Abstract
Background/Objectives
Aim to identify incidence and prevalence of laser-induced retinal injuries in the Northern Ireland paediatric population and to determine negative clinical and OCT indicators in relation to visual acuity.
Subjects/Methods
A retrospective analysis was conducted of retinal injuries secondary to handheld laser pens over a 6-year time period with presenting and final visual acuity (VA), laser source and circumstances of the injury recorded. Fundus photographs and OCT images for each case were also collated.
Results
Sixty-five patients (74 eyes) were identified of which 72% were male and mean age was 11.6 years. 40% of patients were symptomatic. Mean presenting VA was 0.16 LogMAR. VA was ≤0.30 LogMAR in 20 eyes (27%) at presentation. Features which impacted VA to a significant level were foveolar location, diffuse morphology, ELM and BM/RPE/IDZ disruption and ORH presence on presenting OCT images. ORHs or ELM disruption resulted in a significant risk ratio of 3.5 (p = 0.002) and 3.4 (p = <0.001) respectively. Mean presenting VA was demonstrated to improve during follow-up from 0.36 to 0.22 LogMAR (n = 20, p = 0.03). When VA was ≤0.30 LogMAR at presentation, mean presenting VA improved from 0.56 to 0.29 LogMAR (p < 0.01) with 58% of eyes improving to a VA of better than 0.30 LogMAR.
Conclusions
The overall visual loss from macular laser injuries was low and we have identified features on retinal imaging that significantly impact presenting VA. When VA is affected following macular laser injury there is evidence of recovery with >50% of those presenting with VA ≤ 0.30 LogMAR improving to better than 0.30 LogMAR.
Similar content being viewed by others
Introduction
Published reviews have illustrated an increase in ocular laser injuries from the late 1990s onwards [1]. A further increase in the 2000s coincided with the mass production and ease of access to laser pointers and other forms of handheld lasers [2,3,4]. During this latter period, the ubiquitous use of optical coherence tomography (OCT) imaging in eye care also increased case detection. The most frequently affected population is the paediatric age group and, in particular, males of late childhood/teenage years [3,4,5,6].
Regulation of laser products is based on the potential for risk of injury and, in the UK, this is defined by BS EN 60825-1:2014 and advised by Public Health England [7, 8]. Only lasers powered <1 mW should be available to consumers with lasers of greater power (<5 mW) available for limited activities, i.e. surveying/building alignment [8]. Regulations vary between international regions, e.g. in the USA the sale of 5 mW lasers are permitted [9], and through internet retail, lasers of higher powers can be easily purchased. In addition, the correlation between laser labelling and laser power has been shown to be unreliable [10,11,12].
Identifying cases of retinal macular injury can be challenging as patients may be asymptomatic and present with incidental findings. A history of laser exposure may not be forthcoming from a patient and can either be uncovered reluctantly or sometimes not at all [3, 4, 6, 10, 13, 14]. However, with an increasing number of published cases in the literature, the characteristics of a macular laser injury are becoming established. Macular lesions can appear yellow/pale or pigmented in colour and lesion morphology can be diffuse, focal/multifocal or streak-like [5, 6, 15]. OCT features are also characteristic with outer retinal band disruption, hyperreflective material at the outer retina either in vertical columns or mounds/vitelliform-like lesions, hyporeflective cavities may be present, and early vertical curvilinear hyperreflective bands in Henle’s fibre layer [5, 6, 10, 11, 15]. Another clinical characteristic of macular laser injuries is that both visual function and the lesion can improve over time which is atypical amongst the differential diagnoses [3, 6, 11, 15].
We present a case series of laser injuries identified and collected in a large paediatric ophthalmology department and aim to identify the incidence and prevalence within our population, the presenting level of visual acuity and determine any negative characteristic indicators.
Materials and methods
A retrospective analysis of the Belfast Health and Social Care Trust (BHSCT) secure paediatric ophthalmology database identified all children aged less than 16 years with macular laser burns from 2013 to 2019.
