Abstract
Background
The XEN45 Gel Stent is a subconjunctival filtering device that has demonstrated promising efficacy. This meta-analysis quantitatively evaluates reported complications and interventions after XEN45 implantation in the treatment of open angle glaucoma (OAG).
Methods
Pilot, cohort, observational studies, and randomised controlled trials that included at least ten patients undergoing ab interno or externo XEN45 surgery, with or without phacoemulsification were deemed eligible for inclusion. A meta-analysis of proportions with random-effect models was performed using the meta routine in R version 3.2.1. Outcomes included the rate of complications and post-operative interventions.
Results
One hundred and fifty-two studies were identified on initial literature search and 33 were included in final analysis. Numerical hypotony was the most common post-operative complication, involving 20% of patients (95% CI: 10–31%). Post-operative gross hyphema occurred in 14% (95% CI: 7–22%) and transient intra-ocular pressure (IOP) spikes (>30 mmHg) in 13% (95% CI: 4–27%). Stent exposure occurred in 1% (95% CI: 0–2%). Stent migration occurred in 1% (95% CI: 0–3%). XEN45 revision and/or a second XEN45 implantation was performed in 5% of patients (95% CI: 3–7%). Stent relocation was performed in 3% (95% CI: 1–7%). A second glaucoma procedure was performed in 11% (95% CI: 8–15%). 26% underwent one (95% CI: 17–36%), 13% underwent two (95% CI: 5–24%) while 4% underwent three (95% CI: 2–6%) bleb needling procedures. 35% of patients (95% CI: 29–40%) required at least one needling. The average rate of needling per patient was 0.38 (95% CI: 0.20–0.59). However, there is a lack of high-quality data, with 8 of the 33 studies assessed to have a moderate to high risk of bias.
Conclusions
While literature suggests that XEN45 Gel Stent implantation is safe in the treatment of OAG, the overall current level of evidence is low and further studies are needed. More than a third of patients require at least one post-operative bleb needling procedure.
Similar content being viewed by others
Introduction
Glaucoma is the most common cause of irreversible blindness worldwide [1]. Intra-ocular pressure (IOP) remains the primary modifiable risk factor, with effective IOP reduction being shown to prevent progressive optic nerve damage and visual field impairment [2]. While ocular hypotensive medications are used as first-line therapy, they are subject to patient adherence, ocular surface toxicity and other local and systemic side effects [3]. Surgical intervention in the form of glaucoma filtering procedures is indicated when maximal medical therapy fails to ensure adequate IOP reduction [4, 5].
Minimally Invasive Glaucoma Surgery (MIGS) techniques have emerged in the past decade, characterised by ab interno device implantation, little or no scleral dissection, minimal local trauma, high safety profile and rapid post-operative recovery [6, 7]. The XEN45 Gel Stent is a MIGS device that involves creation of a subconjunctival filtration bleb, as in traditional trabeculectomy. It is FDA-approved for use in refractory glaucoma with failed previous surgical treatment and in open-angle glaucoma unresponsive to maximum tolerated medical therapy [8].
MIGS techniques are often marketed as procedures with a higher safety profile than traditional subconjunctival filtration surgery [9,10,11]. However, XEN45 implantation is not without risks. In contrast to trabeculectomy, XEN45 is a device-based surgery that may have device-related complications, such as stent migration and extrusion, in addition to other complications such as hypotony, transient IOP spikes and endophthalmitis [12,13,14]. Secondary interventions may be necessary to address these complications, including anterior chamber reformation, implant relocation and bleb revision. Furthermore, post-operative bleb manipulation and needling procedures are employed to manage suboptimal IOPs due to encapsulation and bleb fibrosis. However, there is a paucity of quantitative information in current literature on the risk of these post-operative complications and incidence of secondary interventions [15, 16].
In a prior meta-analysis [17], our group compared surgical outcomes of standalone XEN45 implantation with combined XEN45-phacoemulsification surgery. However, we were unable to compare safety profiles then, as insufficient papers had reported surgical complications and post-operative interventions. The potential to analyse a larger data pool, from a greater number of studies of a wider context from those previously included in our earlier synthesis, justified a separate review.
This present systematic review and meta-analysis therefore aims to characterise the safety profile of XEN45 Gel Stent implantation by quantitatively evaluating the risk of surgical complications and incidence of post-operative interventions.
Methods
Study selection
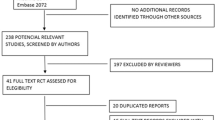
A comprehensive search of MEDLINE, EMBASE, Current Contents, Cochrane Central Register of Controlled Trials (CENTRAL) databases was performed. A combination of subject headings and text words were used as needed to define XEN45 surgery. We employed the terms ‘Xen surgery’ to ensure a comprehensive search, followed by selective vetting. The search workflow was in adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [18].
