Abstract
Background/Objectives
To describe the predisposing factors, pathogens and outcomes in patients with clinical presumed concomitant microbial and herpes simplex keratitis (HSK) at Sydney Eye Hospital, Australia over a 5-year period.
Subjects/Methods
A retrospective case review was conducted. Patients with clinical presumed concomitant microbial and HSK from 2012 to 2016 were identified from pathology and hospital coding databases. Data were extracted from the medical records. VA was converted to the logarithm of the minimum angle of resolution (logMAR). ‘Poor’ outcome was defined as final VA worse than 6/60, or decrease in VA during treatment, or presence of complication, or needed surgical intervention.
Results
126 episodes in 121 patients were included; median age 70 years (range 18–96); 56% male. Predisposing factors included blepharitis 20/126 (16%) cases, and corneal transplantation 19 (15%). Forty-six (37%) cases had prior HSK. Coagulase-negative staphylococci 51/116 (44%), Staphylococcus aureus 11 (9%), and Pseudomonas aeruginosa 11 (9%) were the most common isolates. The median VA at initial visit was 1.7 logMAR (range 0.04–2.7) and at final visit, 0.98 logMAR (range 0–2.7) (P < 0.05). Complications occurred in 70 episodes: persistent epithelial defect in 38 (30%); intraocular pressure elevation in 15 (12%), and corneal perforation in 12 (10%). ‘Poor’ outcome was recorded in 46/75 (61%) episodes.
Conclusions
Patients with clinical presumed concomitant microbial and HSK face significant ocular morbidity and poor visual outcome. In our setting, previous HSK, corneal and ocular surface disease, were common predisposing factors and Gram-positive bacteria were the most commonly associated organisms.
Similar content being viewed by others
Introduction
Microbial keratitis has become a significant cause of monocular blindness worldwide [1,2,3]. Contact lens wear is most associated with microbial keratitis in the United States (USA) [3]; whereas ocular trauma predisposes to the infection in developing countries [3]. Several studies have described herpes simplex keratitis (HSK) as a predisposing factor for microbial keratitis [4,5,6,7,8,9,10,11,12]. Moreover, microbial keratitis can occur with HSK [5, 9]. In fact, the differential diagnoses of stromal HSK with ulceration are all forms of microbial keratitis and herpes zoster keratitis [13].
Microbial keratitis has also been described as a ‘superinfection’ or ‘secondary infection’ complicating HSK [14]. Some case reports have indicated that topical anti-viral medications and/or topical corticosteroids used in HSK might predispose to secondary bacterial keratitis [15, 16]. Case series of patients with HSK and secondary microbial keratitis are scarce. Two case series from USA included limited patient numbers (Nissenkorn and Wood [n = 9] [17] and Boisjoly et al. [n = 15] [18]), and another series from London, 85 patients [14]. These studies reported that the presence of an epithelial defect, the history of keratouveitis and of corneal graft, and the use of topical corticosteroids increased the risk of superinfection [14, 17, 18]. Gram-positive cocci were mostly isolated [14, 17], and almost half of the patients had a final visual acuity (VA) of <6/60 in London [14]. Predisposing factors and microbiology patterns found in these studies may be still relevant these days. However, the first line therapies have changed. Previously, antibiotics such as penicillin and methicillin were used for initial therapy. While, erythromycin, bacitracin, neomycin–polymyxin B combination, or chloramphenicol were used for prophylactic therapy; to patients with damaged corneal epithelium [14, 17, 18].
Many case series worldwide have described the risk factors, microbiology spectrum, antimicrobial therapy and outcomes of microbial keratitis alone; however, little is known whether these features vary in clinical presumed concomitant microbial keratitis and HSK cases. We reviewed clinical presumed cases with this condition to identify the abovementioned features.
