Abstract
Objectives
To compare visual and anatomical outcomes between internal limiting membrane (ILM) flap (IF) and peeling (IP) techniques for full-thickness macular holes (FTMHs).
Methods
A retrospective case series with propensity-score matching (PSM). Patients with a minimum 12 months follow-up were divided into IF and IP groups and matched based on FTMH size and preoperative best-corrected visual acuity (BCVA). BCVA and optical coherence tomography (OCT) findings were obtained to assess outer retinal layer integrity, foveal thickness, and foveal displacement.
Results
Twenty-six eyes were included in each group after PSM. The IF group showed significantly greater BCVA after 1 month, its corresponding change from preoperative BCVA, proportions of eyes with ellipsoid zone defects <250 μm after 1 month, and interdigitation zone restoration after 6 and 12 months (P = 0.007, 0.038, 0.048, 0.025, and 0.023, respectively), as well as less foveal gliosis after 1, 3, 6, and 12 months (P = 0.020, 0.017, 0.050, and 0.024, respectively). In the IP group, the mean outer nuclear layer thickness significantly decreased at 3 (P = 0.019) and 12 months (P = 0.016) compared to 1 month, and the foveal displacement toward the optic disc was significant after 1, 3, 6, and 12 months (P = 0.049, 0.006, 0.001, and <0.001, respectively).
Conclusions
Compared to IP, IF promoted faster recovery of BCVA and outer retinal layers and was more protective against postoperative foveal thinning and displacement; hence, it should be considered for small and large FTMHs.
Similar content being viewed by others
Introduction
The innermost foveal layer is composed of specialised Müller cells which form the Müller cell cone [1,2,3,4]. A macular hole (MH) develops by disruption of both the Müller cell cone and the foveolar external limiting membrane (ELM) [3, 5]. MH surgery involves pars-planar vitrectomy (PPV), combined with internal limiting membrane (ILM) removal and gas tamponade with success depending on elimination of vitreo-macular tractional forces, retinal extensibility, and mechanical forces provided by foveal Müller cells [6, 7]. While ILM peeling (IP) remains the method of choice for repairing full-thickness MHs (FTMHs), its success rate is lower for large MHs, with associated retinal damage (dissociated optic nerve fibre layer [DONFL]) [8,9,10,11,12].
In 2010, inverted ILM flap (IF) technique was first introduced, which showed a higher MH closure rate for MH >400 μm than the IP technique [12]. While the IF technique has shown comparable or superior outcomes to those of the IP technique [13,14,15,16], only few studies have reported the IF technique for MH <400 μm [13, 17]. Some studies lacked a control group, or did not account for baseline confounders, including MH size and preoperative visual acuity. Thus, we conducted propensity-score matching based on potential confounders between the IF and IP groups to analyse long-term visual and anatomical outcomes.
Material and methods
Study population
We retrospectively reviewed the medical records and imaging studies of 251 patients who underwent primary vitrectomy with gas tamponade for idiopathic FTMH at the Department of Ophthalmology, Yonsei University College of Medicine, between January 2017 and April 2020. This study was approved by the institutional review board at Yonsei University Medical Center (No. 4-2021-1519), and the requirement for informed consent was waived. This study adhered to the principles of the Declaration of Helsinki.
Patients who followed up for ≥12 months were included. After exclusion of those with partial-thickness or secondary MHs, myopia >6.00 D, axial length >26.5 mm, history of vitrectomy, or any other identified vision-limiting pathology other than cataracts, 80 patients were selected. Demographic data included sex, age, refractive error, axial length, lens status, and pre-and post-operative best-corrected visual acuity (BCVA) using Snellen chart visual acuity converted to logarithm of minimal angle of resolution (logMAR). The spherical equivalent refractive error was obtained using autorefraction (KR-1, Topcon, Tokyo Japan). Axial length was measured using IOLMaster 700 (Carl Zeiss Meditec AG, Jena, Germany). Optical coherence tomography (OCT) examinations were performed with Spectralis OCT (Heidelberg Engineering, Heidelberg, Germany).
Preoperatively, the minimum linear distance (MLD) and basal diameter (BD) of MH, defined as the smallest linear distance of an MH and linear distance of exposed retinal pigment epithelium (RPE), respectively, were measured using Heidelberg Eye Explorer software. The presence of preoperative complete posterior vitreous detachment (PVD) was assessed using OCT. Postoperatively, we assessed MH closure, ELM restoration (defined as presence of a continuous retinal layer), ellipsoid zone (EZ) restoration, and interdigitation zone (IZ) restoration, outer foveal microdefect (OFMD; EZ defects <250 μm) [18], foveal detachment (hypo-reflective spaces), and foveal gliosis (disorganised hyperreflective tissue within 0.5 mm of the fovea) [17, 19] (Supplementary Fig. 1). The distances between the centralmost ELM and the RPE and the centralmost inner retinal surface and the ELM, which represents the foveolar outer nuclear layer (ONL) thickness, were measured.
