Abstract
Objectives
To describe a surgical technique and early post-operative outcomes for a novel glaucoma drainage device—the PAUL® glaucoma implant (PGI).
Methods
A consecutive cohort study of subjects who had PGI surgery between February 2019 and May 2020 with a minimum of 6-month follow-up. Primary outcome measures included failure (intraocular pressure (IOP) > 21 mmHg or a <20% reduction of IOP, removal of the implant, further glaucoma intervention or visual loss to no light perception). Secondary outcomes included mean IOP, mean number of medications, logMAR visual acuity (VA) and complications.
Results
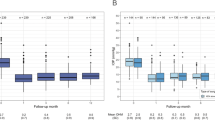
Ninety-nine eyes of 97 patients had a preoperative IOP (mean ± standard deviation) of 28.1 ± 9.0 mmHg, falling to 18.2 ± 6.8 mmHg at 1 month, 17.9 ± 6.7 mmHg at 3 months and 13.6 ± 4.7 mmHg at 6 months. 52 patients had a 12-month mean IOP of 13.3 ± 4.4 mmHg. The mean change in number of medications was a reduction of 2.38 ± 1.48. A significant reduction in the number of medications and intraocular pressure was demonstrated after PGI (p < 0.0001). No significant change was demonstrated in VA (p = 0.1158). A total of nine cases were deemed failures (six had <20% IOP reduction from baseline and three had IOP >21 mmHg). Thirty-eight (38.4%) of eyes had complete success and achieved an unmedicated IOP <21 mmHg. Ninety (90.1%) of eyes were qualified successes (with or without topical medications). Seventy-four (74.7%) eyes have achieved an intraocular pressure of <15 mmHg. Two cases of hypotony were observed.
Conclusion
This study presents a safe surgical technique, which significantly reduces IOP and number of medications with minimal complications.
Similar content being viewed by others
Introduction
Glaucoma is the leading cause of irreversible blindness worldwide and it is estimated that globally the number of people with glaucoma will increase by 74% from 2013 to 2040 due to increasing life expectancy and an ageing population [1]. Numerous multicentre, prospective randomised controlled trials have demonstrated that there is strong evidence that raised intraocular pressure (IOP) is a risk factor for the development and progression of glaucoma [2]. IOP reduction is currently the only therapeutic option available to treat glaucoma.
The use of glaucoma drainage implants (GDIs) to reduce the IOP in patients with glaucoma is increasingly favoured amongst surgeons [3]. GDIs are not only being used for refractory glaucoma but also increasingly as a primary surgical intervention [4]. The Baerveldt® implant was previously used at our centre as the primary GDI due to its higher efficacy data than its counterpart in the two comparison studies Ahmed versus Baerveldt study [5] and the Ahmed Baerveldt Comparison study [6], but the Baerveldt was also found to have a significantly higher risk of hypotony in these studies [5]. This demonstrated the need for a GDI with similar efficacy but with a reduced complication rate.
The PAUL® Glaucoma Implant is a new aqueous shunt device that has been developed with the intention to reduce post-operative complications seen with current shunts. The PAUL® Glaucoma Implant (PGI; Advanced Ophthalmic Innovations, Singapore, Republic of Singapore) is a non-valved glaucoma drainage device made using implantable medical-grade silicone. The tube diameter is smaller than that of the Molteno 3® (MOLTENO Ophthalmic Lt), Ahmed (New World Medical, Rancho Cucamonga, CA) and Baerveldt® tube (Johnson & Johnson Vision, Santa Ana, CA) with an external diameter of 467 mm and an internal diameter of 127 mm whilst having a large surface area endplate for aqueous absorption (342 mm2). The PGI plate has a length of 44.9 mm, which is larger than the Baerveldt and a width of 23 mm, which is smaller than the Baerveldt with less of the device lying beneath the recti muscles. In this paper, we describe our surgical technique for PGI implantation and review our early outcome data at the Manchester Royal Eye Hospital, UK.