Methods
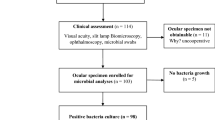
A retrospective case series over the 5 years, 2012–2016 was conducted at The Sydney Eye Hospital, a quaternary referral unit for eye diseases located in the central business district of Sydney, New South Wales, Australia. All patients with microbial keratitis were identified from the following International Classification of Disease, 10th revision (ICD-10) codes: corneal ulcer (H16.0), other superficial keratitis without conjunctivitis (H16.1), keratoconjunctivitis (H16.2), interstitial and deep keratitis (H16.3), other keratitis (H16.8) and keratitis, unspecified (H16.9); and by querying a laboratory information system containing pathology results.
Clinical presumed concomitant microbial keratitis and HSK cases were determined in alignment with clinical practice as follows:
-
1.
Patients over 18 years of age, AND
-
2.
Patients with a clinical diagnosis of presumed concomitant microbial keratitis and HSK who presented the Sydney Eye Hospital from 2012 to 2016, AND
-
3.
Patients had a corneal scrape performed at initial presentation, OR
-
4.
Had a previous history of HSV.
A clinical diagnosis of presumed concomitant microbial keratitis and HSK was made by the treating clinician based on the clinical features (history and examination) and prior history of HSV infection along with the prescription of a therapeutic dose of antiviral. These definitions were chosen to align with clinical practice.
Each separate episode of keratitis suffered by a patient during the period was interpreted as an individual case.
Patients were excluded if the initial diagnosis was an auto-immune-related non-infectious keratitis, neurotrophic corneal ulcer, corneal perforation, or trauma. Neurotrophic ulceration was excluded as it was not considered to be an active HSV infection that is associated with increased viral load. Rather neurotrophic ulceration follows episodes of HSK.
Ethics approval was obtained from the South Eastern Sydney Local Health District Human Resources Ethics Committee (approval number: HREC 14/282). Data are reported in line with the STROBE statement for observational data [19]. Study data were collected and managed using REDCap (Research Electronic Data Capture, Nashville, TN, USA) hosted at The University of Sydney [20]. Medical records were reviewed, and the following data extracted: demographics, ocular predisposing factors [5,6,7, 10, 21], clinical signs at presentation, such as epithelial defect and infiltrates measurements, and management.
Corneal scrapes and specimens for HSV polymerase chain reaction (PCR) test were taken in accord with local protocols [22]. A positive culture was defined as any bacterial and/or fungal growth present on the solid media. Bacteria were identified by matrix-assisted laser desorption ionisation-time of flight (MALDI-TOF) mass spectrometry using an Ultraflex LT with v 3.0 software (Bruker Daltonics® Germany). Antibiotic susceptibilities were determined by the calibrated dichotomous susceptibility (CDS) method [23] and the breakpoints for resistance were in accord with those specified in the CDS method for systemic isolates. Methods have been described elsewhere [24]. Corneal biopsy was performed according to methods described elsewhere [25] and processed for histopathology and microbiology.
Herpes Simplex Virus type 1 and type 2 (HSV-1, HSV-2) were detected using the HSV-1 HSV-2 VZV R-gene kit, a real-time PCR on DNA extracted from human clinical samples (Argene, Australia) according to manufacturer’s instructions. The PCR testing was performed by the attending medical practitioner. The tests were performed using a Roche LC480 thermal cycler for real time amplification and results reported as viral genome copies/ml and calculated log10 copies/ml. Positive and negative controls were used as standard [26].
VA at the presentation to the hospital and at discharge or at the last outpatient visit was recorded. The VA was measured using Snellen projector charts, unaided or aided with their usual means of correction (glasses or contact lens). The Snellen fractions in combination with any letters incorrectly identified or any letters correctly identified on smaller lines were converted to the logarithm of the minimum angle of resolution (logMAR) for further analysis. VA for counting fingers was converted to 1.7 logMAR, hand movement 2.0 logMAR, light perception 2.3 logMAR and no light perception 3.0 logMAR [27].
Following a review of the literature, these outcomes were chosen to enable comparison of our results with a microbial keratitis case series from Brisbane, Australia [28]. The data needed to create these outcome groups was easily available in our medical notes. Outcomes were grouped as follows: [28]
-
1.
