Abstract
Purpose
To examine the risk for retinal-vein-occlusion (RVO) in patients with neovascular age-related-macular-degeneration (AMD) as compared to age- and sex-matched controls.
Method
This is a population-based, cohort study. The study encompassed 24,578 consecutive patients with neovascular AMD and 66,129 control subjects. Multivariate cox regression analysis was utilized to detect the risk of RVO among patients with neovascular AMD. Predictors of RVO in patients with neovascular AMD were identified using multivariate logistic regression analysis. Mortality of patients was assessed using Kaplan–Meier method.
Results
The incidence rate of RVO was estimated at 1.25 (95% CI, 1.06–1.45) per 1000 person-years among patients with neovascular AMD and 0.25 (95% CI, 0.20–0.31) per 1000 person-years among controls. Patients with neovascular AMD were associated with an increased risk of RVO (adjusted HR, 4.35; 95% CI, 3.34–5.66; P < 0.001). Among patients with neovascular AMD, older age (≥79.0 years) was associated with a decreased risk of RVO (adjusted OR, 0.50; 95% CI, 0.37–0.70; P < 0.001), whilst a history of glaucoma increased the likelihood of RVO (adjusted OR, 2.66; 95% CI, 1.94–3.65; P < 0.001). Patients with neovascular AMD and comorbid RVO had a comparable risk of all-cause mortality relative to other patients with neovascular AMD (HR, 0.90; 95% CI, 0.67–1.22; P = 0.500)
Conclusions
An increased risk of RVO was found among patients with neovascular AMD. Younger age and glaucoma predicted the development of RVO in patients with neovascular AMD. Awareness of this comorbidity is of benefit for clinicians as patients with neovascular AMD might be carefully examined for RVO signs and complications.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is the primary cause of blindness in people over the age of 65 in industrialized countries [1]. AMD is classified into non-neovascular and neovascular types. Neovascular AMD, also called “wet AMD”, is the late and serious type of AMD [2]. It is characterized by choroidal neovascularization, which starts from choriocapillaris, extending to the Bruch′s membrane in the area of the macula and causing central vision impairment [3].
Retinal vein occlusions (RVO) is the second most common cause of severe visual impairment and blindness in the elderly [4]. It can be divided into two primary categories depending on the site of obstruction: central RVO (CRVO) when the occlusion involves the whole central retinal vein, and branch RVO (BRVO) when the occlusion involves only one branch of the central retinal vein [5]. BRVO occurs at arterio-venous crossing sites that share a common adventitia [6]. CRVO is caused by external compression of the central retinal artery, which shares a common fibrous sleeve with the vein [7]. RVO may cause macular oedema, retinal neovascularization and neovascular glaucoma [7].
It is known that increased expression of vascular endothelium growth factor (VEGF) plays a major role in angiogenesis in neovascular AMD [3] as well as in macular oedema in RVO [8]. However, it is unknown if people with neovascular AMD are at increased risk of developing also RVOs. Therefore, the purpose of this current study is to examine the risk for RVO in neovascular AMD patients compared to age- and sex-matched controls subjects. Additionally, we sought to identify predictors of RVO among patients with neovascular AMD.
Methods
Study design and database
The current study was designed as a population-based historical cohort study. The study was endorsed by the institutional review board (IRB) of Ben-Gurion University in accordance with the declaration of Helsinki (approval code: 0212-17-COM).
Clalit Health Services (CHS) computerized database was the source of the current study. CHS is the largest health maintenance provider in Israel, providing a broad assortment of healthcare services for a population of roughly 4.5 million inhabitants as of October 2018. The electronic dataset of CHS continuously retrieves data from clinical, pharmaceutical, and administrative operating systems and was evidenced as a prolific and reliable source of well-designed epidemiological studies. The characteristics of the utilized database are further detailed in other publications [9, 10].
Study population, definition of patients, and covariates
Medical files of all enrolees of CHS were systematically screened for a diagnosis of neovascular AMD. The latter was based on the following eligibility criteria: (i) a diagnosis of neovascular AMD as registered by a board-certified ophthalmologist (that is based his diagnosis on Optical Coherence Tomography (OCT) exam and clinical diagnosis), or (ii) a diagnosis of neovascular AMD documented in a discharge letter from an ophthalmological inpatient ward (diagnosis is based on clinical exam and OCT), or (iii) prescription of ranibizumab (Lucentis®) or aflibercept (Eylea®) or bevacizumab (Avastin®) among patients with any diagnosis of AMD.
