Abstract
Objectives
To describe the features, management approaches, and outcomes of orbito-cranial schwannomas.
Methods
Retrospective review of ten patients with orbito-cranial schwannomas managed in six orbital services over 22 years. Data collected included demographics, presenting features, neuroimaging characteristics, histology, management approach, complications, and outcomes.
Results
Mean age of the patients was 41.4 ± 19.9 years, and 6 (60%) were females. The majority presented with proptosis (90%), limited extraocular motility (80%), eyelid swelling (60%), and optic neuropathy (60%). Most lesions (80%) involved the entire anterior-posterior span of the orbit, with both intra- and extraconal involvement. All tumours involved the orbital apex, the superior orbital fissure, and extended at least to the cavernous sinus. Surgical resection was performed for all. Seven (70%) of the tumours were completely or subtotally resected combining an intracapsular approach by an orbital-neurosurgical collaboration, with no recurrence on postoperative follow-up (6–186 months). Three underwent tumour debulking. Of these, two remained stable on follow-up (6–34 months) and one showed progression of the residual tumour over 9 years (cellular schwannoma on histology) necessitating stereotactic radiotherapy (SRT) for local control. Adjuncts to the orbito-cranial resection included perioperative frozen section (n = 5), endoscopic transorbital approach (n = 2), and image-guided navigation (n = 1). Post-surgical adjuvant SRT was used in three subjects.
Conclusions
These results highlight the possibility of successful surgical control in complex orbito-cranial schwannomas. A combined neurosurgical/orbital approach with consideration of an intracapsular resection is recommended. Recurrence may not occur with subtotal excision and observation may be reasonable. Adjunctive SRT for progression or residual tumour can be considered.
Similar content being viewed by others
Introduction
Schwannomas uncommonly occur in the orbits and account for 1–2% of all orbital tumours [1,2,3]. The typical primary orbital schwannoma is localised and well-circumscribed [3, 4], however an orbito-cranial presentation has been documented [5]. In these cases extracapsular total resection, which is the mainstay therapy for localised lesions, is challenging and risks significant morbidity [5, 6].
There is little information regarding the management approach for orbito-cranial schwannomas. Furthermore, the outcome in the context of incomplete surgical excision is not well established. The current multicentre case-series presents the clinical and diagnostic imaging features, surgical and adjuvant management approaches, and outcomes in ten patients with orbito-cranial schwannomas.
Methods
Data were collected retrospectively from consecutive adult patients with orbito-cranial schwannomas attending one of six orbital centres, between August 1998 and April 2020. This study received Institutional Review Board approval and adhered to the tenets of the Declaration of Helsinki.
Included patients were adults (>18 years) with histologically proven orbito-cranial schwannoma. Junctional lesions (e.g. apical lesions abutting the superior orbital fissure but not extending into the cavernous sinus [SOF]) were not included in this series. Data collected included patient demographics, presenting symptoms and signs, duration of symptoms, neuroimaging type (MRI, CT), neuroimaging characteristics of tumour, histology, management course (including surgical approach and radiation therapy), treatment related complications, length of follow up, and clinical status at the last follow up.
Results
Demographic and clinical features
The mean age of the patients was 41.4 ± 19.9 years (median 32, range 19–76 years), and 6 (60%) were females (Supplementary Table 1). All patients had unilateral involvement, of which 7 (70%) were right sided. The most common clinical signs on presentation were proptosis (90%), limited extraocular motility (80%), and eyelid swelling (60%, Supplementary Table 1). Six (60%) patients had signs of optic neuropathy with reduced VA ranging from 20/30 (n = 3), through 20/70 (n = 1), to no perception of light (n = 2). Commonly reported symptoms included blurring of vision (60%), headache (50%), orbital pain (50%), and diplopia (50%). The reported insidious onset of symptoms was a mean of 44.3 ± 66.1 months (median 12, range 2.5–180 months). One subject (#2, Supplementary Table 1) had familial schwannomatosis. An intradural T12/L1 schwannoma was surgically resected 6 years after surgery for the orbito-cranial tumour.