Good outcome: final VA of 6/12 or better, and no complications or surgical intervention, and no decrease in VA during treatment.
-
2.
Moderate outcome: final VA 6/15–6/60, and no complications or surgical intervention, and no decrease in VA during treatment.
-
3.
Poor outcome: final VA worse than 6/60 or decrease in VA during treatment; or complication of infection (perforation or endophthalmitis), or requiring surgical intervention (penetrating keratoplasty (PK), enucleation or evisceration).
Statistical analysis
Descriptive statistics were used to summarise all continuous and categorical variables for this case series. Sociodemographic, predisposing factors and clinical feature data were compared among outcomes and statistical significance assessed using the chi-square test for proportions and Kruskal-Wallis test for non-parametric distributed variables (age, symptom duration and ulcer size). Epithelial defect and infiltrates size were defined as the geometric mean of the longest diameter of the lesion and its perpendicular diameter. Change in VA (logMAR) was investigated using a Wilcoxon test. A p-value < 0.05 was considered as evidence of statistical significance. The statistical software used was IBM SPSS Statistics Desktop Version 25 (IBM Corp, Armonk, NY).
Results
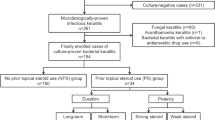
After cross-referencing the datasets, 1581 medical records were identified and reviewed. After applying the inclusion and exclusion criteria, 126 episodes from 121 patients were included. There were 118 patients with one episode of concomitant keratitis, two patients with two episodes (one patient presented with bilateral infection), and one patient with four episodes. The mean age of all patients was 64 years and 56% were male. Patients presented to hospital within a week of the onset of symptoms and most were treated as inpatients (Table 1). Ninety-six of 126 (76%) episodes were seen by another health professional prior the initial visit to the Sydney Eye Hospital. Of these, 79 were seen by an external ophthalmologist, 18 by a general practitioner, and 6 by an optometrist. Of these 96 episodes, 49 received topical antibiotics, 21 topical aciclovir, 12 oral valaciclovir, 1 trifluridine, and 21 glaucoma eye drops.
A presumed predisposing factor for microbial keratitis was found in 115 of 126 episodes (91%). A single predisposing factor was found in 35 (30%). Table 2 illustrates the predisposing factors.
-
Clinical findings
An epithelial defect was identified in 107 of 126 episodes (85%) and measured in 82 (77%). Of these, 57 (70%) epithelial defects measured over 2 mm. The median area of epithelial defect was 8.2 mm2 (IQR 2.2–18, range 0.04–121). Infiltrate was present in 81 of 126 episodes (64%) and measured on 44 (54%). The median area of the infiltrate was 3.5 mm2 (IQR 1–10.9 mm2, range 0.04–100). Other findings included hypopyon in 33 episodes (26%); corneal thinning in 25 (20%); satellite lesions in 16 (13%); ring infiltrates in 9 (7%); and a perforation that was Seidel negative in 4 (3%), and Seidel positive in 6 (5%).
-
Microbiological data
One hundred and thirty-seven corneal scrapes were performed in 126 episodes. Eleven episodes had two corneal scrapes performed during management of the disease. Culture positivity was 67% (n = 92/137) and 116 organisms were identified. Bacterial keratitis accounted for 110 of the positive growths (95% of all isolates). The predominant organisms were the coagulase-negative staphylococci (CoNS) group [(51 of 116), 44%) with Staphylococcus epidermidis as the major species (n = 35), Pseudomonas aeruginosa [(11 of 116, 9%], and Staphylococcus aureus [(11 of 116, 9%]. Polymicrobial infection was detected in 20 of 137 scrapes (15%) (Table 3).