The patient cohort collected is population-based. According to migration statistics, immigration in Northern Ireland (NI) is greater than emigration, making our population ideal for epidemiological studies. The catchment area for the Belfast Regional Paediatric Ophthalmology Centre encompasses a large portion of NI and so our findings will represent a minimum incidence and prevalence of macular laser injuries in NI.
Cases were identified either by a positive reported history of laser exposure with a characteristic lesion or the presence of a characteristic retinal lesion on fundal examination and retinal imaging but no corroborative history of laser exposure. These cases were described as “definite” or “probable” laser injuries, respectively. There was no history of solar retinopathy or sungazing in any case. Characteristics of a macular laser injury include at least the following: a yellow/pale or pigmented lesion and a corresponding defect of outer retinal layers or retinal pigmented epithelium (RPE) on OCT imaging. Other notable features were also collected and analysed.
Presenting VA and symptoms were recorded for each case as well as past ocular history. Additional information was recorded as available, including date of injury and the source of laser device. Retinal imaging was obtained for each case which included fundus photography and OCT. When bilateral injuries presented, each eye was considered separately. VA was recorded in all instances as the logarithm of the minimum angle of resolution (LogMAR) and OCT images were collected from the following machines: Topcon 3D OCT-1 Maestro (Toyko, Japan), Zeiss Cirrus HD-OCT (Jena, Germany), Optovue RTVue OCT (Fremont, California, USA) and Nidek RS-330 Retina Scan Duo (Gamagori, Japan).
Features on fundus photographs were coded according to shape (focal, multifocal, diffuse) and colour (pale or pigmented) and OCT was analysed by lesion location (foveolar: central 0.35 mm, foveal: 1.5–0.35 mm from centre, parafoveal: 2.5–1.5 mm from centre and perifoveal: 5.5–2.5 mm from centre), by retinal bands that were disrupted and by other notable OCT characteristics. The external limiting membrane (ELM) and ellipsoid zone (EZ) were easily identifiable in all OCT images and were coded as separate retinal band disruptions. The Bruch’s membrane (BM), RPE and interdigitation zone (IDZ) could not always be discriminated due to variation in image quality and the presence of hyperreflective material (debris) in this anatomical area. Therefore, a pragmatic decision was made to code disruption of BM/RPE/IDZ as disruption of one anatomical area or retinal band, for the purposes of analysis. Choroidal hypertransmission was also analysed to aid with differentiation of BM/RPE vs. IDZ disruption.
Statistical analysis was performed using MedCalc for Windows, version 15.0 (MedCalc Software, Ostend, Belgium). Change/differences in VA were considered clinically significant if ≥0.2 LogMAR. Statistical significance was a p value ≤0.05.
Full approval was obtained from the BHSCT Standards, Quality and Audit department. Information was managed in accordance with the BHSCT guidance on data protection.
Results
Demographics
Over a 6-year time period (August 2013–December 2019), 74 eyes (65 patients) with retinal lesions in keeping with thermal laser injury were identified. The mean patient age was 11.6 years (median 12.0 years), ranging from 5 to 16 years. A majority (72%) of the patients were male (47 male vs. 18 female) and 55% of the affected eyes were right eyes (41 right vs. 33 left). 8 cases (12%) were bilateral where both maculae had lesions.
Definite vs. probable laser exposure
There were 50 (77%) “definite” cases of macular laser injury involving 56 (76%) eyes. Fifteen (23%) cases of macular laser injury involving 18 (24%) eyes were classified as “probable”. These two groups displayed no statistically significant differences in terms of presenting VA (0.18 vs. 0.08 LogMAR, respectively, p = 0.06), or lesion OCT characteristics.