Identified studies were assessed independently by two authors (SYL, BKB) to determine eligibility for inclusion in the analysis. Pilot, cohort, observational studies, and randomised controlled trials that included at least 10 patients undergoing XEN45 surgery, for the treatment of open angle glaucoma (OAG) were deemed to be eligible for inclusion. Case reports, review articles, studies involving less than 10 patients and duplicate data were excluded. Articles not written in English were also excluded from the study.
Primary outcomes included the rate of surgical complications and post-operative interventions. Outcomes were only analysed if they were reported by three or more papers.
The following information from each study was extracted manually from full text: first author, year of publication, study design, study period, country of origin, number of patients in study, mean age of patients, patient gender, type of intervention and complication rates. Where there was a difference in opinion, a senior author was consulted.
Where more information was required, corresponding authors of articles were contacted to the best of our ability.
Statistical analysis
A meta-analysis of proportions was performed (BKB, SYL) with data available on the complication and intervention rates using the meta routine [19] in R version 3.2.1 [20]. The Freeman-Tukey double arcsine transformation was implemented to calculate an overall proportion. To assess heterogeneity between the studies, I2 was quantified, which estimates the percentage of variability between studies. An I2 of >75% suggested considerable heterogeneity. Random-effect models were used in view of the heterogeneity of the studies. P values < 0.05 were considered statistically significant.
Risk of bias and quality assessment
Two authors (BKB, SYL) independently assessed the included studies for the risk of several biases, including selection, performance, detection, attrition, and selective reporting bias. We deemed there to be a high risk of attrition bias if the follow-up rate was <50%. Performance bias was determined to be low risk in publications where no subjective patient-reported outcomes were used even in the absence of participant blinding. Risk of Bias in Non-Randomised Studies—of Intervention (ROBINS-I) tool was used to evaluate the quality of evidence for each outcome measure (Supplementary Table 1).
Results
One hundred and fifty-two studies were found on the initial literature search governed by PRISMA on 10th April 2020. After full text evaluation and a secondary search of the references of each paper, 33 studies were identified for inclusion [10, 12,13,14, 21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49]. Of these, ten papers [10, 21,22,23,24,25,26,27,28,29] performed standalone XEN45 surgery and combined XEN45 with phacoemulsification (XEN45-Phaco) with distinct reporting of outcomes; 17 papers performed standalone XEN45 surgery and XEN45-Phaco but reported the outcomes together; five papers performed standalone XEN45 surgery only; three papers performed XEN45-Phaco only.
We analysed the outcomes of XEN45 surgery in 3062 eyes, with representation across the Caucasian, African-American, Mexican, Latino and Asian populations. There were 15 prospective studies and 18 retrospective studies, with majority being of case series design. Maximum follow-up duration ranged from 6 months to 36 months with most studies ending follow-up at 12 months. Amongst the papers which reported age, the mean (SD) age of patients was 67.02 (11.93). A summary of each study design, study period, population, patient characteristics is shown in Table 1.
Across the studies, a variety of surgical techniques for XEN45 Gel Stent implantation were employed. However, the general steps of surgery were largely consistent and are as follows. The corneal main and side port incisions are created, followed by the instillation of the anterior chamber (AC) with viscoelastic. The needle tip of the preloaded injector is inserted through the main incision or a separate corneal incision and advanced across the AC towards the supero-nasal quadrant with advancement through the sclera. A second instrument at the side port is used to provide stabilisation and countertraction. The needle and needle tip bevels are then visualised in the subconjunctival space before stent deployment. The injector is then removed and the viscoelastic is aspirated. The AC is pressurised, and the formation of a subconjunctival bleb is checked. The implant is ideally placed through the scleral spur and tracked 3 mm posterior to the limbus, exiting through the sclera into the subconjunctival space. Approximately 1–2 mm of the implant is left in the AC to provide a passage from the AC into the subconjunctival space. Gonioscopic visualisation is used at the surgeon’s discretion. Intra-operative adjunctive anti-fibrotic therapy in the form of Mitomycin C (MMC) was administered in all studies. Of note, the subconjunctival injection route of MMC administration was used for all studies except for Grover et al. [41] which employed sponge-application of the MMC instead. Across the studies, MMC was applied at varying volumes (0.05–0.2 ml) and concentrations (0.01–0.02%). IOP lowering medications were stopped one day prior with no medication wash out period implemented.