Of the CoNS, 18% (9/51) were resistant to cefalotin, 14% (7/51) resistant to chloramphenicol, 12% (6/51) resistant to gentamicin, and 8% (4/51) resistant to ciprofloxacin. Of the methicillin-sensitive S. aureus (MSSA) isolates identified, 37.5% (3/8) were resistant to ciprofloxacin and 12.5% (1/8) resistant to gentamicin. All Gram-positive isolates were susceptible to vancomycin. All P. aeruginosa isolates were susceptible to ciprofloxacin, gentamicin and tobramycin.
-
Corneal biopsy
A corneal biopsy was performed in 10 of 126 episodes (8%) at a median time of 19 days (IQR 9–32, range 5–145) with 60% of culture positivity. A non-resolving infection despite the appropriate antibiotic treatment in accordance to the corneal scrape’s culture result was the indication for corneal biopsies. S. epidermidis (n = 2), Acanthamoeba cysts (n = 2), Serratia ureilytica (n = 1), and an unspecified fungus (n = 1) were isolated in the cultures.
-
PCR test for herpes simplex virus
Herpes simplex virus PCR was performed in 91% of episodes (115/126). The test was positive in 31 of 115 episodes (27%). Of these, 16 (52%) had no previous history of HSK and 12 (39%) were culture negative for bacteria.
-
Initial therapy
The most common initial therapy was a combination of cefalotin 5% and gentamicin 0.9%, oral valaciclovir and homatropine. Upon receipt of microbiology results, anti-microbial therapy was changed in 119 of 126 episodes (94%) Of these, 83 (70%) had a positive culture and 36 (30%) had a negative culture from corneal scrape.
-
Anti-inflammatory treatment
Eighty-one of 126 episodes (64%) received topical corticosteroids at some point during their treatment. Seven episodes received topical corticosteroids as part of the initial therapy. For the rest of the episodes, topical corticosteroids were commenced at a median time of 5 days (IQR 3–6, range 0–124) after initial presentation. Topical corticosteroid therapy was given for a median time of 11 days (IQR 3–88, range 1–114 days) to 19 episodes.
-
Outcomes
An outcome was determined in 75 of 126 episodes (60%). The remaining 51 episodes were lost to follow up, followed up by private ophthalmologists or had missing information on their medical records. Moderate and poor outcomes occurred mainly in patients over 60 years of age (Table 4). Patients with a poor outcome were significantly older (75 years vs. 66 years in moderate outcome vs. 47 years in good outcome, p = 0.005), and presented with worse VA at initial presentation (median 2 logMAR vs. 1.3 logMAR in moderate outcome vs, 0.8 logMAR in good outcome, p < 0.001); and larger ulcers (median stromal infiltrate size 6 vs. 5.46 mm2 vs. 1.06 mm2, p = 0.04). There was no significant statistical association between ocular history and the outcomes.
Final clinical findings
The epithelial defect healed in 65 of 120 episodes (54%) with a median healing time of 11 days (IQR 7–26, range 1–153). Corneal thinning, neovascularisation and scarring were identified at clinical examination in 9% (n = 11), 11% (n = 13) and 33% (n = 39) of episodes, respectively.
Visual acuity
Overall, the median VA at presentation improved from 1.7 to 0.7 logMAR (p < 0.05), where logMAR of 0 is equivalent to 6/6, and a logMAR of 1 is equivalent to 6/60. Eighteen eyes (31%) had a final VA of 6/12 (0.3 logMAR) or better; 15 (26%), between 6/12 and 6/60 (0.3 logMAR and 1 logMAR); and 25 (43%), 6/60 (1 logMAR) or worse.
Complications
Seventy of 126 episodes (55%) experienced complications (Table 5). Of the 38 episodes with persistent epithelial defect, tarsorrhaphy was performed in 18 and amniotic membrane grafting in one. Eight episodes required a PK at a median time of 8 days (IQR 5–14, range 4–21). Chaetomium spp. (n = 1), unspecified fungi (n = 1) and Corynebacterium propinquum (n = 1) were isolated in the non-resolving infection cases which needed a PK. Lamellar keratoplasty (LK) was required in one episode with a non-resolving infection to manage a descemetocele formation. The patient had a history of keratoconus and corneal transplant and two negative cultures from corneal scrapes. Evisceration was performed in five episodes with causal organisms isolated in four episodes (S. ureilytica, S. epidermidis, P. aeruginosa and Moraxella nonliquefaciens). Enucleation was required in one episode caused by P. aeruginosa.