The distance across the fundus was also measured. The centre of the MH or postoperative foveola was determined by manually aligning the vertical and horizontal OCT scans in the infrared image window. When the postoperative foveal pit was irregular, the thinnest part of the OCT scan was considered as the foveal centre [20]. The preoperative and postoperative distance from the foveal centre to the vessel at the temporal margin of the optic disc (MH-D and F-D, respectively), and distance between the foveal centre and a vascular bifurcation or crossover region located superonasal (MH-S and F-S, respectively) and inferonasal (MH-I and F-I,W respectively) to the fovea were measured (Supplementary Fig. 2) [21]. To compensate for variations, each distance was divided by the vertical diameter of the optic disc and divided by the mean preoperative distance for normalisation.
Surgical strategy
All patients underwent primary standard 3-port pars planar vitrectomy (CONSTELLATION, Alcon Surgical, Ft. Worth, TX). PVD was induced if not already present. The surgeon stained ILM with indocyanine green dye and used ILM forceps to either fully remove the ILM or make an ILM flap from the superior side of the MH, which was then inverted and gently manipulated to cover the MH (Supplementary Fig. 3). For the IF technique, the surgeon used dispersive viscoelastic to stabilise the flap before performing fluid-air exchange. After fluid-air exchange, the vitreous cavity was filled with gas. Patients were instructed to spend 1–2 weeks in the prone position. Phacoemulsification and intraocular lens implantation were performed either at the beginning of the surgery or within 12 months after the surgery. All IF surgeries were performed by SHB and all IP surgeries were performed by other experienced surgeons.
Outcomes
The primary outcome was the success of MH closure within 12 months postoperatively. Secondary outcomes were BCVA, retinal layer integrity, distance of centralmost ELM to RPE, foveolar ONL thickness, F-D, F-S, and F-I.
Study participants
We performed 1:1 propensity-score matching with the IF and IP group datasets to balance the baseline covariates and decrease potential confounders between the two groups using the nearest-neighbour algorithm with a caliper set to 0.2 [22, 23]. Propensity score method used a multivariable logistic regression model based on the following objective preoperative characteristics: age, sex, spherical equivalent, axial length, MLD, BD, preoperative BCVA, and the presence of PVD. The adequacy of matching was validated by comparing propensity-score densities and standardised mean differences (SMDs), which is calculated as the population mean difference between both groups, scaled by population standard deviation (SD). SMDs represent meaningful method to assess between groups than the traditional P value. An SMD of 10% or less was deemed to be the ideal balance, and 20% or less was deemed to be an acceptable balance [24, 25].
Statistical analysis
Statistical analysis was performed using SPSS (version 22; SPSS Inc., Chicago, IL, USA). Continuous variables were presented as means ± SD, and categorical variables were presented as numbers (n) and relative frequencies (%). Significance was determined by Student’s t-test, Mann–Whitney U test, chi-square test, and Fisher’s exact test, as appropriate. Statistical significance was set at P < 0.05.
Results
The clinical characteristics of 80 eyes of 76 patients (mean age ± SD, 64.1 ± 7.4 years; male [%], 29 [36.3%]) who underwent vitrectomy for FTMH were analysed. Of the 80 cases, 37 (46.25%) and 43 (53.75%) were IF and IP cases, respectively (Table 1 and Supplementary Fig. 4). The IF cases showed significantly greater MLD and BD (Table 1). Preoperative BCVA was significantly higher for IP cases (Table 1). The differences in mean age, proportion of men vs. women, mean refractive error, mean axial length, and proportion of patients with complete PVD were not significant (all P > 0.05) (Table 1).
The matched sample size was 26 cases in each group, with no major imbalances in all baseline clinical characteristics (Table 1 and Supplementary Fig. 5). Mean preoperative BCVA, MLD, BD, and cases with MLD < 400 μm were comparable for IP and IF groups (Table 1).
In each group, 24 cases (92.3%) showed successful FTMH closure (P > 0.999). Both IF and IP groups showed significant improvement in the postoperative BCVA after 1, 3, 6, and 12 months compared to the preoperative BCVA (Fig. 1). Postoperative BCVA at 1 month was significantly greater in the IF group than in the IP group (Fig. 1). The change in BCVA from preoperative BCVA was also significantly greater in the IF group than in the IP group at 1 month (P = 0.038) but was comparable at 3 (P = 0.294), 6 (P = 0.234), and 12 (P = 0.423) months.