Incidence and prevalence in Northern Ireland
Population statistics, as mid-year population estimates, were acquired for all persons aged 0 to less than 16 years old from the Northern Ireland Statistics and Research Agency [16]. The minimal incidence and prevalence of macular laser injuries in NI are recorded in Table 1, for the years 2013–2019. Incidence of detected laser injuries is presented per year (per 100 000 population <16 years old) and a running year by year prevalence (per 100,000 population <16 years old) is presented with account taken for those patients who “aged out” of the less than 16-year-old paediatric age limit.
Source of lasers
The laser source, when available, was recorded for each case. A definitive source was identified in 22 cases (34%). Where a definitive source was identified, seventeen cases (77%) of laser injury resulted from lasers bought outside the UK, either while on family holiday or brought back from holiday as a gift/toy for the patient. In comparison, only one case (5%) resulted from a laser confirmed to have been bought within the UK. A further four cases (18%) resulted from lasers bought via international internet retailers.
Of the other 43 cases, 16 (25%) occurred through exposure to a laser owned by someone else (school friends, extended family members, etc.) but the source could not be further confirmed. In 12 cases (18%), a laser source could not be determined but laser exposure was confirmed. Five cases (8%) denied laser exposure and, in ten cases (15%), the history could not be confirmed nor denied as the patient was assessed at a nurse-led imaging clinic.
Visual acuity
Twenty-six patients (40%) described themselves as visually symptomatic at presentation with 7 (11%) experiencing positive scotomas. The presenting visual acuity for all 74 eyes (65 patients) was a mean of 0.16 LogMAR (median 0.10 LogMAR) and ranged from −0.18 to 1.00 LogMAR. We defined “poor vision” as VA of 0.30 or worse with 20 eyes (27%) analysed within this subgroup. In the poor vision subgroup, VA at presentation was a mean of 0.52 LogMAR (median 0.48). Conversely, 54 eyes (73%) had presenting VA better than 0.30 LogMar with a mean of 0.03 LogMAR (median 0.00).
Lesion appearance
Lesions were characterised by macular location on OCT (foveola, fovea, parafovea or perifovea) and by appearance on fundus photograph (pale or pigmented and focal, multifocal or diffuse). A case of a choroidal neovascular membrane (CNVM), secondary to macular laser injury, was excluded from any subsequent analysis as this is a distinct pathology and the exact location of laser burn could not be identified.
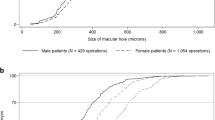
Lesion location
Fifty-two eyes had macular lesions which affected the foveola at its most central point on OCT imaging. When a lesion involved the foveola, presenting VA was a mean of 0.22 LogMAR (Median 0.18, range −0.08 to 1.00 LogMAR). Fifteen eyes had lesions that involved the fovea at their most central point. Presenting VA was a mean of 0.00 LogMAR (Median 0.00 LogMAR, range −0.18 to 0.18). Four eyes had parafoveal lesions at their most central point and a presenting mean VA of −0.01 LogMAR (Median −0.08) and a further two eyes had perifoveal lesions at their most central point with a presenting mean VA of −0.08 LogMAR (Median −0.08 LogMAR). There was a statistically significant difference in presenting VA of foveolar vs. foveal lesions (p value <0.01) and foveolar vs. para/perifovea (p value <0.01) respectively. There was no statistically significant difference between VA at the fovea and more peripheral locations (p value = 0.44), Fig. 1.
Fundal appearance
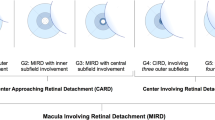
Lesion appearance on fundal photography were described according to the following characteristics: pale or pigmented and focal, multifocal or diffuse in appearance. The frequency of the above characteristics are summarised in Table 2 and illustrated in Fig. 2A.