We additionally recruited a control group encompassing up to three individuals per each eligible case. Controls were randomly selected from CHS enrolees lacking a diagnosis of AMD and were individually-matched in accordance with age, sex, and ethnicity. A control subject was recruited at the same date in which the diagnosis of the respective case was documented.
Patients with neovascular AMD and control subjects were followed longitudinally and compared with regard to the incidence of RVO (in the same eye of AMD in the study group). Patients with AMD were examined every 3 months while control patients were examined every 6–12 months. The diagnosis of RVO relied on the chronic registry of CHS. That is, a diagnosis of BRVO or CRVO was documented by a board-certified ophthalmologist or in discharge letters from ophthalmological inpatient wards and was based on clinical examination and OCT.
Outcome measures were adjusted for age, sex, ethnicity, and socioeconomic status (model 1) to refute the presence of meaningful residual confounding. Given that RVO was reported to associate with glaucoma, hypertension, diabetes mellitus, hyperlipidaemia, ischemic heart disease, and stroke [11], we additionally adjusted for these comorbidities (model 2). The diagnosis of these comorbidities was retrieved from the chronic registry of CHS.
Statistical analysis
Baseline characteristics are demonstrated as means and standard deviations (SD)s for continuous variables and percentages for categorical variables. The circulation of clinical and sociodemographic factors was thought about between AMD patients and controls utilizing Chi-square test and t-test, as shown.
The incidence rate of RVO both among cases and controls was determined as the number of cases per 1000 person-years. Hazard ratios (HR)s for the risk of RVO were determined by the utilization of Cox regression models. Cases and controls with a preexisting diagnosis of RVO prior to the study initiation were excluded from the current analysis.
The cumulative survival of neovascular AMD patients with and without RVO was calculated using Kaplan-Meier method and compared between the subgroups via stratified log-rank test. Age stratification was performed on the basis of the median age of study participants (79.0 years).
Two-tailed P-values less than 0.05 were considered statistically significant, whereas results with 95% confidence intervals (CI)s were reported where applicable.
All statistical analyses were performed using SPSS software, version 25 (SPSS, Armonk, NY: IBM Corp).
Results
The study population included 24,578 consecutive patients with neovascular AMD and 66,129 control subjects. The mean (SD) age at the onset of neovascular AMD was 78.3 (9.2), and 43.7% and 94.3% of the study population were males and of Jewish ancestry, respectively. The mean BMI and the prevalence of smoking were both significantly higher among patients with neovascular AMD. Table 1 delineates the baseline characteristics of the study population.
Patients with neovascular AMD and controls were followed for 128,440.4 and 343,556.3 person-years, respectively. During the follow-up duration, 160 and 87 events of new-onset RVO occurred in the aforementioned groups, respectively. Taken together, the incidence rate of RVO was estimated at 1.25 (95% CI, 1.06–1.45) per 1000 person-years among patients with neovascular AMD and 0.25 (95% CI, 0.20–0.31) per 1000 person-years among controls (Table 2).
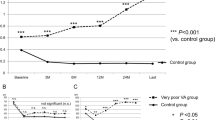
The unadjusted risk of RVO was almost fivefold higher among patients with neovascular AMD relative to control subjects (HR, 4.90; 95% CI, 3.77–6.36; P < 0.001; Fig. 1A). In sex-and age-stratified analyses, the risk of RVO was higher among males (HR, 5.21; 95% CI, 3.56–7.63; P < 0.001) and younger individuals (<79.0 years; HR, 6.38; 95% CI, 4.45–9.15; P < 0.001; Table 2).
We then performed multivariate analyses to identify the independent risk of RVO that is imposed by neovascular AMD. The substantially increased risk retained its statistical significance after controlling for demographic variables (model 1: adjusted HR, 5.00; 95% CI, 3.85–6.49; P < 0.001) and for demographic variables and comorbidities (model 2: adjusted HR, 4.35; 95% CI, 3.34–5.66; P < 0.001; Table 2).