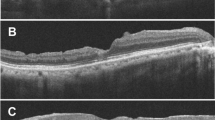
Both groups showed high ELM restoration rates (92.3% vs. 84.6%, P = 0.668) at 12 months postoperatively (Fig. 2A). The rate of EZ defect <250 μm was significantly higher in the IF group after 1 month, but not after 3, 6, and 12 months (Fig. 2B). The rate of OFMD was not significantly different between the two. Restoration of IZ was significantly higher in the IF group only after 6 and 12 months (Fig. 2C). The incidence of foveal detachment was not statistically significant (Fig. 2D). The rate of foveal gliosis was significantly lower in the IF group after 1, 3, 6, and 12 months (Fig. 2E).
A Proportion of ELM restoration. B Proportion of EZ < 250 μm. EZ < 250 μm cases include OFMD and EZR cases. C Proportion of IZ restoration. D Proportion of foveal detachment. E Proportion of foveal gliosis. *P < 0.05. ELM external limiting membrane, EZ ellipsoid zone, EZR complete ellipsoid zone restoration, IZ interdigitation zone, M month, OFMD outer foveal microdefect.
Time-dependent alteration in the distance between the centralmost ELM and RPE and foveolar ONL thickness were analysed. For the IF group, ELM-RPE distance showed a gradual increasing pattern from postoperative month 3 (Fig. 3A). For IP group, ELM-RPE distance gradually decreased (Fig. 3A). The differences in mean ELM-RPE distance were not significant for either group (all P > 0.05). The mean changes in the distance between the ELM and RPE at 1 and 12 months postoperatively were also not significant between the two groups (P = 0.732). The mean foveolar ONL thickness between 1 and 12 months postoperatively gradually increased in the IF group (Fig. 3B). The difference in mean foveolar ONL thickness in the IF group between postoperative months 1, 3, 6, and 12 months was not significant (all P > 0.05). For the IP group, significant decrease in the distance occurred between 1 and 3 months and 1 and 12 months postoperatively (Fig. 3B). The difference in mean foveolar ONL thickness from postoperative months 1 and 12 was statistically different between the two groups (20.2 ± 56.55 µm for the IF group vs. −19.19 ± 64.28 for the IP group, P = 0.012).
In the IF group, the difference between the mean MH-D and mean F-D at 1, 3, 6, and 12 months was not significant (all P > 0.05) (Fig. 4A).The differences between the mean MH-S and the mean F-S as well as the mean MH-I and the mean F-I at 1, 3, 6, and 12 months were not significant (all P > 0.05) (Fig. 4B, C).
In the IP group, the mean F-D was significantly shorter than the mean MH-D at 1, 3, 6, and 12 months (Fig. 4A). The mean F-S at 12 months were shorter than the mean MH-S (P = 0.027) (Fig. 4B). The mean F-I at 1, 3, 6, and 12 months were not significantly different from the mean MH-I distance (Fig. 4C).
After 1 month, four IF cases remained open, with thin flaps overlying the MH detected in two cases (Supplementary Fig. 6). The MH eventually closed within 6 months postoperatively. The other two cases did not spontaneously close after the initial operation. One patient in whom the flap unfolded back to its original place before postoperative month 1, probably due to early loss of gas tamponade, underwent a successful second operation with IP. In the IP group, the MHs in two cases failed to close after the initial operation.
All cases showed postoperative DONFL (Supplementary Fig. 7). The months at which DONFL was first detected was not significantly different (3.00 months [IQR, 1.50–3.00] vs. 3.00 months [IQR, 3.00–3.00], P = 0.511). In the IF group, however, all DONFLs were limited to the superior fovea, where the ILM was peeled.
Discussion
Our analysis provided better control of confounding factors, which were previously not fully accounted for. Visual recovery and microstructural restoration were different during the early and late postoperative periods. The IF group not only showed better BCVA at 1, 3, 6, and 12 months, but also promoted earlier visual recovery at 1 month. Trends for ELM, EZ, and foveal detachment recovery was superior in the IF group. The rate of restoration of EZ < 250 μm was significantly higher at 1 month in the IF group. Significant improvement in the recovery of the IZ layer began at 6 and 12 months in the IF group. Moreover, the rate of foveal gliosis was significantly lower in the IF group at 1, 3, and 12 months. In the IF group, the ONL thickness showed trend for increasing thickness with time. The ONL thickness in the IP group showed a significant decrease from postoperative months 1 to 3, which did not recover up to postoperative month 12. In the IF group, there was no significant trend of displacement of the foveal centre toward the optic disc, superonasal retinal vasculature, or inferonasal retinal vasculature. In the IP group, the foveal centre was significantly displaced toward the optic disc at 1, 3, 6, and 12 months, and showed a trend of sequential displacement toward the superonasal and inferonasal retinal vasculature after the operation.