A Lesion appearance on fundoscopy, described as: (ai) pale, (aii) pigmented, (aiii) focal, (aiv) multifocal, and (av) diffuse. B OCT features of macular laser injuries: (bi) normal outer retinal bands, (bii) outer retinal band defects, (biii) hyperreflective material in outer retina, (biv) vitelliform-like lesion, (bv) curvilinear lines in Henle’s layer (*) and (bvi) outer retinal holes. C OCT B-Scans demonstrating Outer retinal holes (ORHs) of varying size (ci–iii). D Lesions with disruption of the external limiting membrane (ELM), (di) a severe lesion with disruption of inner retinal layers and (dii) a diffuse lesion with hyperreflectivity inner to the ELM, E(ei) A mounded, vitelliform-like area of hyperreflectivity in the acute lesion and (eii) the same lesion 13 months later showing atrophy of the outer retinal bands. F(fi) Outer retinal band defect (EZ band) with mild hyperrelective material and (fii) showing recovery of this lesion at 2 months follow-up.
We analysed only lesions located at the foveola for the impact of lesion morphology on VA (n = 52 eyes) in order to reduce confounding factors as we know that lesion location has a significant impact on visual acuity.
Both clinical and significant differences in mean presenting VA was present between lesions that appeared diffuse on fundal photography and those that were focal (0.46 vs. 0.15 LogMAR, p = 0.01) or multifocal (0.46 vs. 0.15, p < 0.01), respectively. There were no such differences between focal and multifocal lesions (0.15 and 0.15 LogMAR, p = 0.94). There was no significant difference in VA between pale and pigmented groups.
Optical coherence tomography retinal band disruption and other features (foveola cases only)
The frequency of OCT features present in our cohort are summarised in Table 2 and illustrated in Fig. 2B. These include outer retinal band defects, hyperreflective material in outer retina, vitelliform-like lesion, curvilinear lines in Henle’s layer and outer retinal holes.
For the reason stated previously, we analysed only OCT images of foveola lesions (52 eyes/45 patients) looking at disruption of outer retinal bands and the corresponding impact on VA. These findings are summarised in Table 3. The presenting VA was worse in eyes with ELM (0.61 vs. 0.17 LogMAR, p = 0.02), EZ (0.23 vs. 0.05 LogMAR, p value = 0.01) and IDZ/RPE/BM disruption (0.24 vs. 0.02 LogMAR, p value <0.01) at a statistically significant level when compared to eyes in which these OCT bands were intact. ELM and IDZ/RPE/BM band disruption also satisfied our criteria for clinical significance (i.e. a difference of ≥0.2 LogMAR). Choroidal hypertransmission had no significant impact on presenting VA.
We noted a recurring outer retinal feature of hyporeflective spaces extending from the RPE inwards to “touch”, but not disrupt, the ELM. These optically empty spaces where often broad with a “squared” appearance on OCT and throughout this paper we refer to this feature as an “outer retinal hole” (ORH), Fig. 2C. When an ORH was identified, presenting VA was significantly worse (statistically and clinically) than when an ORH was not present and the ELM was intact, 0.36 vs. 0.03 LogMAR, respectively (p value <0.01).
OCT analysis of eyes with good vs. poor VA (foveola cases only)
OCT findings were analysed for 33 eyes with presenting VA better than 0.30 LogMAR and 19 eyes from the worse than or equal to 0.30 LogMAR group and are summarised in Table 3. Lesions in which the ELM was disrupted (Fig. 2D) or where an ORH was present (but the ELM remained intact) had an increased risk of VA being ≤0.30 LogMAR relative to all other cases, i.e. risk ratio (RR) of 3.4 (p value = <0.001) and of 3.5 (p value = 0.002), respectively. The RR associated with EZ or IDZ/RPE/BM disruption did not meet statistical significance.
Complications
Complications secondary to macular laser injury were present in two eyes (3%). There was one case of a full-thickness macular hole and one case of sub-foveal choroidal neovascular membrane. Both complications were present at presentation.
Follow-up data
Forty-nine patients (54 eyes) were seen in hospital outpatient clinic on one occasion only, which included 46 patients (51 eyes) who were discharged to community optometry and three patients (three eyes) who did not attend a planned review appointment.