The last endpoint of the current study was to identify predictors of RVO in patients with neovascular AMD (Table 3). Older age was proved protective against the risk of developing RVO (adjusted OR, 0.50; 95% CI, 0.37–0.70; P < 0.001), whereas a history of glaucoma was associated with an increased likelihood of RVO (adjusted OR, 2.66; 95% CI, 1.94–3.65; P < 0.001). Sex, ethnicity, and other comorbidities were not found to be significantly associated with the development of RVO (Table 3). Relative to other patients with neovascular AMD, those with AMD and comorbid RVO demonstrated a comparable risk of all-cause mortality (HR, 0.90; 95% CI, 0.67–1.22; P = 0.500; Fig. 1).
Discussion
The current large-scale population-based study disclosed that patients with neovascular AMD experience a fivefold increased risk of developing RVO as compared to control individuals. This risk was more prominent among males and younger patients and was robust to multivariate analysis. While the presence of a preexisting history of glaucoma predisposes patients with neovascular AMD to RVO, old age emerged as a protective factor against the development of RVO. The all-cause mortality rate was comparable between neovascular AMD patients with and without RVO.
Hypoxia plays a central role in RVOs as well as in neovascular AMD [12,13,14]. It increases the production of VEGF that causes excessive vascular permeability, neovascularization, and closure of retinal vessels. This cause an exacerbating of the hypoxia and creating a positive feedback loop in RVO as well as in neovascular AMD [12,13,14].
As the pathogenesis of those diseases shares the same factors, it is conceivable to assume that an association exists between them. In this current cohort study, we found that patients with neovascular AMD were almost at a fivefold increased risk of developing RVO compared to control subjects (HR, 4.90). This risk persisted after adjustment to comorbidities and demographic characteristics. To the best of our knowledge, this is the first study that demonstrates this association.
One of the known risk factors of RVOs is the male gender [11]. In this current study, both genders with neovascular AMD were at increased risk to develop RVOs. However, neovascular AMD male patients had higher risk of RVO, thus aligning with the current literature.
Old age is another well-established risk factor of RVO [15]. Surprisingly, we found that younger patients with neovascular AMD had a higher risk of RVO and that older age protected against the development of RVO. This finding might reflect the lower baseline incidence rate of RVO among young individuals in the reference group, thus rendering the HR higher.
It is known that the majority of people diagnosed with RVO had at least 1 component of the metabolic syndrome (defined as the presence of hypertension [15], diabetes mellitus, hyper-triglyceridemic and low HDL [16]) or vascular diseases (like ischemic heart disease and cerebrovascular accident [17]) or glaucoma [18]. Since these variables are strongly associated with RVO, they were included in a multivariate analysis to enable estimating the independent risk conferred by neovascular AMD. After adjustment, it was found that patients with neovascular AMD are at more than 4 times increased risk to develop RVOs. This finding indicates that neovascular AMD embodies an independent risk factor of RVO.
In addition, we aimed to evaluate whether these comorbidities predispose patients with neovascular AMD to develop RVO. Glaucoma emerged as an independent predictor of subsequent development of RVO in patients with neovascular AMD. Younger patients were additionally found as an independent predictor of RVO. Therefore, younger neovascular AMD with comorbid glaucoma should be examined carefully to exclude signs of RVO and its complications.
In retina clinics in the western world, in the past two decades, the use of the OCT in neovascular AMD has become very common and even considered as an essential exam in the management of patients with neovascular AMD [19]. As the prevalence of neovascular AMD is increasing due to growing longevity [1], the use of OCT without a clinical exam by slit-lamp became even more common [20, 21]. In the OCT exam, some findings like some BRVO and RVO complications like retinal neovascularization, retinal haemorrhage, neovascular glaucoma, and high intraocular pressure can be missed. The finding of this current study suggesting an increased risk for RVO in patients with neovascular AMD demonstrates that the clinical exam is essential in neovascular AMD patients. Moreover, while the treatment for neovascular AMD is composed only of anti-VEGF agents, the treatment for macular oedema secondary to RVO can also include corticosteroid injections [22]. Therefore, it is important to diagnose the exact reason for the decrease in visual acuity in patients with RVO and AMD.