We hypothesise that for the IF group, once the flap is stably attached to the edge of MH, it may render resistance to centrifugal movement of the retina during MH closure, which is exerted by the horizontal contraction of the astrocytic network in the nerve fibre and ganglion cell layers as well as Müller cells of the foveal walls [1, 26]. As neurotrophic factors and basic fibroblast growth factor from the flap promote migration and proliferation of retinal cells within the cystic space underneath the flap [27], this space, which sometimes exists as a cyst or glial tissue, is replaced by more physiologic retinal cells (Supplementary Fig. 6A, arrowheads). This difference matches the data from this study in which higher incidence of foveal gliosis was noted in the IP group even from the early postoperative period. Once the space sufficiently changes into the retinal tissue, the fovea thickens and becomes resistant to centrifugal forces. This finding is more prevalent after the IF technique as the flap can serve as scaffold for foveal reorganisation once gas disappears. For IP cases in the early postoperative period, centripetal movement of the inner retinal tissues results in increased foveolar thickness [6]. Since IP cases lack the flap, they are more susceptible to centrifugal forces during subsequent remodelling of the fovea, resulting in significant foveolar ONL thinning. A previous study described centrifugal foveal tissue elongation after IP surgery [28], seen as increased horizontal and vertical inter-outer plexiform (OPL) distance up to 6 months postoperatively, and that the degree of asymmetry between horizontal and vertical distances was associated with postoperative metamorphopsia. Although investigating the direct correlation between the change in foveolar ONL thickness and the change in inter-OPL distance is beyond the scope of this study, foveal remodelling may play an important role in these processes [6] and postoperative visual function.
Müller cell-mediated centripetal displacement of photoreceptor cells is one of the main mechanisms for MH closure [7, 26, 29]. The visual outcomes of MH surgery are dependent on restoring the outer retina [30,31,32,33]. A significantly higher rate of eyes with EZ defect <250 μm would likely have resulted in greater visual acuity at 1 month postoperatively in the IF group. The mechanism of hole closure in IF share similarities with surgical closure and spontaneous closure of small MHs. One common pathway involved in the MH-sealing process is Müller cell and astrocyte proliferation initiating in the inner retina, which fills the tissue defect [34]. For IF cases, the flap may initially serve as a bridge during this process at the level of the ELM and ONL, followed by the restoration of the EZ. Further healing processes can reduce EZ defects to smaller OFMD, which can eventually disappear with full EZ restoration [34,35,36]. A similar phenomenon was also reported in spontaneous MH closure in macular telangiectasia type 2, in which the intact ILM drape may facilitate the bridging mechanism [37, 38]. In addition, another MH surgical technique that can preserve peri-foveal Müller cells and take advantage of their function is foveal sparing ILM peeling surgery. It has been reported that this technique resulted in a high closure rate, improved foveal morphology, greater improvement in foveal retinal sensitivity, and better postoperative BCVA compared to the traditional IP technique [39, 40].
A higher rate of IZ restoration was observed in the IF group. One reason is that the higher incidence of foveal gliosis in the IP group may prevent the restoration of foveolar IZ. Direct contact between ONL and RPE has been suggested to promote foveal gliosis [26]. The flap could prevent ONL from directly contacting the RPE and induce guided foveal remodelling, reducing the incidence of gliosis. Additionally, greater resistance against the centrifugal force in the IF group could promote a higher density of photoreceptors in the foveola. In contrast, the IP group was more susceptible to the centrifugal force, resulting in ONL thinning and foveal movement toward the optic disc.
Foveal movement toward the optic disc after ILM peeling has been reported [20, 41,42,43,44]. In one study which compared the foveal movement after ILM peeling and spontaneous MH closure, the MH-D and F-D were not different in eyes with spontaneous MH closure [20]. We showed similar results, in which the IF group with minimal ILM peeling area showed comparable MH-D and F-D. Although the exact mechanism requires further investigation, bare nerve fibres from ILM peeling might be more likely to be influenced by intravitreal chemical factors, resulting in shrinkage [42]. Optic nerve fibre tethering at the lamina cribrosa causes movement toward the optic disc after shrinkage of the fibres [42]. Many studies have reported negative effects of postoperative foveal displacement. In epiretinal membrane surgery, the extent of tractional foveal dystopia is correlated with a decrease in visual acuity [45]. A different study suggested that horizontal stretching initiated by foveal displacement might damage deep capillary plexuses (DCP), delaying postoperative remodelling and restoration of the DCP [41]. Additional effects of nasal movement include pseudoesotropia and asymmetrical recovery of cone photoreceptor outer segments [20, 43]. Therefore, we believe that the IF group was more likely to have superior anatomical and functional outcomes.