Surgical technique
The procedure is performed either using sub-Tenon’s anaesthesia with 2% lidocaine and 0.5% bupivacaine or under general anaesthesia. The patient is positioned supine and 5% povidone-iodine applied to the periocular skin and conjunctival sac. The PGI (see Fig. 1a) is usually sited in the superotemporal quadrant but may be sited superonasally or inferonasally in specific cases. A corneal traction suture is used (7/0 Novofil® or 7/0 silk) to rotate the eye into down gaze. Conjunctival and Tenon’s peritomy are performed to expose the superotemporal quadrant. Minimal cautery is applied to the scleral bed. A conjunctival clamp is then applied to hold the conjunctiva and Tenon’s capsule whilst Mitomycin-C is applied to the space, using three corneal shields for 3 min (typically 0.5 mg/ml, but this concentration is reduced depending on the perceived conjunctival health) followed by thorough saline irrigation.
The plate is then inserted into the space and guided beneath the recti, which are located and held using squint hooks. The plate is then moved anteriorly to ensure that it is adequately held beneath the recti. The plate is then sutured to the sclera using 8/0 Ethilon® sutures, typically 8–10 mm back from the limbus. A portion of 6/0 prolene is then inserted into the PAUL® tube (see Fig. 1B). The purpose of the insertion of an intraluminal stent is to prevent early post-operative hypotony as this allows time for a plate capsule to form around the plate site. A Prolene stent was chosen as a suture material as the monofilament nature of the suture material allows ease of removal at a slit lamp setting. The 6/0 prolene size was chosen after experimentation of different suture sizes in a dry lab and intraoperative setting and this size demonstrated adequate aqueous flow.
The tube is then rested in place and cut in a bevelled manner to ensure a small short length within the anterior chamber and the prolene within the tube is maintained in position at the tip of the tube. The tunnel is then created using a 15° to create a deep scleral horizontal incision tunnel. A 26-G brown needle is then bent and used to tunnel a passage for the tube to pass. The tube is then sited in the anterior chamber. The plate is checked to demonstrate flow through the tube, and the tube is then secured using a 8/0 Ethilon® box suture to the underlying sclera to prevent tube movement (see Fig. 1C). Given the smaller lumen size and slow rate of flow at the plate, a ligation suture is not required as a part of the procedure. The entry site is checked to ensure no paratube leak. The 6/0 Prolene® intraluminal stent is placed into an inferior-temporal pocket in the conjunctiva.
Tutoplast® pericardium is then measured to the globe and cut to be placed as a double layer over the length of the tube externally (~6 × 6 mm) and this is then sited using TISSEEL (Baxter, US) glue onto the tutoplast or using 10/0 Ethilon® sutures to the scleral bed depending on surgeon preference (see Fig. 1D). Two slip knots are used to site the conjunctiva (10/0 Ethilon®) and the radial conjunctival incisions can be closed using TISSEEL® or further sutures if required. The anterior chamber can be reformed if required during the procedure e.g. balanced salt solution using a 30 G needle or an anterior chamber maintainer could be used if required. Subconjunctival cefuroxime 125 mg and Dexamethasone is then delivered. The patient then receives prednisolone 1% eye drops 6 × day for 2–3 months and chloramphenicol topically for 4 weeks. All glaucoma medications are ceased immediately post-op. Early post-operative raised pressure at week 1 or week 4–6 review can be managed by the addition of aqueous suppressants e.g. carbonic anhydrase inhibitors. The Prolene® stent can be removed post-operatively at 3 months or thereafter at the slit lamp in an outpatient setting.
Methods
This was a consecutive single centre retrospective evaluation of early post-operative outcomes and interventions for patient who had a PGI inserted between February 2019 and May 2020 under the supervision of five consultant surgeons at Manchester Royal Eye Hospital, UK. A minimum of 6 months follow up was required to be included in this study. The study was registered as a retrospective audit (audit number 9653). Patients under the age of 18 years were excluded.