To the best of our knowledge, the current study is the first population-based cohort study to shed light on the association between neovascular AMD and RVO. We contributed a novel epidemiological feature regarding the risk of developing RVO during the course of AMD. Furthermore, the current study population represent one of the world’s largest cohorts of patients with neovascular AMD.
This study is not without limitations. One of the limitations is that there was no differentiation between the patients who develop CRVO and those who develop BRVO. Another limitation is the ethnicity of the population in this study which included only Jewish and Arab subjects, reflecting the ethnic composition of the Israeli population. Asians and Hispanics, who are known for their increased risk of RVO [4] were not included in this study. Further prospective studies are needed to evaluate this epidemiological relationship in other ethnic groups as well as the differences between CRVO and BRVO.
In conclusion, we demonstrate a fivefold increased risk of RVO among patients with neovascular AMD. The risk was more prominent among young and male individuals. The presence of comorbid glaucoma and younger age were independent predictors of RVO among patients with neovascular AMD. Patients with neovascular AMD, particularly those with comorbid glaucoma should undergo careful slit lamp clinical examination for RVO signs and complications in each follow up visit and not just OCT exam. Further research is required to reproduce our findings in other study populations originating from different ethnic backgrounds.
Summary Table
What was known before
-
Age-related macular degeneration (AMD) is the primary cause of blindness in people over the age of 65 in industrialized countries.
-
Retinal vein occlusion (RVO) is the second most common cause of severe visual impairment and blindness in the elderly.
-
It is known that increased expression of vascular endothelium growth factor (VEGF) plays a major role in angiogenesis in neovascular AMD as well as in macular oedema in RVO.
What this study adds
-
Patients with neovascular AMD experience a fivefold increased risk of developing RVO as compared to control individuals.
-
This risk was more prominent among males and younger patients.
-
The presence of a preexisting history of glaucoma predisposes patients with neovascular AMD to RVO, old age emerged as a protective factor against the development of RVO.
Data availability
It is not possible to share research data publicly, due to individual privacy. In case that necessary, as approval from the IRB as well as the patients will be needed.
References
Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Heal. 2014;2:e106–16. https://doi.org/10.1016/S2214-109X(13)70145-1
Mitchell P, Liew G, Gopinath B, Wong TY. Age-related macular degeneration. Lancet 2018;392:1147–59. https://doi.org/10.1016/S0140-6736(18)31550-2
Bhutto I, Lutty G. Understanding age-related macular degeneration (AMD): Relationships between the photoreceptor/retinal pigment epithelium/Bruch’s membrane/choriocapillaris complex. Mol Asp Med. 2012;33:295–317. https://doi.org/10.1016/j.mam.2012.04.005
Rogers S, McIntosh RL, Cheung N, Lim L, Wang JJ, Mitchell P, et al. The Prevalence of Retinal Vein Occlusion: Pooled Data from Population Studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010;117:313–9.e1. https://doi.org/10.1016/j.ophtha.2009.07.017
Coscas G, Loewenstein A, Augustin A, Bandello F, Battaglia Parodi M, Lanzetta P, et al. Management of retinal vein occlusion - Consensus document. Ophthalmologica. 2011;226:4–28. https://doi.org/10.1159/000327391
Frangieh GT, Green WR, Barraquer Somers E, Finkelstein D. Histopathologic Study of Nine Branch Retinal Vein Occlusions. Arch Ophthalmol. 1982;100:1132–40. https://doi.org/10.1001/archopht.1982.01030040110020
Haymore JG, Mejico LJ. Retinal vascular occlusion syndromes. Int Ophthalmol Clin. 2009;49:63–79. https://doi.org/10.1097/IIO.0b013e3181a8db88
Kaur C, Foulds WS, Ling EA. Blood-retinal barrier in hypoxic ischaemic conditions: Basic concepts, clinical features and management. Prog Retin Eye Res. 2008;27:622–47. https://doi.org/10.1016/j.preteyeres.2008.09.003