Delayed FTMH closure after IF surgery with a thin flap overlying the MH, or flap closure, has been described [46,47,48,49]. Studies have reported delayed closure rates of 9.8–16.1% [46,47,48,49]. For each study, nearly all flap closure configuration disappeared within 12 months. In our study, two IF cases (7.7%) showed flap closure, which eventually closed into U-shape within 3 and 6 months for each of the two cases. One case showed complete restoration of ELM, EZ, and IZ and the other case showed restoration of ELM with a small defect (<250 μm) of EZ and IZ by 12 months. Flap closure may be an advantage of the IF technique, since these cases could have failed with the IP technique [47]. Although MHs with larger MLD and BD have greater chance of flap closure [47], one case in our study showed MLD of 296 μm. As more studies show the efficacy of the IF technique regardless of MH size [13], the flap closure pattern may be a specific feature of the IF technique which could be associated with other factors, such as the effectiveness of the tamponade, speed of retinal cells to migrate and proliferate to fill up the void, and the property of each ILM to promote retinal cell migration and proliferation.
There was no significant difference in the median postoperative month at which DONFL was detected [11]. However, the IF technique drastically reduced the area of DONFL because only the superior portion of the ILM was peeled. The foveal shape in the IF group was also more physiologic than that in the IP group (Supplementary Fig. 7). While DONFL may not significantly affect visual acuity [9, 11, 50, 51], it is associated with subtle ultrastructural retinal changes, possibly manifesting as decreased central retinal sensitivity [52, 53], increased paracentral scotomata [54], and macular dysfunction [55, 56]. Therefore, we believe that the IF technique is more advantageous in minimising the DONFL area and preserving retinal function.
The limitations of this study include the small sample size and the exclusion of data for high myopia and MH retinal detachment cases. However, by propensity score matching, we minimised potential bias. The IF technique was a superior inverted flap with single-layer ILM; thus, our finding may not be generalised to other types of IF techniques. Additionally, our study did not investigate postoperative visual quality. Data from microperimetry, contrast sensitivity test, and metamorphopsia test could provide subtle differences in visual quality. Regarding propensity score matching, though we have used clinically relevant and objective factors in the matching, there may be other undefinable or subjective factors such as symptom duration that might influence the matching analysis.
In conclusion, the IF technique promoted superior vision earlier and faster recovery of outer retinal layers with a lower rate of gliosis and was more protective against foveal ONL thinning, displacement toward the optic disc, and DONFL. Thus, the IF technique should be considered as the treatment of choice for both small and large MHs.
Summary
What was known before
-
For large MHs, the IF technique shows greater MH closure rate compared to the IP technique. However, long-term visual and anatomical outcomes for the IF technique for both small and large MHs have not been extensively investigated.
What this study adds
-
Using propensity score matching, we showed that the IF technique is superior to the IP technique in terms of earlier recovery of vision and faster recovery of outer retinal layers with a lower rate of gliosis. The IF technique was also more protective against foveal ONL thinning, displacement toward the optic disc, and DONFL. The IF technique should be considered as the treatment of choice for both small and large MHs.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Bringmann A, Syrbe S, Gorner K, Kacza J, Francke M, Wiedemann P, et al. The primate fovea: structure, function and development. Prog Retin Eye Res. 2018;66:49–84. https://doi.org/10.1016/j.preteyeres.2018.03.006.
Yamada E. Some structural features of the fovea centralis in the human retina. J Archives Ophthalmology 1969;82:151–9. https://doi.org/10.1001/archopht.1969.00990020153002.
Gass JD. Muller cell cone, an overlooked part of the anatomy of the fovea centralis: hypotheses concerning its role in the pathogenesis of macular hole and foveomacualr retinoschisis. Arch Ophthalmol. 1999;117:821–3. https://doi.org/10.1001/archopht.117.6.821.
Syrbe S, Kuhrt H, Gartner U, Habermann G, Wiedemann P, Bringmann A, et al. Muller glial cells of the primate foveola: an electron microscopical study. Exp Eye Res. 2018;167:110–7. https://doi.org/10.1016/j.exer.2017.12.004.
Bringmann A, Unterlauft JD, Wiedemann R, Barth T, Rehak M, Wiedemann P. Two different populations of Muller cells stabilize the structure of the fovea: an optical coherence tomography study. Int Ophthalmol. 2020;40:2931–48. https://doi.org/10.1007/s10792-020-01477-3.
Chung H, Byeon SH. New insights into the pathoanatomy of macular holes based on features of optical coherence tomography. Surv Ophthalmol. 2017;62:506–21. https://doi.org/10.1016/j.survophthal.2017.03.003.
Bringmann A, Duncker T, Jochmann C, Barth T, Duncker GIW, Wiedemann P. Spontaneous closure of small full-thickness macular holes: Presumed role of Muller cells. Acta Ophthalmol. 2020;98:e447–e56. https://doi.org/10.1111/aos.14289.