Tumour characteristics
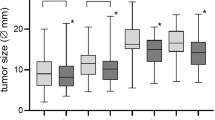
The orbital location of the tumour was mainly superior in 5 (50%) of subjects, involving all orbital quadrants in 40%, and mainly inferior in one (Table 1).
The mean size of the tumours (maximal length) was 53.4 ± 1.73 mm (median 58.5, range 26–80 mm). Most lesions (80%) involved the entire anterior-posterior span of the orbit, with both intra- and extraconal involvement (Table 1).
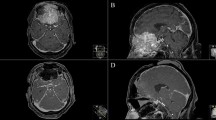
All tumours extended at least to the cavernous sinus (CS) by SOF expansion (Fig. 1). Four lesions extended beyond the CS to involve Meckel’s cave and/or the middle cranial fossa. Two of these additionally extended to the anterior cranial fossa and the paranasal sinuses/nasal cavity via orbital roof and medial wall bone destruction, respectively (Figs. 2 and 3).
Because of the extent of the tumours, the nerve of origin was not readily identifiable, likely involving more than one branch at the time of orbito-cranial presentation.
MRI imaging with and without contrast was available for 8/10 subjects, in three of which CT was also conducted. In two subjects only CT was performed. On MRI all tumours were T1 isointense. Six (out of 8) were T2 hyperintense, and two showed heterogenous T2 intensity. All displayed marked enhancement that proved to be early and rapid on dynamic contrast imaging (available for two subjects, Fig. 1). Most of the tumours (8/10) were well-circumscribed, while 2 were diffuse (Figs. 2 and 3). Only three had a homogenous appearance, the majority (70%) appearing heterogeneous. Three lesions were multi-lobular with degenerative/multi-cystic changes (Fig. 4).
Management and outcomes
Histological diagnosis proved low-grade schwannomas in all but one subject (#5). This patient underwent initial surgery for orbital tumour debulking due to ongoing pain, in which low-grade schwannoma was shown on histology. Over the next six years, the orbital and intracranial involvement significantly progressed along with increasing pain and discomfort (Fig. 2), prompting a joint orbital-neurosurgical resection. At that stage the histological features suggested a cellular schwannoma with 10% MIB-1 positive cells [7].
In eight (80%) of the subjects, surgery entailed a joint orbital and neurosurgical collaboration (Table 1). In one subject an ENT collaboration was additionally needed for the resection of ethmoidal/nasal cavity extension (subject #4, Fig. 3). The orbital approach was in most cases a lateral orbitotomy or superolateral orbitotomy, with (n = 3) or without a bone flap. In three subjects an eyelid sparing exenteration was performed. The neurosurgical craniotomy approaches included orbitofrontal, orbitozygomatic, frontotemporal, and pterional with (n = 1) or without (n = 3) image guidance. In two subjects an endoscopic transorbital approach was utilised for the intracranial resection. Perioperative frozen section control was used in five (50%) of the cases. In five subjects the tumour resection was intracapsular, in four subjects extracapsular, and in one subject the orbital resection was extracapsular while the intracranial resection was intracapsular. In three subjects adjuvant fractioned stereotactic radiotherapy (SRT) was employed, with accumulative doses of 45 Gy (n = 1) and 54 Gy (n = 2).
Two of the patients underwent complete resection of the tumour, confirmed by frozen section and lack of residual disease on subsequent MRI (Supplementary Fig. 1), with no recurrence at 36 months and 49 months of postoperative follow up, respectively.
Five subjects had subtotal resection (with neurosurgical collaboration) with minimal residual disease, and with no recurrence on postoperative follow up (at 6, 8, 12, 108, and 186 months, respectively). Two patients had only the orbital component resected by orbital surgeons (i.e. tumour debulking) with evidence of residual tumour. There was no postoperative tumour progression at 6 months and 34 months, respectively. Another patient that underwent (neuro-orbital) debulking (subject #5, Fig. 2) had slow progression of a residual CS tumour over 9 years of postoperative follow-up, for which she recently (4 months) had SRT (20 Gy) treatment. The mean post-surgical follow-up was 56.5 ± 61.3 months (median 35, range 6–186 months).