Primary outcomes
The primary outcome was failure defined as the following:
(1) IOP out of target range (5–21 mmHg inclusive) or <20% reduction from baseline for two consecutive visits after 3 months.
(2) De novo glaucoma surgery required (e.g. cyclodestructive procedure, additional tube shunt).
(3) Removal of the implant.
(4) Severe vision loss related to the surgery (endophthalmitis, suprachoroidal haemorrhage with vision loss, enucleation, evisceration, or phthisis bulbi) or progression to no light perception for any reason.
The time to failure was defined as the time from surgical treatment to reoperation for glaucoma, loss of light perception vision, or the first of two consecutive study visits after 3 months in which the patient had persistent hypotony (IOP ≤ 5 mmHg) or inadequately reduced IOP (IOP > 21 mmHg or not reduced by 20% below baseline).
Eyes with successfully controlled unmedicated IOPs (≤21 mmHg and >5 mmHg and reduced by at least 20% from baseline) at 6 months, 12 months and the final visit were considered complete successes. Qualified success was deemed to be successfully controlled IOP, with or without medications at 6 months, 12 months and the final visit. Further IOP upper limits were determined including 12, 15 and 18 mmHg.
Secondary outcomes
Secondary outcome measures included complications. Early complications were considered to be a complication that occurred by the 3-month follow-up visit, whereas late complications were experienced after the 3-month follow-up visit. Post-operative complications included tube occlusion with iris/vitreous, choroidal effusion, suprachoroidal haemorrhage, cystoid macular oedema, shallow anterior chamber, hypotony maculopathy, endophthalmitis, cataract, diplopia, corneal oedema, and tube or shunt erosion, uveitis and tube malposition. A serious complication was defined as any complication, early or late, that required major surgery (reoperation in the operating room) to manage the complication, or both.
Clinic-based procedures at the slit lamp including Prolene® removal, needling, injection of viscoelastic gel into the anterior chamber were not considered as reoperation but were evaluated.
Further outcome measures included the number of medications required and the LogMAR visual acuity (VA) during the course of the follow up.
VA was assessed using LogMAR testing and numerical equivalents of low vision categories were used (counting fingers: 1.9 logMAR, hand movement: 2.3 logMAR, perception of light: 2.7 logMAR and no perception of light: 3.0 logMAR) as per Lange et al. [7].
Statistical analysis
All statistical analyses were performed using GraphPad Prism 6.0. Paired analyses of the data were performed using Wilcoxon matched-pairs signed rank test when data were non parametric and paired t-test when parametric. A p value of <0.05 was considered significant. Variables were reported as mean ± standard deviation (SD). Kaplan–Meier survival analyses were performed to analyse the time to failure from the date of implantation.
Results
Between February 2019 and May 2020, 99 eye of 97 patients had a PGI inserted at Manchester Royal Eye Hospital. The baseline demographics and ocular characteristics of the patients recruited are shown in Table 1 and demonstrate that 63.6% of patients were male. The mean age (±SD) was 58.7 ± 16.6 years. The mean follow-up time was 10.7 ± 3.2 months ranging from a minimum of 6–21 months. Ninety-eight eyes, 90 eyes, 89 eyes, 90 eyes and 52 eyes had follow up data up at week 1, month 1, month 3, month 6 and month 12, respectively. The surgical technique was as described above, however, due to the temporary problems with Mitomycin-C supply coinciding with the study period, 21 patients had the surgery performed using 5-fluorauracil and six patients without any antimetabolite. Four patients required a superonasal tube and one was sited inferonasally. One patient had the tube sited in the sulcus and one patient required vitrectomy at the time of surgery as they were aphakic.