Tadayoni R, Paques M, Massin P, Mouki-Benani S, Mikol J, Gaudric A. Dissociated optic nerve fiber layer appearance of the fundus after idiopathic epiretinal membrane removal. Ophthalmology. 2001;108:2279–83. https://doi.org/10.1016/s0161-6420(01)00856-9.
Ito Y, Terasaki H, Takahashi A, Yamakoshi T, Kondo M, Nakamura M. Dissociated optic nerve fiber layer appearance after internal limiting membrane peeling for idiopathic macular holes. Ophthalmology. 2005;112:1415–20. https://doi.org/10.1016/j.ophtha.2005.02.023.
Michalewska Z, Michalewski J, Nawrocki J. Continuous changes in macular morphology after macular hole closure visualized with spectral optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2010;248:1249–55. https://doi.org/10.1007/s00417-010-1370-5.
Mitamura Y, Ohtsuka K. Relationship of dissociated optic nerve fiber layer appearance to internal limiting membrane peeling. Ophthalmology. 2005;112:1766–70. https://doi.org/10.1016/j.ophtha.2005.04.026.
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018–25. https://doi.org/10.1016/j.ophtha.2010.02.011.
Baumann C, Dervenis N, Kirchmair K, Lohmann CP, Kaye SB, Sandinha MT. Functional and morphological outcomes of the inverted internal limiting membrane flap technique in small-sized and medium-sized macular holes <400 microm. Retina. 2021;41:2073–8. https://doi.org/10.1097/IAE.0000000000003160.
Ramtohul P, Parrat E, Denis D, Lorenzi U. Inverted internal limiting membrane flap technique versus complete internal limiting membrane peeling in large macular hole surgery: a comparative study. BMC Ophthalmol. 2020;20:11. https://doi.org/10.1186/s12886-019-1294-8.
Hung JH, Horng YH, Chu HC, Li MS, Sheu SJ. Tailored internal limiting membrane flap technique for primary macular hole. Graefes Arch Clin Exp Ophthalmol. 2020;258:759–66. https://doi.org/10.1007/s00417-019-04596-5.
Rizzo S, Tartaro R, Barca F, Caporossi T, Bacherini D, Giansanti F. Internal limiting membrane peeling versus inverted flap technique for treatment of full-thickness macular holes: a comparative study in a large series of patients. Retina. 2018;38:S73–s8. https://doi.org/10.1097/iae.0000000000001985.
Chou HD, Liu L, Wang CT, Chen KJ, Wu WC, Hwang YS, et al. Single-layer inverted internal limiting membrane flap versus conventional peel for small- or medium-sized full-thickness macular holes. Am J Ophthalmol. 2022;235:111–9. https://doi.org/10.1016/j.ajo.2021.08.016.
Cohen SY, Mrejen S, Nghiem-Buffet S, Dubois L, Fajnkuchen F, Gaudric A. Outer foveal microdefects. Ophthalmol Retin. 2021;5:553–61. https://doi.org/10.1016/j.oret.2020.09.018.
Ko TH, Witkin AJ, Fujimoto JG, Chan A, Rogers AH, Baumal CR, et al. Ultrahigh-resolution optical coherence tomography of surgically closed macular holes. Arch Ophthalmol. 2006;124:827–36. https://doi.org/10.1001/archopht.124.6.827.
Kawano K, Ito Y, Kondo M, Ishikawa K, Kachi S, Ueno S, et al. Displacement of foveal area toward optic disc after macular hole surgery with internal limiting membrane peeling. Eye (Lond). 2013;27:871–7. https://doi.org/10.1038/eye.2013.99.
Yilmaz S, Mavi Yildiz A, Avci R. Foveal Displacement following Temporal Inverted Internal Limiting Membrane Technique for Full Thickness Macular Holes: 12 Months Results. Curr Eye Res 2021:1–8. https://doi.org/10.1080/02713683.2021.1945110.
D’Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–81. 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b.
Yang JM, Koh HY, Moon SY, Yoo IK, Ha EK, You S, et al. Allergic disorders and susceptibility to and severity of COVID-19: A nationwide cohort study. J Allergy Clin Immunol. 2020;146:790–8. https://doi.org/10.1016/j.jaci.2020.08.008.
Goldstone AB, Chiu P, Baiocchi M, Lingala B, Patrick WL, Fischbein MP, et al. Mechanical or biologic prostheses for aortic-valve and mitral-valve replacement. N. Engl J Med. 2017;377:1847–57. https://doi.org/10.1056/NEJMoa1613792.
Silber JH, Rosenbaum PR, Trudeau ME, Even-Shoshan O, Chen W, Zhang X, et al. Multivariate matching and bias reduction in the surgical outcomes study. Med Care. 2001;39:1048–64. https://doi.org/10.1097/00005650-200110000-00003.