There were no reported intraoperative complications. The postoperative visual acuity did not change compared to baseline in seven (70%) of the subjects, improved by two lines in one subject, and by one line in another (Table 1). In subject #5 an exenteration was performed despite preserved visual acuity, due to the abovementioned considerations. Other postoperative sequelae are detailed in Table 1.
Discussion
It is recognised in the neurosurgical literature that trigeminal schwannomas epicentered intracranially, and particularly the CS, may infrequently invade the orbit. Categorisations of such presentation included “dumbbell-shaped tumour in the middle fossa and the extracranial orbital space” (ME1) [8], type D extracranial extension [9,10,11], or referred to as “(cavernous) peripheral subtype” [12, 13]. Nonetheless, this series is the first to focus on the management of schwannomas epicentered in the orbit with an intracranial extension. These cases presented to the orbital service due to predominant orbital involvement and significant ophthalmic manifestations, such as compressive optic neuropathy, proptosis, and limitation of extraocular movement. Because of the rarity of this presentation, the orbital surgeon may have very little experience in the management of extensive orbito-cranial tumours. Thus, being aware of the management approaches and experience collated herein from six orbital centres may benefit the orbital surgeon encountering such complex schwannomas.
The ophthalmic literature is mostly dedicated to primary orbital schwannoma. It is typically a localised, well-circumscribed, noninvasive, encapsulated tumour that can be completely or near-completely excised, and rarely recur [1, 3,4,5, 14]. There were, however, previous orbital schwannoma series reporting that tumours extended to the SOF in up to a quarter to one-third of cases [1, 5, 15, 16]. The course of extension corresponds to the most common orbital origin from the ophthalmic branch of the trigeminal nerve [1, 5]. Nevertheless, many of these represent junctional tumours (without intracranial involvement), thus some can be resected using a traditional extraperiosteal approach via lateral or superolateral orbitotomy [17].
The current series represents orbito-cranial schwannomas with relatively extensive orbital involvement. Most lesions (80%) occupied the entire anterior-posterior span of the orbit, with both intra- and extraconal involvement. All tumours involved the orbital apex, the SOF, and extended at least to the CS intracranially (4 involved Meckel’s cave and/or middle cranial fossa). Despite this, in 70% of cases complete or subtotal resection was achieved, with significant debulking in the rest. There were no intraoperative complications (e.g. CSF leak). Postoperative sequalae were sensory (paraesthesia), motor (ophthalmoplegia/diplopia), or autonomic (mydriasis) deficits, in some cases with subsequent improvement. These were reported even following excision of localised orbital schwannomas [1, 5, 18], however are expected to be more common following SOF and CS surgical manipulation. All cases but one remained stable in up to 6–186 months, including those with residual tumours. Although in some subjects longer follow up is warranted in order to establish stability, these results highlight the possibility of successful surgical control in complex orbito-cranial schwannomas.
Infrequent occurrences of orbital schwannomas that were unable to be completely removed due to orbital apex involvement, SOF and/or CS extension have been reported. Cantore et al. [16] described one case (out of 9 orbital schwannomas) that extended beyond the SOF to involve the “skull”. It was managed by intracapsular debulking using an ultrasonic aspirator. Rose et al. [1] described 6/25 orbital schwannomas that extended to the SOF, limiting complete resection. Neurosurgical collaboration was not mentioned. Nevertheless, even with incomplete resection, there has been no evidence of progression in up to 23 years of follow-up. They proposed that surgical debulking alters the growth pattern by removal of tumour growth factors [1].