Primary outcomes
A total of nine cases (9.3%) were deemed failures; the reasons for which were that six had <20% IOP reduction from baseline for two consecutive visits after 3 months and three patients had an IOP of 21 mmHg for two consecutive visits after 3 months. Figure 2 shows the Kaplan–Meier survival analysis for patients over the duration of their follow up.
Thirty-eight (38.4%) of eyes were found to have complete success at 6 months, 12 months and the final follow up visit and hence required no medication to achieve an IOP >5 and <21 mmHg. Ninety (90.1%) of eyes were qualified successes as they achieved an IOP >5 and <21 mmHg with or without topical medications at 6 months, 12 months and the final follow up visit. A further sub-analysis was performed to evaluate the differing final follow up IOP achieved. Fifty (50.1%) eyes had achieved an IOP of <12 mmHg (17 without medication). Seventy-four (74.7%) eyes had achieved an IOP of <15 mmHg (30 without medication). Ninety-one (91.9%) eyes had achieved an IOP of <18 mmHg (38 without medication).
The baseline mean IOP was 28.1 ± 9.0 mmHg, falling to 13.6 ± 5.4 mmHg at week 1 post-operatively, 18.2 ± 6.8 mmHg at 1 month, 17.9 ± 6.7 mmHg at 3 months and 13.6 ± 4.7 mmHg at 6 months. Fifty-two patients had 12-month follow up data with a mean IOP of 13.3 ± 4.4 mmHg. The IOP results include those patients in whom the intraluminal prolene was removed (56.6% of eyes) as described further in the secondary outcomes. Figure 3 demonstrates the IOP with 95% confidence intervals over a 12-month period. The mean final follow up IOP was 13.0 ± 3.75 mmHg. The mean change in IOP from the preoperative visit to the last visit was a reduction of 15.1 ± 8.87 mmHg (range: +3 to −47 mmHg). A Wilcoxon matched-pairs signed rank test showed that there was a significant difference between starting and final IOP (p < 0.0001****).
The mean number of medications used preoperatively was 3.61 ± 1.09, reducing to 0.14 ± 0.56 at 1 week post operatively, 0.44 ± 0.91 at 1 month, 1.06 ± 1.16 at 3 months and 1.22 ± 1.21 at 6 months. Fifty-two patients had 12-month follow-up data with a mean number of medications of 1.25 ± 1.28. The mean number of medications at the final follow up visit was 1.22 ± 1.23. The mean change in number of medications from the preoperative visit to the last visit was a reduction of 2.38 ± 1.48 (range: reduction of 5 medication to a gain of 1 medication). A Wilcoxon matched-pairs signed rank test showed that there was a significant difference between starting and final number of medications (p < 0.0001****).
Secondary outcomes
Hypotony was observed in two patients, one due to a leak from the anterior chamber maintainer site, which resolved upon re-suturing and a second that developed choroidal detachments and spontaneously resolved with observation. Two patients had complications that required return to theatre; one patient required suturing of their anterior chamber maintainer tract due to a leak resulting in hypotony, the second required revision of the tube and extension as the tube was short and not well-placed in the anterior chamber. There were no cases of endophthalmitis observed within the cohort. The early and late complications observed are demonstrated in Table 2.
The mean preoperative VA measured using logMAR was 0.68 ± 0.72, at 1 week post-operatively the VA was 0.87 ± 0.75, 0.67 ± 0.78 at 1 month, 0.62 ± 0.66 at 3 months and 0.55 ± 0.48 at 6 months. Fifty-two patients had 12-month follow up data with a mean VA of 0.55 ± 0.48. The mean final follow-up VA was 0.60 ± 0.633.
The mean change in logMAR VA from the preoperative visit to the last visit was minimal with a reduction of 0.08 ± 0.47 (Wilcoxon test p = 0.1158) (range: improvement 2.56 to a reduction in 1.76 logMAR). A Wilcoxon matched-pairs signed rank test showed that there was no significant difference between starting and final LogMAR VA (p = 0.1158).