Bringmann A, Unterlauft JD, Barth T, Wiedemann R, Rehak M, Wiedemann P. Muller cells and astrocytes in tractional macular disorders. Prog Retin Eye Res. 2021:100977. https://doi.org/10.1016/j.preteyeres.2021.100977.
Shiode Y, Morizane Y, Matoba R, Hirano M, Doi S, Toshima S, et al. The role of inverted internal limiting membrane flap in macular hole closure. Invest Ophthalmol Vis Sci. 2017;58:4847–55. https://doi.org/10.1167/iovs.17-21756.
Kim JH, Kang SW, Park DY, Kim SJ, Ha HS. Asymmetric elongation of foveal tissue after macular hole surgery and its impact on metamorphopsia. Ophthalmology. 2012;119:2133–40. https://doi.org/10.1016/j.ophtha.2012.05.018.
Bringmann A, Jochmann C, Unterlauft JD, Wiedemann R, Rehak M, Wiedemann P. Different modes of foveal regeneration after closure of full-thickness macular holes by (re)vitrectomy and autologous platelet concentrate. Int J Ophthalmol. 2020;13:36–48. https://doi.org/10.18240/ijo.2020.01.06.
Sano M, Shimoda Y, Hashimoto H, Kishi S. Restored photoreceptor outer segment and visual recovery after macular hole closure. Am J Ophthalmol. 2009;147:313–8. https://doi.org/10.1016/j.ajo.2008.08.002.
Kitaya N, Hikichi T, Kagokawa H, Takamiya A, Takahashi A, Yoshida A. Irregularity of photoreceptor layer after successful macular hole surgery prevents visual acuity improvement. Am J Ophthalmol. 2004;138:308–10. https://doi.org/10.1016/j.ajo.2004.03.004.
Shimozono M, Oishi A, Hata M, Kurimoto Y. Restoration of the photoreceptor outer segment and visual outcomes after macular hole closure: spectral-domain optical coherence tomography analysis. Graefes Arch Clin Exp Ophthalmol. 2011;249:1469–76. https://doi.org/10.1007/s00417-011-1681-1.
Caprani SM, Donati S, Bartalena L, Vinciguerra R, Mariotti C, Testa F, et al. Macular hole surgery: the healing process of outer retinal layers to visual acuity recovery. Eur J Ophthalmol. 2017;27:235–9. https://doi.org/10.5301/ejo.5000905.
Kang SW, Lim JW, Chung SE, Yi CH. Outer foveolar defect after surgery for idiopathic macular hole. Am J Ophthalmol. 2010;150:551–7. https://doi.org/10.1016/j.ajo.2010.04.030.
Privat E, Tadayoni R, Gaucher D, Haouchine B, Massin P, Gaudric A. Residual defect in the foveal photoreceptor layer detected by optical coherence tomography in eyes with spontaneously closed macular holes. Am J Ophthalmol. 2007;143:814–9. https://doi.org/10.1016/j.ajo.2006.12.039.
Morawski K, Jedrychowska-Jamborska J, Kubicka-Trzaska A, Romanowska-Dixon B. The analysis of spontaneous closure mechanisms and regeneration of retinal layers of a full-thickness macular hole: Relationship with visual acuity improvement. Retina. 2016;36:2132–9. https://doi.org/10.1097/IAE.0000000000001074.
Nalci H, Batioglu F, Demirel S, Ozmert E. Spontaneous closure of macular hole in a patient with macular telangiectasia type 2. Retin Cases Brief Rep. 2021;15:369–72. https://doi.org/10.1097/ICB.0000000000000812.
Chandra V, Merani R, Hunyor AP, Gillies M. Spontaneous closure of a macular hole in macular telangiectasia type 2. Journal of VitreoRetinal Diseases. 2021;5:275–80. https://doi.org/10.1177/2474126420958907.
Murphy DC, Fostier W, Rees J, Steel DH. Foveal sparing internal limiting membrane peeling for idiopathic macular holes: effects on anatomical restoration of the fovea and visual function. Retina. 2020;40:2127–33. https://doi.org/10.1097/IAE.0000000000002724.
Morescalchi F, Russo A, Bahja H, Gambicorti E, Cancarini A, Costagliola C, et al. Fovea-sparing versus complete internal limiting membrane peeling in vitrectomy for the treatment of macular holes. Retina. 2020;40:1306–14. https://doi.org/10.1097/IAE.0000000000002612.
Cho JH, Yi HC, Bae SH, Kim H. Foveal microvasculature features of surgically closed macular hole using optical coherence tomography angiography. BMC Ophthalmol. 2017;17:217. https://doi.org/10.1186/s12886-017-0607-z.