Incidence of complications after XEN45 implantation
Numerical hypotony was the most common complication involving 20% of patients (95% CI: 10–31%), defined as IOP < 6 mmHg and resolving without intervention (Fig. 1). This was followed by post-operative hyphema, occurring in 14% of patients (95% CI: 7–22%). Post-operative transient IOP spike with IOP ≥ 30 mmHg occurred in 13% of patients (95% CI: 4–27%). Stent exposure occurred in 1% (95% CI: 0–2%). Stent migration occurred in 1% (95% CI: 0–3%). Hypotonous maculopathy occurred in 1% (95% CI: 0–3%). Choroidal effusion occurred in 2% (95% CI: 1–3%) while choroidal detachment occurred in 4% (95% CI: 1–7%). Dysesthetic bleb occurred in 2% (95% CI: 1–3%). Endophthalmitis was reported in 1 patient in each of 4 papers. Malignant glaucoma occurred in 1% (95% CI: 0–2%).
Complications after XEN45 implantation include (from top to bottom, left to right) – Intra- and post-operative intracameral haemorrhage and hyphema; stent exposure or extrusion; stent migration; numerical hypotony; hypotonous maculopathy; transient intra-ocular pressure spike; choroidal effusion; choroidal detachment; dysesthetic bleb; endophthalmitis; malignant glaucoma or aqueous misdirection. CI confidence interval.
Incidence of interventions after XEN45 implantation
2% of patients had a shallow anterior chamber (95% CI: 1–4%), while 1% had a shallow anterior chamber requiring reformation (95% CI: 0–3%) (Fig. 2). XEN45 revision or 2nd XEN45 implantation was performed in 5% of patients (95% CI: 3–7%). Stent relocation was performed in 3% (95% CI: 1–7%). A second glaucoma procedure was performed in 11% (95%CI: 8–15%). 26% of patients underwent one bleb needling procedure (95% CI: 17–36%), 13% underwent two needling procedures (95% CI: 5–24%) while 4% underwent three needling procedures (95% CI: 2–6%). 35% of patients (95% CI: 29–40%) required at least 1 needling procedure over the entire follow-up period. The average rate of needling procedures per patient was 0.38 (95%CI: 0.20–0.59).
Interventions after XEN45 implantation include (from top to bottom, left to right) – 2nd XEN45 implantation or XEN45 revision; XEN45 relocation; secondary glaucoma procedures; post-operative laser procedure; mean number of needling procedures per patient; proportion of patients requiring needling procedures; proportion of patients undergoing 1 needling procedure; proportion of patients undergoing 2 needling procedures; proportion of patients undergoing 3 needling procedures; shallow anterior chamber; shallow anterior chamber requiring reformation. CI confidence interval.
Discussion
In this meta-analysis evaluating the safety profile of XEN45 implantation, we found that the incidence of post-operative complications was low, as well as often transient and self-resolving in nature. However, post-operative intervention rates were relatively high.
Complications after XEN45 implantation
Most reported cases of hypotony were that of numerical hypotony, which resolved without intervention and were not clinically significant. This may have been attributable to early peri-stent leak and the effect of medications that had not yet completely washed out during this early post-operative period. Some rare complications of hypotony were reported—hypotonous maculopathy was described in 5 patients by Karimi et al. [22] in 1 patient by Mansouri et al. [23] and in 2 patients by Schlenker et al. [14]. The low incidence of clinically significant hypotony is unsurprising, given the design of the XEN45 stent, which has been modelled on the Hagen-Poiseuille equation [50, 51]. Prior flow testing demonstrated the implant’s ability to maintain a steady-state pressure above numerical hypotony levels [51].
While our study did not aim to compare complication rates between XEN45 implantation and trabeculectomy, we highlight some observations from some comparative studies included in our analysis. Schlenker et al. [14] demonstrated that trabeculectomy eyes experienced more transient complications than XEN45 surgery, which were mostly contributed by bleb leaks and dehiscence. They reported 2 cases and 1 case of hypotonous maculopathy in the XEN45 and trabeculectomy groups respectively. These cases subsequently resolved, though no details were given. In another comparative study, Marcos Parra et al. [10] noted that the incidence of hyphema and anterior chamber flattening was significantly greater in the trabeculectomy group than in the XEN45 group.
Transient post-operative IOP spikes (IOP ≥ 30 mmHg) occurred in 13% of patients, all of whom required no intervention. Post-operative hyphema (occurring in 14% of patients in our analysis) and retained viscoelastic may have contributed to this early, transient elevation of IOP. Stent exposure was uncommon, but still occurred in 1% of patients and presents a risk of endophthalmitis. Of note, stent exposure and erosion has been shown to occur despite the ability of the XEN45 stent to conform to tissue after swelling upon contact with water [52]. Other case reports have described implant dislocation [53] which at times may necessitate implant removal and re-implantation. Choroidal effusion occurred in 2% of patients. Most studies did not describe any further association with concurrent hypotony, the type of effusion (serous or haemorrhagic), the absence or presence of accompanying symptoms and visual outcomes. Most resolved with conservative management. Grover et al. [41] reported 2 cases unrelated to hypotony which extended posterior to the equator without haemorrhage. Karimi et al. [22] reported 4 cases which lasted more than 1 month and extended posterior to the equator. Smith et al. [29] reported 2 cases, both of which were associated with hypotony. One case developed in the early post-operative period requiring revision surgery, while the other developed in the late post-operative period with severe choroidal effusions following tube revision, necessitating further revision with a pericardial patch graft. Dysesthetic blebs occurred in 2% of patients. Karimi et al. [22] reported 6 cases of large, overhanging dysesthetic blebs which required post-operative lancing, application of a bandage contact lens, cryotherapy to the conjunctiva or subsequent bleb revisions. Olgun et al. [24] and Grover et al. [41] reported one case of a hypertrophic and a dysesthetic bleb respectively, but did not specify symptoms or the need for further management.