Discussion
This study reported predisposing factors, clinical findings, microbiological patterns, anti-microbial therapy and outcomes of adults with clinically presumed concomitant microbial keratitis and HSK presenting to the Sydney Eye Hospital over a 5-year period. There are a few out-dated case reports and a retrospective study describing secondary microbial keratitis in HSK from 1980s [14, 17, 18]. Clinicians in practice however are interested to know if patients with concomitant microbial keratitis and HSK are different to those with microbial keratitis alone, as this data could be used to assist diagnosis and management. The most common presumed predisposing factors in this study were topical corticosteroid use, ocular surface disease including prior HSK and corneal transplant. CoNS were the most common isolated microorganisms. Patients with poor outcomes were likely to be older, presenting with poor vision acuity and larger ulcers.
Correct initial diagnosis of microbial keratitis based only on clinical features is challenging. Hence the need of a good medical history and diagnostic tests to guide the appropriate therapy. In this study, 65% of the patients were 60 years or older suggesting that this condition may occur more frequently in the elderly. The mean age (64 years) was higher than the mean age of patients with suppurative keratitis and prior HSK in London (55 years) [14]. Previous ocular disease and surgery, topical corticosteroid use, immunosuppressive conditions and medications have been reported as the main predisposing factors among the elderly with microbial keratitis [5, 10, 21], and among patients with HSK and secondary microbial keratitis [14, 17, 18]. The importance of these predisposing factors was comparable to this study as the main risk factors were topical corticosteroid use (38%), previous HSK (37%), and blepharitis/dry eye (22%). These findings were similar to a case series in the Netherlands where the use of topical corticosteroids (26%), dry eye/blepharitis (21%) and prior HSK (29%) were prevalent in patients over 60 years of age [10]. This Dutch study included all cases of microbial keratitis but divided the patients into two groups for analysis (under 60 years vs. over 60 years) to elicit any differences between younger and elder patients [10].
The overall culture positive rate was 67% comparable to previous Australian microbial keratitis series (70.8% [9], 65% [21], 63.5% [29]); and a Indian microbial keratitis series in the elderly (67.3%) [30]. This is not surprising as similar techniques were used to isolate and culture the organisms across our and the reported studies. Gram-positive isolates were identified in 72% of all organisms in our study being comparable with other microbial keratitis studies [5, 7,8,9,10, 14, 29,30,31,32,33]. A standard regimen of fortified antibiotics and oral valaciclovir was the most common initial therapy in this study. Oral valaciclovir was the most common antiviral prescribed as the patients were already receiving multiple topical medications and a topical antiviral ointment might affect the penetration of the antibiotics, produce additional toxicity or cause issues with drop compliance. Further, most of these cases presented with signs of stromal keratitis and an oral antiviral is the preferred therapy for this type of keratitis [13]. Initial antibiotics were mainly switched according to the sensitivity reporting. The empiric therapy was also altered in the episodes with a negative culture (30%) probably due to the antibiotic toxicity which could affect healing [3, 6]. The empiric therapy tended to be changed to chloramphenicol eye drops or ointment, tobramycin ointment or ofloxacin which are readily available in community pharmacies. Therefore, clinicians change initial antibiotics to something the patient will easily be able to obtain after discharge.
Furthermore, about two-thirds of episodes were given a topical steroid therapy in combination with antibiotics. This practice does not follow the recommendations from Steroids for Corneal Ulcers Trial (SCUT) [34] and clinical guidelines to prescribe topical steroids in microbial keratitis which have shown beneficial effect on visual outcomes. Topical steroids were commenced at a median time of 5 days, later than recommended by the SCUT; but similar to a microbial keratitis study from Brisbane, at 7 days [35]. Reasons for not prescribing topical steroids may be that clinicians were lack of confidence in commencing this medication as it could be caused by fungus, or the disease worsened rapidly due to the predisposing factors or the virulence of the organism.