The intraluminal Prolene® stent was removed in 56 (56.6%) eyes at a mean of 4.76 ± 2.90 months (ranging from 1.8 to 12.2 months) after surgery to reduce the IOP. This resulted in a mean reduction of pressure by 6.2 ± 9.0 mmHg and a mean reduction of 0.25 ± 1.37 medications, which were both statistically significant with Wilcoxon matched-pairs signed rank testing (p < 0.0001 for both parameters).
Twenty-one eyes of the cohort had implantation of the PAUL® tube performed with 5-fluorouracil due to a lack of availability of Mitomycin-C. A Chi-squared analysis revealed that there was no significant difference observed between the rates of complete and qualified success between the two cohorts (χ2 = 3.1264, p = 0.077).
Discussion
Prior to the PGI, the glaucoma drainage device of choice within this department had been the Baerveldt® glaucoma implant. The pooled data analysis of the Ahmed Baerveldt Comparison study and the Ahmed Versus Baerveldt study demonstrated that the Baerveldt tube achieved a 6-month mean IOP (±SD) of 15.0 ± 6.6 and 12-month mean IOP of 13.6 ± 5.9 mmHg and a mean number of medications of 1.2 ± 1.3 at 6 months and 1.4 ± 1.4 at 12 months in 247 cases [8]. The results in our cohort of 99 eyes demonstrated lower IOPs of 13.6 ± 4.7 at 6 months and similarly an IOP of 13.3 ± 4.4 mmHg at 12 months, and similar mean number of medications of 1.22 ± 1.21 at 6 months and 1.25 ± 1.28 at 12 months. The pooled Baerveldt® cohort demonstrated 4% of cases developed hypotony (11 eyes of 247) [8] whereas 2% of cases demonstrated hypotony in our group. This reveals that the PAUL® tube in our cohort has similar levels of IOP control as the Baerveldt tube, with fewer cases of hypotony. It is worth noting that one of the two hypotony cases in our cohort was due to leakage from the paracentesis site, hence not directly really related to the device itself. Analysis of the results of the PGI within this study demonstrated a 9.3% failure of the PGI at 1 year within this cohort. This was less than the cumulative probability of failure at 1 year within the Ahmed Baerveldt comparison study, which was 16.4% in the Ahmed® group and 14% in the Baerveldt® [9].
Koh et al. published 1-year results of the use of the PGI in a multicentre study (six centres). The results of 74 eyes demonstrated that 68.9% had complete success and 93.2% had qualified success [10], defined using the same parameters used in our cohort. Significant post-operative complications included self-limiting shallow anterior chamber (n = 11; 14.9%), hypotony requiring intervention (n = 7; 9.5%), tube shunt occlusion (n = 5; 6.8%), tube exposure (n = 3; 4.1%) and endophthalmitis with resultant loss of vision (n = 1; 1.4%) [10]. Review of the surgical technique within this paper demonstrated variability, with 14.9% having intraluminal stents compared to 100% of our cases, and some surgeons opting to use a viscoelastic over the plate and in the anterior chamber (although the number using this technique is not detailed). This study reported higher levels of hypotony (9.5%) compared to our study (2.0%). Whilst having these higher risks of hypotony with this technique, inversely patients in the Koh et al. study had lower mean IOP at 1 month and 3 months (14.9 ± 7.3 and 14.5 ± 4.6 mmHg, respectively) compared to our study (18.1 ± 6.79 mmHg). However, it is reassuring to find that at later time points, particularly considering that the Prolene® can be removed safely at a later time point whilst avoiding hypotony, the IOP in the Koh study was 13.8 ± 4.0 mmHg and 13.2 ± 3.3 mmHg at 6 and 12 months, respectively, and similarly within our study, it was 13.3 ± 4.4 and 13.3 ± 4.4 mmHg at 6 and 12 months, respectively. It is our belief that the technique of inserting a PGI without intraluminal stent but tamponading with viscoelastic can lead to variability in outcome and potential risk of higher rate of hypotony or, conversely, a hypertensive episode if too much viscoelastic is used. Our technique of using 6/0 Prolene® intraluminal stent without any viscoelastic allows immediate drainage (unlike the Baerveldt tube) and a more predictable IOP outcome within the first few weeks.