Major complications were rare and there was a very low incidence of severe, sight-threatening complications. 4 cases of malignant glaucoma were reported in Schlenker et al. [14]. 1 case of malignant glaucoma was reported in Fea et al. [25] which subsequently underwent vitrectomy with irido-zonular-hyaloidectomy. 1 case of malignant glaucoma was reported in Heidinger et al. [13] which necessitated vitrectomy. 1 case of endophthalmitis was reported each in Reitsamer et al. [28], Gillman et al. [38], Heidinger et al. [13], Karimi et al. [22] and Sng et al. [48].
Interventions after XEN45 implantation
Bleb needling has been established as an effective [54, 55] post-operative procedure that aims to re-establish aqueous outflow through the disruption of fibrosis after bleb-forming, subconjunctival drainage surgeries. A sizable proportion of patients in our analysis (35%) required at least 1 needling procedure post-operatively, with an average rate of 0.38 needlings per patient. Most required only one needling (26%) while a minority required three needlings (4%). In terms of mean number of days to first needling, Gillmann et al. [38], Lenzhofer et al. [56], Mansouri et al. [23] reported a mean of 143.8, 137 and 136 days respectively. Reitsamer et al. [28] reported a mean (SD) time to first needling of 152 (160) with a median of 90 days. Heidinger et al. [13] reported a range of 6 to 582 days for time of needling, with a median of 59.5 days while Hengerer et al. [37] did not specify but reported all needling procedures taking place between POW1 to POM3. In terms of the number of needling procedures conducted as a proportion of eyes included in the study, needling was performed in 39.1% (n = 975/2493) of eyes, in studies which reported needling rates. The needling rate was markedly higher in Fea et al. [25] (n = 147/171, 85.9%) and lower in De Gregorio et al. [39] (n = 1/41, 2.4%). Most needling procedures were performed at the slit lamp. Fea et al. [34] performed needling at the slit lamp or in the operating room, according to surgeon preference. Kalina et al. [21] performed all needlings under microscopic guidance in a procedure room while Gillmann et al. [38] and Mansouri et al. [23] performed all needlings under surgical microscope in the operating theatre.
There is likely to be significant variability in the indication, threshold and method of post-operative bleb needling across studies. The decision for needling is left to the surgeon’s discretion, with consideration of patient preference. Other factors affecting the decision to needle may include the target IOP, the risk of recurrence of fibrosis, whether the needling is performed at the slit lamp or in the operating theatre, and bleb morphology, which has been correlated with the performance of a filtering bleb [34, 57, 58]). Higher needling rates may reflect a more proactive approach to needling, while lower needling rates may conversely reflect a more conservative approach. Explicit indications for needling were not detailed by the studies. In our review, most papers did not report the timepoints at which needling was carried out, or criterion for needling, making meaningful comparison difficult. However, Grover et al. [41] did define the criteria for needling as a flat bleb with absence of microcysts, fibrotic or blocked bleb filtration area and high risk of bleb failure based on investigator assessment. Of note, the last criteria was still open to surgeon discretion. Sng et al. [48] reported a criterion of an absence of a subconjunctival filtering bleb and IOP ≥ 21 mmHg. Furthermore, in recent times, modifications to XEN45 implantation surgery have been made in an attempt to reduce post-operative bleb fibrosis and needling rates, including increasing the dose and concentration of intra-operative MMC, performing needling at the time of primary surgery, as well as performing open conjunctival surgery to ensure a sub-tenon’s placement of the stent. Most studies did not provide these details. Nonetheless, overall in comparison to trabeculectomy surgery, it may appear that higher rates of needling can be expected after XEN45 implantation surgery [10, 14].
A second glaucoma procedure was performed in 11% (95%CI: 8–15%) of patients. Of the studies that reported rates of second glaucoma procedure, many did not describe the specifics of the second procedure (Supplementary Table 2). However, we note that a majority of second glaucoma procedures, where described, were trabeculectomies.
Risk of bias
All 33 manuscripts included in this meta-analysis were assessed for sources of bias using the ROBINS-I Tool (Supplementary Table 1). A low to moderate risk of bias across all domains was determined in 28 studies. Five papers were deemed to have serious risk of bias [13, 22, 29, 32, 35].