The SCUT and Green et al. reported that the median time of reepithelialisation was 7 [34] and 9 days [21], respectively. However, in this study, the ulcers tended to heal couple of days later (11 days). In this study; corneal perforation, resulting from the infection, was mainly treated with glueing (8/13, 60%). The rate of PK [6% (8/126)] was much lower than the rates reported in previous series of microbial keratitis in the elderly in India (10.8%) [31], Australia (17.9%) [5], and The Netherlands; (27.6%) [10] and a case series with patients with HSK and secondary microbial keratitis in United Kingdom (UK) (48%) [14]. PK was performed due to corneal perforation or to non-resolving microbial keratitis. Perhaps, the clinicians at our institution intended to avoid PK in eyes with history of HSK and persisted with a conservative approach for longer.
The proportion of evisceration/enucleation has varied in previous microbial keratitis studies worldwide. Evisceration/enucleation resulted from non-resolving microbial keratitis progressing to endophthalmitis. The proportion of eyes requiring evisceration/enucleation (5%) was lower than in previous studies with elderly population with microbial keratitis from India (14.7%) [31] and Australia (8.9%) [5]. Nevertheless, this proportion was comparable with the study of microbial keratitis in the elderly from the Netherlands (4%) [10] and with the study with patients with HSK and secondary microbial keratitis from UK (3%) [14].
Overall, the patients had a poor presenting median VA of 1.7 logMAR (count fingers) and final visual outcome of 0.7 logMAR (6/30) with 43% (n = 25/58) with a VA worse than 6/60. The poorer initial vision was likely due to prior ocular disease, including HSK. These findings were comparable with the findings from the microbial keratitis study in the elderly from Sydney which reported poor initial VA of 6/300 with over 40% of patients with a final VA worse than 6/60 [5]. Similarly, Wilhelmus reported a similar proportion of patients with final VA worse than 6/60 [45% (18/40)] [14]. Among various microbial keratitis studies, VA at presentation is poor regardless of the age group; but it is noted that older patients consistently seem to achieve poorer final VA [10, 30, 31]. Perhaps the lack of steroid therapy may explain the poor outcomes of these patients.
The main limitation of this study was the inclusion criteria used to identify episodes of concomitant microbial keratitis and HSK. It can be difficult for clinicians to diagnose HSK in addition to microbial keratitis [13]. This is because the symptoms and signs are overlapping, and the investigations can be non-confirmatory. In HSK, PCR is not universally performed if there is a prior diagnosis of HSK and is often negative in stromal HSK without ulceration, endothelial HSK and keratouveitis [36]. Similarly, corneal scrapes are not always positive in microbial keratitis. Further, the results from such investigations are not available at the time of presentation which is when treatment is commenced by the clinician. In practice, the diagnosis of ‘concomitant’ herpetic keratitis with microbial keratitis is typically made clinically and treatment commenced. For the clinical diagnosis the clinicians make an assessment based on the history and clinical features. As a result of the above issues, an important limitation is that although some cases had positive HSV PCR, indicating an active viral replication, the remaining cases with negative HSV PCR were still included in the study because they had history of HSK indicating an immune-related HSK (stromal HSK, endothelial HSK, or keratouveitis); as in these cases PCR is typically negative. Another limitation is its retrospective nature introducing risks of selection bias and misclassification. Clinical data collected was only that recorded. Nonetheless, this is a recent large series of cases with presumed concomitant microbial keratitis and HSK over 5 years to be reported from Australia.