In a recent series by Yong et al. [5], 3/18 orbital schwannomas involved the orbital apex, one case involved the SOF, and four extended to the CS. In total, only one of these cases, a tumour that involved the orbital apex, was completely excised (via superolateral orbitotomy). Of the four cases with CS involvement, two underwent initial debulking of the orbital portion of the tumour, requiring neurosurgical intervention (via pteronial craniotomy) a few years later due to progression. One other case was debulked via lateral orbitotomy, and the last case underwent SRT without surgical management. Subsequently, all of them showed stable tumours in 3 to 19 years of follow-up [5]. Nevertheless, based on their experience the authors suggested that a larger residual tumour bulk has a higher risk of recurrence, thus surgery should aim for the maximum possible removal [5]. The neurosurgical literature supports this notion, as incomplete resections of intracranial trigeminal schwannomas are associated with a greater recurrence rate [19, 20].
In this series, complete or subtotal, intracapsular excision was attained in three cases via lateral or superior orbitotomy combined with pteronial craniotomy. Image-guided navigation was used in one (of the three). In a fourth case subtotal resection was achieved via an extracapsular exenteration combined with an ethmoidal (ENT) and a pteronial intracapsular excision. A pteronial approach was previously advocated in a case of orbital schwannoma involving the SOF and CS, enabling complete surgical removal [13]. In another of our cases an orbitofrontal craniotomy was performed enabling subtotal intracapsular resection. This approach was previously utilised in a case of orbital oculomotor nerve schwannoma extending to the CS, enabling complete intracapsular removal [21]. Two additional cases underwent a lateral orbitotomy (with bone window) combined with an endoscopic transorbital (intracapsular) approach, achieving complete or subtotal removal, respectively. This is a recent advance in endoscopic skull base surgery, allowing access to the lateral orbit, apex of the orbit, anterior cranial fossa, and middle cranial fossa. It was shown to achieve successful resection of tumours, including trigeminal schwanommas, while minimising significant morbidities such as CSF leaks or ophthalmic complications [22, 23].
Noteworthy, SRT was employed in three of our subjects as adjuvant post-surgical treatment, and in a fourth subject for local control of a progressing CS residual tumour. Radiosurgery is an established treatment of intracranial trigeminal schwannomas with reported local control rates as high as 91–100% [6]. SRT offers the biological advantages of dose fractionation. It was reported as a sole treatment modality, after subtotal resection, and after recurrence following initial surgical resection, and similarly has shown local control rates of 95–100% [6, 24, 25]. It was advocated as an adjunct to surgical resection in symptomatic high-risk cases, including large tumours, recurrences, and CS involvement, as well as for enhancement of progression-free survival in cases of subtotal excision [6]. SRT (gamma knife) as sole treatment has been reported to be effective in two cases of solitary, well-circumscribed orbital apex schwannomas [26]. Yong et al. [5] reported the use of SRT in an orbito-cranial schwannoma deemed not amenable for surgical resection. The current experience supports the possible benefit of adjuvant SRT in surgically resected orbito-cranial schwannomas. However, further studies are warranted in order to establish its role.
In conclusion, based on the multicentre experience in the management of orbito-cranial schwannomas, the orbital surgeon can consider these approaches when encountering these rare presentations. Firstly, an orbital-neurosurgical collaborative approach, increases the feasibility of complete or subtotal tumour removal. An intracapsular resection may decrease the risk of collateral damage and should be strongly considered, particularly for the intracranial component. Perioperative frozen section control and image-guided navigation may aid in some cases. In schwannomas with extensive orbital involvement, orbital exenteration may be warranted. Finally, post-excision adjuvant SRT can be considered, as well as for local control of residual tumour progression.
Summary
What was known before
-
Schwannomas of the orbit usually present as localised and well-circumscribed tumours approachable to surgical resection.
-
Schwannomas that occupy the deep orbital apex, and particularly cases of intracranial extension, represent a surgical challenge.
What this study adds
-
This is the first series dedicated to describe the presentation, characteristics, management, and outcomes of orbito-cranial schwannomas.
-
An orbital-neurosurgical collaborative approach, increases the feasibility of complete or subtotal tumour removal.
-
Post-excision adjuvant radiotherapy can be considered.
References
Rose GE, Wright JE. Isolated peripheral nerve sheath tumours of the orbit. Eye 1991;5:668–73.