Karimi et al. [22] and Heidinger et al. [13] reported a 73 and 56% loss to follow-up at the 12-month mark respectively. Fernandez-Garcia et al. [35], Dar et al. [32] and Smith et al. [29] excluded otherwise eligible patients that did not attend follow-up, subjecting data to selection bias.
Limitations and further considerations
First, studies included in this review only reported outcomes up till the end of their follow-up period, which ranged from 6 to 36 months (most commonly 12 months). Longer-term safety profiles beyond this timepoint could not be analysed. Second, most included studies were retrospective in nature. Selection and observation biases, as well as confounding factors, are inherent limitations of retrospective studies. This reduces the level of evidence of a systematic review. Third, this review was not prospectively registered and could be subject to reporting bias. While we adhered to our pre-planned protocol, knowledge of potential includable reports could influence key components of the review process such as criteria for study selection, target population and outcomes to be assessed. Fourth, the specific timepoints at which various complications and interventions occurred were not reported. Knowledge of these timepoints would have allowed survival analysis and may have enabled postulation of underlying causes of these complications, as well as better anticipation of post-operative interventions. Fifth, XEN45 implantation is performed as either a standalone procedure or in combination with phacoemulsification surgery. Because most included papers did not report results from these groups separately, we were unable to analyse these outcomes separately. The difference in outcomes between standalone trabeculectomy surgery and combined phacoemulsification-trabeculectomy surgery is well understood. Differences in complication and post-operative intervention rates between standalone XEN45 and combined XEN45-phacoemulsification surgery may similarly be expected [59]. Sixth, post-operative complications and intervention rates may be related to patient and ocular factors, including age, scleral thickness, and diabetic status. However, data on these factors was largely not available for analysis. Seventh, ethnicity has been shown to impact trabeculectomy outcomes [60, 61], hypothesised to be due to differing rates of healing and fibrosis [62]. It is reasonable to assume similar ethnic differences in fibrosis after XEN45 Gel Stent implantation, also a subconjunctival bleb-forming surgery. However, differences in outcome between ethnicities could not be further explored as most studies included a mix of ethnicities. Eighth, initial surgical learning curves in XEN45 Gel Stent implantation are likely to affect outcomes and incidence of complications and interventions. This has been acknowledged in some papers [33, 46, 63]. Ninth, heterogeneity levels across included studies were high, reaching I2 values of >90% in several of our models. While excessive clinical diversity in our included studies restricted our ability to derive overall effect estimates, this was expected due to variations in glaucoma sub-type, population size, baseline IOP, number of IOP lowering medications and follow-up durations.
Conclusions
XEN45 Gel Stent implantation is an effective surgical modality in the treatment OAG, with a low incidence of complications but a relatively high incidence of post-operative interventions. There is currently a lack of high‐quality evidence available regarding the safety of XEN45 implantation for OAG. Properly designed randomised controlled trials (RCTs) which compare the medium‐ and long‐term safety of the XEN45 Gel Stent compared to conventional medical, laser and surgical treatments for OAG may be useful. It was observed that there was significant heterogeneity of data reporting across studies. The World Glaucoma Association Guidelines on Design & Reporting Glaucoma Trials [64] provide a clear, standardised guide for reporting of complications specific to glaucoma drainage device surgery. Detailed reporting of event timepoints will also be useful in facilitating survival analysis.
Summary
What was known before
-
The XEN45 Gel Stent is a subconjunctival bleb-forming MIGS device used in the treatment of OAG.
-
Known post-operative complications include hyphema, transient numerical hypotony, intra-ocular pressure spikes, stent migration and extrusion, as well as endophthalmitis.
-
Secondary bleb interventions, including needling, may be required after surgery.
What this study adds
-
Review and meta-analysis of current literature suggests a low incidence of complications and secondary glaucoma procedures after XEN45 Gel Stent implantation.
-
However, there is a relatively high incidence of post-operative bleb needling.
-
Overall, there remains a lack of high‐quality, longer-term evidence regarding the safety of XEN45 Gel Stent implantation in the treatment of OAG.
References
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–7.
Pillunat LE, Erb C, Junemann AG, Kimmich F. Micro-invasive glaucoma surgery (MIGS): a review of surgical procedures using stents. Clin Ophthalmol. 2017;11:1583–600.
Lemij HG, Hoevenaars JG, van der Windt C, Baudouin C. Patient satisfaction with glaucoma therapy: reality or myth? Clin Ophthalmol. 2015;9:785–93.
Musch DC, Gillespie BW, Niziol LM, Lichter PR, Varma R, Group CS. Intraocular pressure control and long-term visual field loss in the Collaborative Initial Glaucoma Treatment Study. Ophthalmology. 2011;118:1766–73.