Sixteen patients (20 eyes) were reviewed for at least one further hospital outpatient appointment with follow-up data on VA available. Within this group, mean presenting VA was 0.36 LogMAR (median 0.35, range −0.08 to 1.00 LogMAR) and final recorded mean VA was 0.22 LogMAR (median 0.18, range −0.08 to 0.40 LogMAR). The improvement in VA was statistically significant, p value = 0.03. Follow-up ranged from 0.5 to 13 months. When separating cases into ≤3 month, 6 (±3) months and 12 (±3) months follow-up groups, VA improvement was not greater with an increased follow-up period (i.e. 0.27 (n = 5), 0.09 (n = 6) and 0.09 (n = 5) LogMAR improvement respectively).
Twelve patients (12 eyes) in the “poor vision” group were followed up over a range of 0.5–13 months. The mean presenting VA was 0.56 LogMAR (median 0.55, range 0.30–1.00) and mean final recorded VA was 0.29 LogMAR (median 0.19, range −0.08 to 0.70). This demonstrated a clinically and statistically significant (p < 0.01) improvement. Of these 12 eyes, 7 (58%) improved to a level of better than 0.30 LogMAR. Notable features in the 5 (42%) eyes which did not improve were diffuse lesions (4 of 5, 80%) and ORHs (5 of 5, 100%).
Fundal photography/OCT imaging follow-up data
Serial retinal photographs were collected for six eyes/cases and serial OCT imaging was collected in eight eyes/cases over a mean follow-up period of 9.3 and 8.5 months, respectively.
Of the six eyes with retinal photographs, changes in lesion morphology were noted in three eyes/cases (50%). Acute or earlier lesions had a less distinct border and were pale while on later images these lesions developed a more distinct border with increased pigmentation at the centre of the lesion.
OCT images remained stable in 4 eyes (50%) at 12-, 11-, 10- and 10 months follow-up, respectively. A raised hyperreflective lesion, “vitelliform-like” in shape, was present in two eyes which resolved over time to leave a flat atrophic lesion (VA 0.48 to −0.08 LogMAR at 14 days, and VA 1.0 to 0.34 LogMAR at 13 months, Fig. 2E). A further lesion initially had outer retinal hyperreflective material which resolved leaving an ORH; this case also had a subtle curvilinear line in Henle’s layer present on initial OCT which later resolved (VA 0.4 to 0.18 LogMAR at 10 months). In the remaining eye which demonstrated change on OCT, there was recovery of the EZ retinal band which was disrupted on initial OCT (hyperreflective material was also present at this site, Fig. 2D) but appeared to recover at 2 months with concomitant recovery of VA (0.30 to 0.10 LogMAR). All four of the cases had acute, symptomatic presentations and were presumed to demonstrate temporal changes of lesions presenting soon after the initial injury.
Discussion
We believe this to be the largest case series of macular injuries secondary to lasers and the only series to provide population-based data on incidence and prevalence within a paediatric population.
In our cohort of children (<16 years old), 65 patients (74 eyes) with a macular lesion were identified over a 6-year time period with a mean age of 11.6 years and a majority of male patients (72%) and unilateral injuries (88%). Over the most recent 3 years, the data has stabilised with an approximate prevalence of 10–12 paediatric cases of macular laser injury per 100,000 population.
Where a source was identifiable, lasers purchased outside the UK were the most common source of lasers (77%) followed by those purchased via international internet retailers (18%). Lasers bought online or on holiday may be of greater output power than permitted by UK regulations; however, caution is required when determining laser risk based on output power as there is worrying evidence that the labelled power of handheld lasers may also be inaccurate with the true power considerably greater [10,11,12].