Pushker N, Khurana S, Kashyap S, Sen S, Shrey D, Meel R, et al. Orbital schwannoma: a clinicopathologic study. Int Ophthalmol. 2015;35:481–6.
Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions. Ophthalmol [Internet]. 2004;111:997–1008. https://linkinghub.elsevier.com/retrieve/pii/S0161642003014957
Rootman J, Goldberg C, Robertson W. Primary orbital schwannomas. Br J Ophthalmol [Internet]. 1982;66:194–204. https://bjo.bmj.com/lookup/doi/10.1136/bjo.66.3.194
Yong K-L, Beckman TJ, Cranstoun M, Sullivan TJ. Orbital Schwannoma-Management and Clinical Outcomes. Ophthal Plast Reconstr Surg [Internet]. 2020;36:590–5. http://www.ncbi.nlm.nih.gov/pubmed/32282644
Hamm KD, Gross MW, Fahrig A, Surber G, Henzel M, Kleinert G, et al. Stereotactic radiotherapy for the treatment of nonacoustic schwannomas. Neurosurg [Internet]. 2008;62:A29–36. https://academic.oup.com/neurosurgery/article/62/suppl_5/A29/2558352
Abe M, Kawase T, Urano M, Mizoguchi Y, Kuroda M, Kasahara M, et al. Analyses of proliferative potential in schwannomas. Brain Tumor Pathol [Internet]. 2000;17:35–40. http://link.springer.com/10.1007/BF02478916
Yoshida K, Kawase T. Trigeminal neurinomas extending into multiple fossae: surgical methods and review of the literature. J Neurosurg [Internet] 1999;91:202–11. https://thejns.org/view/journals/j-neurosurg/91/2/article-p202.xml
Samii M, Migliori MM, Tatagiba M, Babu R. Surgical treatment of trigeminal schwannomas. J Neurosurg [Internet]. 1995;82:711–8. https://thejns.org/view/journals/j-neurosurg/82/5/article-p711.xml
Jefferson G. The Trigeminal Neurinomas with Some Remarks on Malignant Invasion of the Gasserian Ganglion. Neurosurg [Internet]. 1955;1:11–54. http://academic.oup.com/neurosurgery/article/1/CN_suppl_1/11/4100295
Zhang L, Yang Y, Xu S, Wang J, Liu Y, Zhu S. Trigeminal schwannomas: a report of 42 cases and review of the relevant surgical approaches. Clin Neurol Neurosurg [Internet]. 2009;111:261–9. https://linkinghub.elsevier.com/retrieve/pii/S0303846708003831
Wanibuchi M, Fukushima T, Zomordi AR, Nonaka Y, Friedman AH. Trigeminal Schwannomas: Skull Base Approaches and Operative Results in 105 Patients. Oper Neurosurg [Internet]. 2012;70:ons132–44. https://academic.oup.com/ons/article/70/suppl_1/ons132/2408529
Schick U, Bleyen J, Hassler W. Treatment of orbital schwannomas and neurofibromas. Br J Neurosurg [Internet]. 2003;17:541–5. http://www.tandfonline.com/doi/full/10.1080/02688690310001627786
Kron M, Bohnsack BL, Archer SM, McHugh JB, Kahana A. Recurrent orbital schwannomas: clinical course and histopathologic correlation. BMC Ophthalmol [Internet]. 2012;12:44. http://bmcophthalmol.biomedcentral.com/articles/10.1186/1471-2415-12-44
Dervin JE, Beaconsfield M, Wright JE, Moseley IF. CT findings in orbital tumours of nerve sheath origin. Clin Radio [Internet]. 1989;40:475–9. https://linkinghub.elsevier.com/retrieve/pii/S0009926089802508
Cantore G, Ciappetta P, Raco A, Lunardi P. Orbital Schwannomas: Report of Nine Cases and Review of the Literature. Neurosurg [Internet]. 1986;19:583–8. https://academic.oup.com/neurosurgery/article/19/4/583/2745519
Shields JA, Kapustiak J, Arbizo V, Augsburger JJ, Schnitzer RE. Orbital Neurilemoma With Extension Through the Superior Orbital Fissure. Arch Ophthalmol [Internet]. 1986;104:871–3. http://archopht.jamanetwork.com/article.aspx?articleid=636090