Francis BA, Singh K, Lin SC, Hodapp E, Jampel HD, Samples JR, et al. Novel glaucoma procedures: a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118:1466–80.
Saheb H, Ahmed II. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012;23:96–104.
Lavia C, Dallorto L, Maule M, Ceccarelli M, Fea AM. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PLoS ONE. 2017;12:e0183142.
Chatzara A, Chronopoulou I, Theodossiadis G, Theodossiadis P, Chatziralli I. XEN implant for glaucoma treatment: a review of the literature. Semin Ophthalmol. 2019;34:93–7.
Wagner FM, Schuster AK, Emmerich J, Chronopoulos P, Hoffmann EM. Efficacy and safety of XEN®-Implantation vs. trabeculectomy: data of a “real-world” setting. PLoS ONE. 2020;15:e0231614.
Marcos Parra MT, Salinas Lopez JA, Lopez Grau NS, Ceausescu AM, Perez Santonja JJ. XEN implant device versus trabeculectomy, either alone or in combination with phacoemulsification, in open-angle glaucoma patients. Graefes Arch Clin Exp Ophthalmol. 2019;257:1741–50.
Basílio AL, Moura-Coelho N, Passos I, Cardoso MS, Domingues I, Reina M, et al. XEN(®) implant and trabeculectomy medium-term quality of life assessment and comparison of results. Int J Ophthalmol. 2018;11:1941–4.
Widder RA, Dietlein TS, Dinslage S, Kuhnrich P, Rennings C, Rossler G. The XEN45 Gel Stent as a minimally invasive procedure in glaucoma surgery: success rates, risk profile, and rates of re-surgery after 261 surgeries. Graefes Arch Clin Exp Ophthalmol. 2018;256:765–71.
Heidinger A, Schwab C, Lindner E, Riedl R, Mossbock G. A retrospective study of 199 Xen45 stent implantations from 2014 to 2016. J Glaucoma. 2019;28:75–9.
Schlenker MB, Gulamhusein H, Conrad-Hengerer I, Somers A, Lenzhofer M, Stalmans I, et al. Efficacy, safety, and risk factors for failure of standalone ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology. 2017;124:1579–88.
King AJ, Shah A, Nikita E, Hu K, Mulvaney CA, Stead R, et al. Subconjunctival draining minimally-invasive glaucoma devices for medically uncontrolled glaucoma. Cochrane Database Syst Rev. 2018;12:Cd012742.
Bicket AK, Le JT, Azuara-Blanco A, Gazzard G, Wormald R, Bunce C, et al. Minimally invasive glaucoma surgical techniques for open-angle glaucoma: an overview of cochrane systematic reviews and network meta-analysis. JAMA Ophthalmol. 2021;139:983–9.
Lim SY, Betzler BK, Yip LWL, Dorairaj S, Ang BCH. Standalone XEN45 Gel Stent Implantation Versus Combined XEN45-phacoemulsification in the treatment of open angle glaucoma-a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2021;259:3209–19.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–12.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60.
Team RC. R Core Team. R: a language and environment for statistical computing. Found Stat Comput. 2013.
Kalina AG, Kalina PH, Brown MM. XEN® gel stent in medically refractory open-angle glaucoma: results and observations after one year of use in the United States. Ophthalmol Ther. 2019;8:435–46.
Karimi A, Lindfield D, Turnbull A, Dimitriou C, Bhatia B, Radwan M, et al. A multi-centre interventional case series of 259 ab-interno Xen gel implants for glaucoma, with and without combined cataract surgery. Eye. 2019;33:469–77.
Mansouri K, Guidotti J, Rao HL, Ouabas A, D'Alessandro E, Roy S, et al. Prospective evaluation of standalone XEN gel implant and combined phacoemulsification-XEN gel implant surgery: 1-year results. J Glaucoma. 2018;27:140–7.
Olgun A, Aktas Z, Ucgul AY. XEN gel implant versus gonioscopy-assisted transluminal trabeculotomy for the treatment of open-angle glaucoma. Int Ophthalmol. 2020;40:1085–93.
Fea AM, Bron AM, Economou MA, Laffi G, Martini E, Figus M, et al. European study of the efficacy of a cross-linked gel stent for the treatment of glaucoma. J Cataract Refract Surg. 2020;46:441–50.
Hu JY, Ang BCH, Yip LW. Efficacy of the XEN gel stent on intraocular pressure lowering in East Asian eyes. Int Ophthalmol. 2020;40:1191–9.
Ozal SA, Kaplaner O, Basar BB, Guclu H, Ozal E. An innovation in glaucoma surgery: XEN45 gel stent implantation. Arq Bras Oftalmol. 2017;80:382–5.
Reitsamer H, Sng C, Vera V, Lenzhofer M, Barton K, Stalmans I, et al. Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2019;257:983–96.