Seventy-eight percent of patients had “definite” laser injuries and 22% had “probable” laser injuries. For a variety of reasons, as described by other authors, there can be a reluctance to admit to laser exposure or it may have occurred a long time previously and not be remembered by the patient. Additionally, clinicians may have a low suspicion for such an aetiology [3, 4, 6, 10, 13, 14].
It is, therefore, useful to establish characteristic features of a macular laser injury to alert suspicion of this aetiology. The classical features of macular laser injury include a lesion which is pale in appearance (yellow, green or grey), well demarcated with variable degrees of pigmentation (reviewed by Neffendorf et al., Birtel et al. and Linton et al.) [4, 11, 13]. Disruption of outer retinal bands is an essential finding on OCT imaging as reported widely in cases reports and series [4, 11, 13]. All retinal bands remained intact in only one eye in our cohort, although the EZ showed irregular hyperreflectivity at the site of the lesion (pale lesion with choroidal hypertransmission on OCT) possibly indicating recovery of outer retinal bands in this area.
Additional features, although not always present, have been described. With an acute lesion, there is often a hyperreflective material present in the outer retina/RPE and there may even be a vitelliform-like morphology to the lesion [2, 5, 6, 14]. An OCT feature that is present even earlier are vertical curvilinear lines in Henle’s layer spanning from RPE to the outer nuclear layer [2, 10, 17,18,19] but these resolve quickly, within weeks [10]. Curvilinear lines were visible in the presenting OCT of 3 eyes only in our cohort. This is not surprising as this feature resolves quickly and many of our cases were asymptomatic (60%) and referred with incidental findings.
Hyporeflective spaces are less frequently reported [2, 10, 17, 19]. In our cohort, we described ORHs as hyporeflective spaces within the outer retinal bands extending from the RPE inwards to the ELM, but with the ELM intact, Fig. 2C. These cavities are often broad with a “squared” appearance on OCT and resemble an OCT feature described with solar retinopathy in which there is similar loss of outer retinal tissue. Earlier reports on solar retinopathy injury termed these lesions “RPE excavations”, likely due to the limited image resolution of time domain OCT imaging [20]. Later reports with the benefit of spectral domain of OCT described an “Outer Retinal Hole” as a rectangular lesion spanning inner border of RPE line to the ELM [21]. Due to the similar appearance and likely similar patho-aetiology we have elected to term these lesions in our cohort as ORHs. Similar lesions can be visualised in published literature of macular laser injuries and may appear as a chronologically later feature [2, 22]. In our cohort, three eyes with ORH had serial OCT images available with a more discrete ORH present in the later images. We believe that the presence of ORHs have not previously been analysed as a factor in relation to VA. Their negative impact on vision may relate to a greater volume of tissue loss than other injuries and so limit potential for recovery.
Overall presenting VA in our patients was 0.16 LogMAR (median 0.10). Presenting VA was worse than or equal to 0.30 LogMAR in 20 eyes (27%). This contrasts with the findings in a systematic review by Birtel et al. in which 55% of published cases had presenting VA worse than 0.30 LogMAR [11]. It may be that more serious cases are presented in published literature with milder cases going undetected (only 40% of our patients were symptomatic) or not considered for publication (publication bias). As our cohort is population-based, it is a truer reflection of the overall impact of lasers on vision in childhood.
We found that the significant factors which negatively affect presenting VA were lesions involving the foveola (i.e. central 0.35 mm), a diffuse lesion and the presence of ELM disruption or an ORH. The latter two features resulted in a significant increase in RR of VA being ≤0.30 LogMAR that is clinically useful.
Follow-up data was available for 20 eyes and displayed mean VA improvement that was statistically significant. Twelve of these eyes with VA worse than 0.30 LogMAR improved from a mean of 0.56 to of 0.29 LogMAR. Seven (58%) of these 12 eyes improved to a level of better than 6/12 demonstrating the potential for considerable VA improvement when presenting VA is “poor”. Of the five eyes (42%) where VA did not improve to better than 6/12, at least one of the significant OCT features, previously described, were present in all, i.e. foveolar-involving (100%), diffuse lesion (60%) and ELM disruption or ORH (100%).