Ishida M, Ichikawa Y, Higashida R, Tsutsumi Y, Ishikawa A, Imamura Y. Retinal displacement toward optic disc after internal limiting membrane peeling for idiopathic macular hole. Am J Ophthalmol. 2014;157:971–7. https://doi.org/10.1016/j.ajo.2014.01.026.
Itoh Y, Inoue M, Rii T, Ando Y, Hirakata A. Asymmetrical recovery of cone outer segment tips line and foveal displacement after successful macular hole surgery. Invest Ophthalmol Vis Sci. 2014;55:3003–11. https://doi.org/10.1167/iovs.14-13973.
Yoshikawa M, Murakami T, Nishijima K, Uji A, Ogino K, Horii T, et al. Macular migration toward the optic disc after inner limiting membrane peeling for diabetic macular edema. Invest Ophthalmol Vis Sci. 2013;54:629–35. https://doi.org/10.1167/iovs.12-10907.
Lo D, Heussen F, Ho HK, Narala R, Gasperini J, Bertoni B, et al. Structural and functional implications of severe foveal dystopia in epiretinal membranes. Retina. 2012;32:340–8. https://doi.org/10.1097/IAE.0b013e31821dbb35.
Tsui MC, Yang CM. Early and late macular changes after the inverted internal limiting membrane flap technique for a full-thickness macular hole. Retina. 2021;41:20–8. https://doi.org/10.1097/IAE.0000000000002796.
Boninska K, Nawrocki J, Michalewska Z. Mechanism of “Flap Closure” after the inverted internal limiting membrane flap technique. Retina. 2018;38:2184–9. https://doi.org/10.1097/IAE.0000000000001861.
Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Adelman RA, Nawrocki J. Temporal inverted internal limiting membrane flap technique versus classic inverted internal limiting membrane flap technique: a comparative study. Retina. 2015;35:1844–50. https://doi.org/10.1097/IAE.0000000000000555.
Pak KY, Park JY, Park SW, Byon IS, Lee JE. Efficacy of the perfluoro-n-octane-assisted single-layered inverted internal limiting membrane flap technique for large macular holes. Ophthalmologica. 2017;238:133–8. https://doi.org/10.1159/000477823.
Mitamura Y, Suzuki T, Kinoshita T, Miyano N, Tashimo A, Ohtsuka K. Optical coherence tomographic findings of dissociated optic nerve fiber layer appearance. Am J Ophthalmol. 2004;137:1155–6. https://doi.org/10.1016/j.ajo.2004.01.052.
Imai H, Ohta K. Microperimetric determination of retinal sensitivity in areas of dissociated optic nerve fiber layer following internal limiting membrane peeling. Jpn J Ophthalmol. 2010;54:435–40. https://doi.org/10.1007/s10384-010-0839-4.
Tadayoni R, Svorenova I, Erginay A, Gaudric A, Massin P. Decreased retinal sensitivity after internal limiting membrane peeling for macular hole surgery. Br J Ophthalmol. 2012;96:1513–6. https://doi.org/10.1136/bjophthalmol-2012-302035.
Ripandelli G, Scarinci F, Piaggi P, Guidi G, Pileri M, Cupo G, et al. Macular pucker: to peel or not to peel the internal limiting membrane? A microperimetric response. Retina. 2015;35:498–507. https://doi.org/10.1097/IAE.0000000000000330.
Haritoglou C, Gass CA, Schaumberger M, Ehrt O, Gandorfer A, Kampik A. Macular changes after peeling of the internal limiting membrane in macular hole surgery. Am J Ophthalmol. 2001;132:363–8. https://doi.org/10.1016/s0002-9394(01)01093-5.
Lim JW, Kim HK, Cho DY. Macular function and ultrastructure of the internal limiting membrane removed during surgery for idiopathic epiretinal membrane. Clin Exp Ophthalmol. 2011;39:9–14. https://doi.org/10.1111/j.1442-9071.2010.02377.x.
Terasaki H, Miyake Y, Nomura R, Piao CH, Hori K, Niwa T, et al. Focal macular ERGs in eyes after removal of macular ILM during macular hole surgery. Invest Ophthalmol Vis Sci. 2001;42:229–34.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (Ministry of Science and ICT) (No. 2019R1A2C2086729). The funding organisation had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
JJK and SHB made substantial contributions to the conception and design of the work. JJK and SHB collected and analysed the data. JJK and SHB interpreted the data. JJK drafted and all the authors substantively revised the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kwak, J.J., Byeon, S.H. Comparison of long-term visual and anatomical outcomes between internal limiting membrane flap and peeling techniques for macular holes with a propensity score analysis. Eye 37, 1207–1213 (2023). https://doi.org/10.1038/s41433-022-02103-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02103-5