This study also evaluated PGIs that were implanted during the initial outbreak of the COVID-19 pandemic, a time when the immediate priority was the task of balancing individual patient’s risk of developing glaucoma-related visual impairment against their risk of death from COVID-19 and attending the hospital at this time [11]. The benefit found of using the PGIs was that given the safety profile of the device, the follow up intervals could be safely minimised (1 week, 1 month and 3 months). This is in comparison to the routine follow up after trabeculectomy, which usually require close monitoring with multiple follow up appointments (day 1 and up to weekly for 6 weeks) to ensure success. This is also in comparison to the Baerveldt tube, when patients require more frequent follow up (for example day one, week 1, week 3, week 5, week 7 and month 3) due to published higher risks of hypotony and the need to closely monitor this risk to coincide with the time of opening of the Vicryl® tie around the tube [8].
A limitation of this study was that for 2 months there was a lack of Mitomycin-C availability and therefore 27 eyes (27.3%) did not have Mitomycin-C applied (21 had 5-FU and 6 eyes had no Mitomycin-C applied). However, sub-analysis demonstrated no significant difference between these groups. The use of Mitomycin-C with glaucoma drainage device surgery is common practice, however, randomised prospective studies have demonstrated that intraoperative MMC is not effective in increasing the success rates of glaucoma drainage devices [12, 13]. Unfortunately, these studies were performed in respect to the Ahmed® valve and warrants further investigation for both the Baerveldt® and Paul® tube. Twelve-month data were only available for 52 eyes (52.5%), but these results demonstrated similar IOPs to those found in the study by Koh et al. [10]. A further limitation is that all follow-up intervals could not be performed for all patients enroled in the study due to the COVID-19 pandemic, for example only 89 of the 99 eyes (89.9%) attended a 3-month follow-up due to COVID-19 restrictions.
In summary, we believe that this is the first paper to demonstrate the safety and efficacy of PGI using a uniform standardised technique of 6/0 Prolene® intraluminal stent without any Vicryl® overtie or use of viscoelastic. We believe that this technique allows immediate and predictable drainage like the Ahmed valve but with the superior efficacy of a Baerveldt tube. It also offers excellent safety profile with low post-operative maintenance. The results of this study are encouraging and warrant further comparison with other forms of glaucoma surgical interventions and glaucoma drainage devices using rigorously designed randomised controlled trials.
Summary
What was known before
-
The PGI is a novel surgical glaucoma drainage device with a smaller lumen size (467 µm external, 127 µm internal) and preserves a large surface area of endplate for aqueous absorption (342 mm2).
-
Early studies have demonstrated successful lowering of IOP and number of medications as demonstrated by current glaucoma drainage devices.
What this study adds
-
This study presents a safe surgical technique to implant a PGI with few intraoperative and post-operative complications.
-
This study provides further evidence of the high rates of surgical success with the use of the PGI as a glaucoma drainage device.
References
Tham Y, Li X, Wong TY, Quigley HA, Aung T, Ed F, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2020;121:2081–90. https://doi.org/10.1016/j.ophtha.2014.05.013.
Miglior S, Bertuzzi F. Relationship between intraocular pressure and glaucoma onset and progression. Curr Opin Pharmacol. 2013;13:32–5.
Vinod K, Gedde SJ, Feuer WJ, Panarelli JF, Chang TC, Chen PP, et al. Practice preferences for glaucoma surgery: a survey of the American Glaucoma Society. J Glaucoma. 2017;26:687–93.
Agrawal P. Glaucoma drainage implants. Int J Ophthalmol. 2020;13:1318–28.