These findings on visual acuity have been very useful to us clinically when counselling our patients and a patient/parent information leaflet has been developed based on this information (available as Supplementary file).
Limitations that we experienced during this study were the retrospective nature of data collection, specifically this limited data on laser source and impacted follow-up duration and final VA. As a result, we were unable to identify clinical features relating to final VA. Acquisition of retinal imaging from numerous OCT machines involved pragmatic decisions on analysis of B-Scans. We have also made the assumption that presenting VA values correlated with the macular lesion present, as there was no available baseline or pre-lesion VA for these cases. However, the degree of visual recovery in many patients implies that reduced VA was due to the macular lesion. Furthermore, there is excellent uptake of the regional Primary 1 School Vision Screening Programme in NI and none of our patients had been referred to community or hospital eye services due to failed vision screening. Finally, we acknowledge that our statistics will represent a minimum incidence and prevalence of macular laser injuries in NI due to a retrospective data collection and the possibility that milder cases would not be referred to the Belfast Regional Paediatric Ophthalmology Centre by optometrists. We would recommend that an epidemiological study, through an organisation such as the British Ophthalmological Surveillance Unit, would be useful to aid robust follow-up and help inform UK wide incidence and prevalence.
Conclusion
We identified a cohort of patients over a 6-year period with macular laser injuries and provide population-based data on incidence and prevalence of these injuries.
The overall visual impact appeared to be low but there was a subgroup of patients with visual acuity worse than or equal to 0.30 LogMAR. We also found an overall improvement in VA during follow-up. When presenting VA was poor, we demonstrated a potential for visual recovery with almost 58% improving to better than 0.30 LogMAR.
Negatively lesion characteristics relating to worse VA were identified including lesions involving the foveola, diffuse lesions and the presence of ORHs or ELM disruption on OCT imaging.
There is strong evidence that further public health messaging on the dangers of ‘’toy lasers” is required: consideration should be given to undertaking targeted education of children within primary and secondary schools.
Summary
What was known before
-
Increasing prevalence over ~20 years involving mainly patients who are male from the paediatric age population.
-
Harmful lasers are often purchased online or while abroad and the laser power can be mislabelled.
-
OCT imaging is increasingly used to identify and characterise these lesions
-
There is a low rate of complications from macular laser injuries.
What this study adds
-
We present population data on incidence and prevalence of macular handheld laser injuries.
-
We demonstrate, on average, a low impact on visual acuity and the potential for visual recovery in those with reduced vision.
-
We also add to the OCT imaging characterisation of macular laser injuries identifying outer retinal holes and present risk ratios of visual acuity being ≤0.30 LogMAR with specified OCT features.
References
Barkana Y, Belkin M. Laser eye injuries. Surv Ophthalmol. 2000;44:459–78.
Lee GD, Baumal CR, Lally D, Pitcher JD, Vander J, Duker JS. Retinal injury after inadvertent handheld laser exposure. Retina. 2014;34:2388–96.
Torp-Pedersen T, Welinder L, Justesen B, Christensen UC, Solborg Bjerrum S, La Cour M, et al. Laser pointer maculopathy—on the rise? Acta Ophthalmol. 2018;96:749–54.
Neffendorf JE, Hildebrand GD, Downes SM. Handheld laser devices and laser-induced retinopathy (LIR) in children: an overview of the literature. Eye. 2019;33:1203–14.
Raoof N, Bradley P, Theodorou M, Moore AT, Michaelides M. The new pretender: a large UK case series of retinal injuries in children secondary to handheld lasers. Am J Ophthalmol. 2016;171:88–94.
Zhang L, Zheng A, Nie H, Bhavsar KV, Xu Y, Sliney DH, et al. Laser-induced photic injury phenocopies macular dystrophy. Ophthalmic Genet. 2016;37:59–67.