Smith M, Charles R, Abdel-Hay A, Shah B, Byles D, Lim LA, et al. 1-year outcomes of the Xen45 glaucoma implant. Eye. 2019;33:761–6.
Buffault J, Graber M, Bensmail D, Bluwol É, Jeanteur MN, Abitbol O, et al. Efficacy and safety at 6 months of the XEN implant for the management of open angle glaucoma. Sci Rep. 2020;10:4527.
Cutolo CA, Iester M, Bagnis A, Bonzano C, Negri L, Olivari S, et al. Early Postoperative Intraocular Pressure is Associated With Better Pressure Control After XEN Implantation. J Glaucoma. 2020;29:456–60.
Dar N, Sharon T, Hecht I, Kalev-Landoy M, Burgansky-Eliash Z. Efficacy and safety of the ab interno gelatin stent in severe pseudoexfoliation glaucoma compared to non-pseudoexfoliation glaucoma at 6 months. Eur J Ophthalmol. 2019. https://doi.org/10.1177/1120672119848277.
Lenzhofer M, Kersten-Gomez I, Sheybani A, Gulamhusein H, Strohmaier C, Hohensinn M, et al. Four-year results of a minimally invasive transscleral glaucoma gel stent implantation in a prospective multi-centre study. Clin Exp Ophthalmol. 2019;47:581–7.
Fea AM, Spinetta R, Cannizzo PML, Consolandi G, Lavia C, Aragno V, et al. Evaluation of bleb morphology and reduction in IOP and glaucoma medication following implantation of a novel gel stent. J Ophthalmol. 2017;2017:9364910.
Fernandez-Garcia A, Zhou Y, Garcia-Alonso M, Andrango HD, Poyales F, Garzon N. Medium-term clinical outcomes following Xen45 device implantation. Int Ophthalmol. 2020;40:709–15.
Galal A, Bilgic A, Eltanamly R, Osman A. XEN glaucoma implant with mitomycin C 1-year follow-up: result and complications. J Ophthalmol. 2017;2017:5457246.
Hengerer FH, Kohnen T, Mueller M, Conrad-Hengerer I. Ab interno gel implant for the treatment of glaucoma patients with or without prior glaucoma surgery: 1-year results. J Glaucoma. 2017;26:1130–6.
Gillmann K, Bravetti GE, Mermoud A, Rao HL, Mansouri K. XEN gel stent in pseudoexfoliative glaucoma: 2-year results of a prospective evaluation. J Glaucoma. 2019;28:676–84.
De Gregorio A, Pedrotti E, Russo L, Morselli S. Minimally invasive combined glaucoma and cataract surgery: clinical results of the smallest ab interno gel stent. Int Ophthalmol. 2018;38:1129–34.
Ibáñez-Muñoz A, Soto-Biforcos VS, Chacón-González M, Rúa-Galisteo O, Arrieta-Los Santos A, Lizuain-Abadía ME, et al. One-year follow-up of the XEN(R) implant with mitomycin-C in pseudoexfoliative glaucoma patients. Eur J Ophthalmol. 2019;29:309–14.
Grover DS, Flynn WJ, Bashford KP, Lewis RA, Duh YJ, Nangia RS, et al. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2017;183:25–36.
Ibáñez-Muñoz A, Soto-Biforcos VS, Rodríguez-Vicente L, Ortega-Renedo I, Chacón-González M, Rúa-Galisteo O, et al. XEN implant in primary and secondary open-angle glaucoma: a 12-month retrospective study. Eur J Ophthalmol. 2019. https://doi.org/10.1177/1120672119845226.
Laroche D, Nkrumah G, Ng C. Real-world retrospective consecutive study of ab interno XEN 45 gel stent implant with mitomycin C in Black and Afro-Latino patients with glaucoma: 40% required secondary glaucoma surgery at 1 year. Middle East Afr J Ophthalmol. 2019;26:229–34.
Olate-Pérez Á, Pérez-Torregrosa VT, Gargallo-Benedicto A, Neira-Ibáñez P, Cerdà-Ibáñez M, Osorio-Alayo V, et al. Prospective study of filtering blebs after XEN45 surgery. Arch Soc Esp Oftalmol. 2017;92:366–71.
Pérez-Torregrosa VT, Olate-Pérez Á, Cerdà-Ibáñez M, Gargallo-Benedicto A, Osorio-Alayo V, Barreiro-Rego A, et al. Combined phacoemulsification and XEN45 surgery from a temporal approach and 2 incisions. Arch Soc Esp Oftalmol. 2016;91:415–21.
Post M, Lubinski W, Sliwiak D, Podboraczynska-Jodko K, Mularczyk M. XEN gel stent in the management of primary open-angle glaucoma. Doc Ophthalmol. 2020;141:65–76.