Christakis PG, Kalenak JW, Tsai JC, Zurakowski D, Kammer JA, Harasymowycz PJ, et al. The Ahmed Versus Baerveldt Study: five-year treatment outcomes. Ophthalmology. 2016;123:2093–102. https://doi.org/10.1016/j.ophtha.2016.06.035.
Budenz DL, Barton K, Gedde SJ, Feuer WJ, Schiffman J, Costa VP, et al. Five-year treatment outcomes in the ahmed baerveldt comparison study. Ophthalmology. 2015;122:308–16. https://doi.org/10.1016/j.ophtha.2014.08.043.
Lange C, Feltgen N, Junker B, Schulze-Bonsel K, Bach M. Resolving the clinical acuity categories “hand motion” and “counting fingers” using the Freiburg Visual Acuity Test (FrACT). Graefe’s Arch Clin Exp Ophthalmol. 2009;247:137–42. https://doi.org/10.1007/s00417-008-0926-0.
Tsai JC, Budenz DL. Five-year pooled data analysis of the Ahmed Baerveldt Comparison Study and the Ahmed Versus Baerveldt Study. Am J Ophthalmol. 2017;176:118–26. https://doi.org/10.1016/j.ajo.2017.01.003.
Budenz DL, Barton K, Feuer WJ, Schiffman J, Costa VP, Godfrey DG, et al. Treatment outcomes in the Ahmed baerveldt comparison study after 1 year of follow-up. Ophthalmology. 2011;118:443–52. https://doi.org/10.1016/j.ophtha.2010.07.016.
Koh V, Chew P, Triolo G, Lim KS, Barton K. Treatment outcomes using the PAUL glaucoma implant to control intraocular pressure in eyes with refractory glaucoma. Ophthalmol Glaucoma. 2020;1–10. https://doi.org/10.1016/j.ogla.2020.05.001.
Jayaram H, Strouthidis NG, Gazzard G. The COVID-19 pandemic will redefine the future delivery of glaucoma care. Eye. 2020;34:1203–5. https://doi.org/10.1038/s41433-020-0958-1.
Susanna R. Partial Tenon’s capsule resection with adjunctive mitomycin C in Ahmed glaucoma valve implant surgery. Br J Ophthalmol. 2003;87:994–8. https://doi.org/10.1136/bjo.87.8.994.
Costa VP, Azuara-Blanco A, Netland PA, Lesk MR, Arcieri ES. Efficacy and safety of adjunctive mitomycin C during Ahmed Glaucoma Valve implantation: a prospective randomized clinical trial. Ophthalmology. 2004;111:1071–6. https://doi.org/10.1016/j.ophtha.2003.09.037.
Author information
Authors and Affiliations
Contributions
Design of study—LA and NAV. Data collection—NAV, JTSY and FM. Analysis and writing of paper—NAV. Surgical procedures, review and approval of manuscript—KY, CHF, KME, AFS and LA.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vallabh, N.A., Mason, F., Yu, J.T.S. et al. Surgical technique, perioperative management and early outcome data of the PAUL® glaucoma drainage device. Eye 36, 1905–1910 (2022). https://doi.org/10.1038/s41433-021-01737-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01737-1
This article is cited by
-
Comment on: Surgical technique, perioperative management and early outcome data of the PAUL glaucoma drainage device, dated September 2021
Eye (2024)
-
Suprachoroidale Blutung nach Paul™ Tube-Stententfernung bei hoher Myopie
Die Ophthalmologie (2024)
-
The PAUL® glaucoma implant: 1-year results of a novel glaucoma drainage device in a paediatric cohort
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Münsteraner Standard: modifizierte PAUL®-Implantation bei Zustand nach PreserFlo® MicroShunt-Implantation. Videobeitrag
Die Ophthalmologie (2023)
-
Glaukomdrainageimplantate im Vergleich
Die Ophthalmologie (2023)