BS EN 60825-1:2014—Safety of laser products. Equipment classification and requirements [Internet]. 2020. https://shop.bsigroup.com/en/ProductDetail/?pid=000000000030364399.
Laser radiation: safety advice—GOV.UK [Internet]. 2020. https://www.gov.uk/government/publications/laser-radiation-safety-advice/laser-radiation-safety-advice#laser-pointers-currently-available-on-the-market.
Laser Products and Instruments|FDA [Internet]. 2020. https://www.fda.gov/radiation-emitting-products/home-business-and-entertainment-products/laser-products-and-instruments.
Dhrami-Gavazi E, Lee W, Balaratnasingam C, Kayserman L, Yannuzzi LA, Freund KB. Multimodal imaging documentation of rapid evolution of retinal changes in handheld laser-induced maculopathy. Int J Retin Vitr. 2015;1:1–7.
Birtel J, Harmening WM, Krohne TU, Holz FG, Issa PC, Herrmann P. Retinal injury following laser pointer exposure—a systematic review and case series. Dtsch Arztebl Int. 2017;114:831–7.
Hadler J, Tobares E, Dowell M. Random testing reveals excessive power in commercial laser pointers. J Laser Appl. 2013;25:032007.
Linton E, Walkden A, Steeples LR, Bhargava A, Williams C, Bailey C, et al. Retinal burns from laser pointers: a risk in children with behavioural problems. Eye. 2019;33:492–504.
Xu K, Chin EK, Quiram PA, Davies JB, Wilkin Parke D, Almeida DRP. Retinal injury secondary to laser pointers in pediatric patients. Pediatrics. 2016;138:9–16.
Bhavsar KV, Wilson D, Margolis R, Judson P, Barbazetto I, Bailey Freund K, et al. Multimodal imaging in handheld laser-induced maculopathy. Am J Ophthalmol. 2015;159:227–.e2.
Mid Year Population Estimates|Northern Ireland Statistics and Research Agency [Internet]. 2020. https://www.nisra.gov.uk/statistics/population/mid-year-population-estimates.
Raoof N, O’Hagan J, Pawlowska N, Quhill F. “Toy” laser macular burns in children: 12-month update. Eye. 2016;30:492–6.
Lally DR, Duker JS. Foveal injury from a red laser pointer. JAMA Ophthalmol. 2014;132:297.
Rusu I, Sherman J, Gallego-Pinazo R, Lam M, Freund KB. Spectral-domain optical coherence tomography and fundus autofluorescence findings in a case of laser pointer-induced maculopathy. Retin Cases Br Rep. 2013;7:371–5.
Chen JC, Lee LR. Solar retinopathy and associated optical coherence tomography findings. Clin Exp Optom. 2004;87:390–3.
Comander J, Gardiner M, Loewenstein J. High-resolution optical coherence tomography findings in solar maculopathy and the differential diagnosis of outer retinal holes. Am J Ophthalmol. 2011;152:413–.e6.
Weng CY, Baumal CR, Albini TA, Berrocal AM. Self-induced laser maculopathy in an adolescent boy utilizing a mirror. Ophthalmic Surg Lasers Imaging Retin. 2015;46:485–8.
Author information
Authors and Affiliations
Contributions
GR was responsible for designing the study, collecting data, analysing and interpreting results, writing the report, creating and tables and figures. EM was responsible for designing study, collecting data, analysing and interpreting results, reviewing report. KS responsible for collecting data, reviewing report. RG was responsible for collecting data, reviewing report. SG was responsible for collecting data, reviewing report. MO was responsible for collecting data, reviewing report. JK was responsible for collecting data, reviewing report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Reid, G., Shirley, K., Gamble, R. et al. Macular injuries secondary to handheld lasers in a paediatric population—clinical characteristics and indicators of visual impact. Eye 37, 176–182 (2023). https://doi.org/10.1038/s41433-021-01916-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01916-0