Qureshi A, Jones NP, Au L. Urgent management of secondary glaucoma in uveitis using the Xen-45 gel stent. J Glaucoma. 2019;28:1061–6.
Sng CC, Wang J, Hau S, Htoon HM, Barton K. XEN-45 collagen implant for the treatment of uveitic glaucoma. Clin Exp Ophthalmol. 2018;46:339–45.
Tan SZ, Walkden A, Au L. One-year result of XEN45 implant for glaucoma: efficacy, safety, and postoperative management. Eye. 2018;32:324–32.
De Gregorio A, Pedrotti E, Stevan G, Bertoncello A, Morselli S. XEN glaucoma treatment system in the management of refractory glaucomas: a short review on trial data and potential role in clinical practice. Clin Ophthalmol. 2018;12:773–82.
Sheybani A, Reitsamer H, Ahmed II. Fluid dynamics of a novel micro-fistula implant for the surgical treatment of glaucoma. Investig Ophthalmol Vis Sci. 2015;56:4789–95.
Arnould L, Theillac V, Moran S, Gatinel D, Grise-Dulac A. Recurrent exposure of XEN gel stent implant and conjunctival erosion. J Glaucoma. 2019;28:e37–40.
Dervenis N, Mikropoulou AM, Dervenis P, Lewis A. Dislocation of a previously successful XEN glaucoma implant into the anterior chamber: a case report. BMC Ophthalmol. 2017;17:148.
Nikita E, Murdoch I. Same-site surgical revision of failed trabeculectomy blebs with mitomycin C augmentation: long-term follow-up. Eye. 2018;32:352–8.
Anand N, Khan A. Long-term outcomes of needle revision of trabeculectomy blebs with mitomycin C and 5-fluorouracil: a comparative safety and efficacy report. J Glaucoma. 2009;18:513–20.
Lenzhofer M, Strohmaier C, Sperl P, Hohensinn M, Hitzl W, Steiner V, et al. Effect of the outer stent position on efficacy after minimally invasive transscleral glaucoma gel stent implantation. Acta Ophthalmologica. 2019;97:e1105–11.
Narita A, Morizane Y, Miyake T, Seguchi J, Baba T, Shiraga F. Characteristics of successful filtering blebs at 1 year after trabeculectomy using swept-source three-dimensional anterior segment optical coherence tomography. Jpn J Ophthalmol. 2017;61:253–9.
Lenzhofer M, Strohmaier C, Hohensinn M, Hitzl W, Sperl P, Gerner M, et al. Longitudinal bleb morphology in anterior segment OCT after minimally invasive transscleral ab interno Glaucoma Gel Microstent implantation. Acta Ophthalmol. 2019;97:e231–7.
Arimura S, Iwasaki K, Orii Y, Takamura Y, Inatani M. Comparison of 5-year outcomes between trabeculectomy combined with phacoemulsification and trabeculectomy followed by phacoemulsification: a retrospective cohort study. BMC Ophthalmol. 2021;21:188.
Broadway D, Grierson I, Hitchings R. Racial differences in the results of glaucoma filtration surgery: are racial differences in the conjunctival cell profile important? Br J Ophthalmol. 1994;78:466–75.
Broadway DC, Chang LP. Trabeculectomy, risk factors for failure and the preoperative state of the conjunctiva. J Glaucoma. 2001;10:237–49.
Wadhwa SD, Higginbotham EJ. Ethnic differences in glaucoma: prevalence, management, and outcome. Curr Opin Ophthalmol. 2005;16:101–6.
Marques RE, Ferreira NP, Sousa DC, Pinto J, Barata A, Sens P, et al. Glaucoma gel implant learning curve in a teaching Tertiary hospital. J Glaucoma. 2019;28:56–60.
Shaarawy T, Grehn F, editors. Guidelines on design and reporting of glaucoma surgical trials. Amsterdam, The Netherlands: Kugler publications; 2009.
Acknowledgements
All authors contributed to the intellectual development of this paper. BCHA conceived and planned the study. BKB, SYL and BCHA wrote the paper. BKB and SYL performed the literature review and data analysis. BKB, SYL, BAL, VCHY and BCHA contributed to the interpretation of the results and provided critical feedback to the paper. The final version of the paper has been seen and approved by all authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
BKB and SYL declare no competing interests. BAL has previously received speaker’s honorarium from Allergan plc. VCHY has previously received funds for travel from Allergan plc. BCHA has previously received funds for travel and research, as well as speaker’s honorarium from Allergan plc.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Betzler, B.K., Lim, S.Y., Lim, B.A. et al. Complications and post-operative interventions in XEN45 gel stent implantation in the treatment of open angle glaucoma—a systematic review and meta-analysis. Eye 37, 1047–1060 (2023). https://doi.org/10.1038/s41433-022-02022-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02022-5