Chen MH, Yan JH. Imaging characteristics and surgical management of orbital neurilemmomas. Int J Ophthalmol [Internet]. 2019;12:1108–15. http://www.ijo.cn/gjyken/ch/reader/view_abstract.aspx?file_no=20190709&flag=1
Al-Mefty O, Ayoubi S, Gaber E. Trigeminal schwannomas: removal of dumbbell-shaped tumors through the expanded Meckel cave and outcomes of cranial nerve function. J Neurosurg [Internet]. 2002;96:453–63. https://thejns.org/view/journals/j-neurosurg/96/3/article-p453.xml
Konovalov AN, Spallone A, Mukhamedjanov DJ, Tcherekajev VA, Makhmudov UB. Trigeminal neurinomas a series of 111 surgical cases from a single institution. Acta Neurochir (Wien) [Internet]. 1996;138:1027–35. http://link.springer.com/10.1007/BF01412304
Kauser H, Rashid O, Anwar W, Khan S. Orbital oculomotor nerve schwannoma extending to the cavernous sinus: a rare cause of proptosis. J Ophthalmic Vis Res [Internet]. 2014;9:514. http://www.jovr.org/text.asp?2014/9/4/514/150833
Park HH, Hong SD, Kim YH, Hong C-K, Woo KI, Yun I-S, et al. Endoscopic transorbital and endonasal approach for trigeminal schwannomas: a retrospective multicenter analysis (KOSEN-005). J Neurosurg [Internet]. 2020;133:467–76. https://thejns.org/view/journals/j-neurosurg/133/2/article-p467.xml
Kong D-S, Young SM, Hong C-K, Kim Y-D, Hong SD, Choi JW, et al. Clinical and ophthalmological outcome of endoscopic transorbital surgery for cranioorbital tumors. J Neurosurg [Internet]. 2019;131:667–75. https://thejns.org/view/journals/j-neurosurg/131/3/article-p667.xml
Zabel A, Thilmann C, Schlegel W, Wannenmacher M. Management of benign cranial nonacoustic schwannomas by fractionated stereotactic radiotherapy. Int J Cancer [Internet]. 2001;96:356. http://doi.wiley.com/10.1002/ijc.1036
Kharod SM, Herman MP, Amdur RJ, Mendenhall WM. Fractionated Radiation Therapy for Benign Nonacoustic Schwannomas. Am J Clin Oncol [Internet]. 2018;41:13–7. https://journals.lww.com/00000421-201801000-00003
Goh ASC, Kim YD, Woo KI, Lee J-Il. Benign orbital apex tumors treated with multisession gamma knife radiosurgery. Ophthalmol [Internet]. 2013;120:635–41. https://linkinghub.elsevier.com/retrieve/pii/S0161642012007865
Author information
Authors and Affiliations
Contributions
YS: analysis and interpretation of data, drafting of paper and critical revision. VJ: conception or design of the work, acquisition of data, and critical revision. TD: conception or design of the work, acquisition of data, and critical revision. AH: conception or design of the work, acquisition of data, and critical revision. DM: conception or design of the work, acquisition of data, and critical revision. AW: conception or design of the work, acquisition of data, and critical revision. AY: conception or design of the work, acquisition of data, and critical revision. PS: conception or design of the work, acquisition of data, and critical revision. KIW: conception or design of the work, acquisition of data, and critical revision. TH: conception or design of the work, acquisition of data, and critical revision. BP: conception or design of the work, acquisition of data, and critical revision. KD: conception or design of the work, acquisition of data, and critical revision. DS: conception or design of the work, analysis and interpretation of data, and critical revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Shapira, Y., Juniat, V., Dave, T. et al. Orbito-cranial schwannoma—a multicentre experience. Eye 37, 48–53 (2023). https://doi.org/10.1038/s41433-021-01850-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01850-1