Kridin K, Zelber-Sagi S, Comaneshter D, Cohen AD. Association between schizophrenia and an autoimmune bullous skin disease-pemphigus: a population-based large-scale study. Epidemiol Psychiatr Sci. 2019;28:191–8. https://doi.org/10.1017/S204579601700052X
Kridin K, Amber K, Khamaisi M, Comaneshter D, Batat E, Cohen AD. Is there an association between dipeptidyl peptidase-4 inhibitors and autoimmune disease? A population-based study. Immunol Res. 2018;66:425–30. https://doi.org/10.1007/s12026-018-9005-8
Kolar P. Risk factors for central and branch retinal vein occlusion: a meta-analysis of published clinical data. J Ophthalmol. 2014;2014:724780. https://doi.org/10.1155/2014/724780
Karia N. Retinal vein occlusion: Pathophysiology and treatment options. Clin Ophthalmol. 2010;4:809–16. https://doi.org/10.2147/opth.s7631
Young RW. Pathophysiology of age-related macular degeneration. Surv Ophthalmol. 1987;31:291–306. https://doi.org/10.1016/0039-6257(87)90115-9
Campochiaro PA, Akhlaq A Sustained suppression of VEGF for treatment of retinal/choroidal vascular diseases. Prog Retin Eye Res. https://doi.org/10.1016/j.preteyeres.2020.100921
Cugati S, Jie JW, Rochtchina E, Mitchell P. Ten-year incidence of retinal vein occlusion in an older population: The blue mountains eye study. Arch Ophthalmol. 2006;124:726–32. https://doi.org/10.1001/archopht.124.5.726
Recchia FM, Brown GC. Systemic disorders associated with retinal vascular occlusion. Curr Opin Ophthalmol. 2000;11:462–7. https://doi.org/10.1097/00055735-200012000-00013
Yau JWY, Lee P, Wong TY, Best J, Jenkins A. Retinal vein occlusion: An approach to diagnosis, systemic risk factors and management. Intern Med J. 2008;38:904–10. https://doi.org/10.1111/j.1445-5994.2008.01720.x
Lang GE, Spraul CW. Risk factors for retinal vein occlusion. Tagl Prax. 2002;43:787–94. https://doi.org/10.1016/s0161-6420(92)31940-2
Haar CM Summary of Recommendations. In: Mastering Boston Harbor. National Institute for Health and Care Excellence (UK); 2015:311-4. https://doi.org/10.4159/9780674038097-023
Gale RP, Mahmood S, Devonport H, Patel PJ, Ross AH, Walters G, et al. Action on neovascular age-related macular degeneration (nAMD): recommendations for management and service provision in the UK hospital eye service. Eye 2019;33:1. https://doi.org/10.1038/s41433-018-0300-3
Alexander CW. Time is now for retina exams to move from slit lamp to OCT biomicroscopy. Ocular surgery news. 2012.
Bremond-Gignac D. Investigational drugs for retinal vein occlusion. Expert Opin Investig Drugs. 2016;25:841–50. https://doi.org/10.1080/13543784.2016.1181750
Acknowledgements
ADC served as an advisor, investigator, or speaker for Abbvie, BI, Dexcel Pharma, Janssen, Novartis, Perrigo, Pfizer, and Rafa. None of the other authors have any conflicts of interest to declare. No funding was provided for this manuscript. The manuscript has not been published elsewhere, has not been evaluated for publication previously by another journal, and was not submitted simultaneously for publication elsewhere.
Author information
Authors and Affiliations
Contributions
OW: Conception or design of the work, Data collection, Critical revision of the article, Final approval of the version to be published. MK: Data analysis and interpretation, Drafting the article, Final approval of the version to be published. KK: Conception or design of the work, Data collection, Data analysis and interpretation, Critical revision of the article, Final approval of the version to be published. OM: Critical revision of the article, Final approval of the version to be published. ADC: Conception or design of the work, Data collection, Critical revision of the article, Final approval of the version to be published. OZ: Conception or design of the work, Data analysis and interpretation, Drafting the article, Final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weinstein, O., Kridin, M., Kridin, K. et al. The risk of retinal vein occlusion among patients with neovascular age related macular degeneration: a large-scale cohort study. Eye 37, 1445–1450 (2023). https://doi.org/10.1038/s41433-022-02163-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02163-7