymphoma. Eye Vis (Lond). 2019;6:22.
White WL, Ferry JA, Harris NL, Grove AS Jr. Ocular adnexal lymphoma. A clinicopathologic study with identification of lymphomas of mucosa-associated lymphoid tissue type. Ophthalmology. 1995;102:1994–2006.
Salar A. Gastric MALT lymphoma and Helicobacter pylori. Med Clin (Barc). 2019;152:65–71.
Melenotte C, Mezouar S, Mege JL, Gorvel JP, Kroemer G, Raoult D. Bacterial infection and non-Hodgkin’s lymphoma. Crit Rev Microbiol. 2020;46:270–87.
Ferreri AJ, Ponzoni M, Guidoboni M, Resti AG, Politi LS, Cortelazzo S, et al. Bacteria-eradicating therapy with doxycycline in ocular adnexal MALT lymphoma: a multicenter prospective trial. J Natl Cancer Inst. 2006;98:1375–82.
Kim TM, Kim KH, Lee MJ, Jeon YK, Lee SH, Kim DW, et al. First-line therapy with doxycycline in ocular adnexal mucosa-associated lymphoid tissue lymphoma: a retrospective analysis of clinical predictors. Cancer Sci. 2010;101:1199–203.
Ferreri AJ, Govi S, Pasini E, Mappa S, Bertoni F, Zaja F, et al. Chlamydophila psittaci eradication with doxycycline as first-line targeted therapy for ocular adnexae lymphoma: final results of an international phase II trial. J Clin Oncol. 2012;30:2988–94.
Han JJ, Kim TM, Jeon YK, Kim MK, Khwarg SI, Kim CW, et al. Long-term outcomes of first-line treatment with doxycycline in patients with previously untreated ocular adnexal marginal zone B cell lymphoma. Ann Hematol. 2015;94:575–81.
Collina F, De Chiara A, De Renzo A, De Rosa G, Botti G, Franco R. Chlamydia psittaci in ocular adnexa MALT lymphoma: a possible role in lymphomagenesis and a different geographical distribution. Infect Agent Cancer. 2012;7:8.
Ferreri AJ, Guidoboni M, Ponzoni M, De Conciliis C, Dell’Oro S, Fleischhauer K, et al. Evidence for an association between Chlamydia psittaci and ocular adnexal lymphomas. J Natl Cancer Inst. 2004;96:586–94.
Ponzoni M, Ferreri AJ, Guidoboni M, Lettini AA, Cangi MG, Pasini E, et al. Chlamydia infection and lymphomas: association beyond ocular adnexal lymphomas highlighted by multiple detection methods. Clin Cancer Res. 2008;14:5794–5800.
Yoo C, Ryu MH, Huh J, Park JH, Kang HJ, Ahn HS, et al. Chlamydia psittaci infection and clinicopathologic analysis of ocular adnexal lymphomas in Korea. Am J Hematol. 2007;82:821–3.
Daibata M, Nemoto Y, Togitani K, Fukushima A, Ueno H, Ouchi K, et al. Absence of Chlamydia psittaci in ocular adnexal lymphoma from Japanese patients. Br J Haematol. 2006;132:651–2.
Aigelsreiter A, Leitner E, Deutsch AJ, Kessler HH, Stelzl E, Beham-Schmid C, et al. Chlamydia psittaci in MALT lymphomas of ocular adnexals: the Austrian experience. Leuk Res. 2008;32:1292–4.
Zhang D, Dong L, Li H, Jin H, Ye H, Zhou X, et al. Ocular adnexal mucosa-associated lymphoid tissue lymphoma in Northern China: high frequency of numerical chromosomal changes and no evidence of an association with Chlamydia psittaci. Leuk Lymphoma. 2010;51:2031–8.
Jaffe ES, Harris NL, Stein H, Isaacson PG. Classification of lymphoid neoplasms: the microscope as a tool for disease discovery. Blood. 2008;112:4384–99.
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–90.
Coupland SE, White VA, Rootman J, Damato B, Finger PT. A TNM-based clinical staging system of ocular adnexal lymphomas. Arch Pathol Lab Med. 2009;133:1262–7.
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, et al. Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol. 1999;17:1244.
Kwon M, Lee JS, Lee C, Yoon DH, Sa HS. Prognostic factors for relapse and survival among patients with ocular adnexal lymphoma: validation of the eighth edition of the American Joint Committee on Cancer (AJCC) TNM classification. Br J Ophthalmol. 2021;105:279–84.
Cho EY, Han JJ, Ree HJ, Ko YH, Kang YK, Ahn HS, et al. Clinicopathologic analysis of ocular adnexal lymphomas: extranodal marginal zone b-cell lymphoma constitutes the vast majority of ocular lymphomas among Koreans and affects younger patients. Am J Hematol. 2003;73:87–96.
Woo JM, Tang CK, Rho MS, Lee JH, Kwon HC, Ahn HB. The clinical characteristics and treatment results of ocular adnexal lymphoma. Korean J Ophthalmol. 2006;20:7–12.
Yoon JS, Ma KT, Kim SJ, Kook K, Lee SY. Prognosis for patients in a Korean population with ocular adnexal lymphoproliferative lesions. Ophthalmic Plast Reconstr Surg. 2007;23:94–99.
Nam SW, Woo KI, Kim YD. Characteristics of primary extranodal marginal zone B-cell lymphoma in Korea: conjunctiva versus other ocular adnexa. Br J Ophthalmol. 2018;102:502–8.
Author information
Authors and Affiliations
Contributions
Concept and design: TMK and HJC. Acquisition, analysis, or interpretation of data: SHC, MKY, MK and HJC. Manuscript draft: SHC and HJC. Critical revision of the manuscript for important intellectual content: SHC, MKY, MK and HJC. Statistical analysis: SHC; Administrative, technical, or material support: MKY and TMK; Supervision: TMK and HJC; Guarantor: HJC.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The sentence “Older age and TNM stage T1c were significant risk factors for the time to progression in the multivariate Cox regression analysis (p<0.05)” in the abstract was corrected to read as follows: “Younger age and TNM stage T1c were significant risk factors for the time to progression in the multivariate Cox regression analysis (p<0.05)”.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Choi, S.H., Yang, M.K., Kim, T.M. et al. Feasibility of oral doxycycline as first-line therapy for conjunctival mucosa-associated lymphoid tissue lymphoma. Eye 38, 82–88 (2024). https://doi.org/10.1038/s41433-023-02635-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02635-4