These cases of clinical presumed concomitant microbial keratitis and HSK are considered to correlate more closely to the microbial keratitis in the elderly. These cases were likely to present with poor vision and severe disease (large ulcers) in patients over 60 years of age with at least one predisposing factor. The predisposing factors were highlighted, including corneal or ocular surface disease, history of prior HSK, and topical corticosteroid use. The microbiological spectrum was comparable to microbial keratitis series with Gram-positive isolates being the most common culprit of the infection. The outcomes of our patients were comparable to the poor outcomes reported in several studies in elderly patients with microbial keratitis. In our study, 1 out of 3 episodes resulted with a poor final VA worse than 6/60 and/or a need of a surgery. To improve outcomes for patients with mixed infection, there is a need for earlier diagnosis via increased suspicion in patients with risk factors and rapid diagnostic techniques.
Summary
What was known before
-
Herpes simplex keratitis can occur with microbial keratitis.
What this study adds
-
Clinical presumed concomitant microbial and herpes simplex keratitis occurs mostly in elderly patients who present poor vision and large ulcers. Common predisposing factors: corneal graft, blepharitis, history of prior HSK, and topical corticosteroid use.
-
The commonest isolated organism was coagulase-negative staphylococci.
References
Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ. 2001;79:214–21.
Stapleton F, Keay LJ, Sanfilippo PG, Katiyar S, Edwards KP, Naduvilath T. Relationship between climate, disease severity, and causative organism for contact lens-associated microbial keratitis in Australia. Am J Ophthalmol. 2007;144:690–8.
Austin A, Lietman T, Rose-Nussbaumer J. Update on the management of infectious keratitis. Ophthalmology. 2017;124:1678–89.
Musch DC, Sugar A, Meyer RF. Demographic and predisposing factors in corneal ulceration. Arch Ophthalmol. 1983;101:1545–8.
Butler TK, Spencer NA, Chan CC, Singh Gilhotra J, McClellan K. Infective keratitis in older patients: a 4 year review, 1998–2002. Br J Ophthalmol. 2005;89:591–6.
Allan BD, Dart JK. Strategies for the management of microbial keratitis. Br J Ophthalmol. 1995;79:777–86.
Keay L, Edwards K, Naduvilath T, Taylor HR, Snibson GR, Forde K, et al. Microbial keratitis predisposing factors and morbidity. Ophthalmology 2006;113:109–16.
Ly CN, Pham JN, Badenoch PR, Bell SM, Hawkins G, Rafferty DL, et al. Bacteria commonly isolated from keratitis specimens retain antibiotic susceptibility to fluoroquinolones and gentamicin plus cephalothin. Clin Exp Ophthalmol. 2006;34:44–50.
Gebauer A, McGhee CN, Crawford GJ. Severe microbial keratitis in temperate and tropical Western Australia. Eye 1996;10:575–80.
van der Meulen IJ, van Rooij J, Nieuwendaal CP, Van Cleijnenbreugel H, Geerards AJ, Remeijer L. Age-related risk factors, culture outcomes, and prognosis in patients admitted with infectious keratitis to two Dutch tertiary referral centers. Cornea 2008;27:539–44.
Bourcier T, Thomas F, Borderie V, Chaumeil C, Laroche L. Bacterial keratitis: predisposing factors, clinical and microbiological review of 300 cases. Br J Ophthalmol. 2003;87:834–8.
Ng AL-K, To KK-W, Choi CC-L, Yuen LH, Yim S-M, Chan KS-K, et al. Predisposing factors, microbial characteristics, and clinical outcome of microbial keratitis in a tertiary Centre in Hong Kong: a 10-year experience. J Ophthalmol. 2015;2015:9.
White ML, Chodosh J. Herpes Simplex virus keratitis: a treatment guideline. San Francisco: Hoskins Center for Quality Eye Care, American Academy of Ophthalmology; 2014.
Wilhelmus KR. Suppurative corneal ulceration following herpetic keratitis. Doc Ophthalmol. 1982;53:17–36.
Dohlman CH, Zucker BB. Long-term treatment with idoxuridine and steroids: a complication in herpetic keratitis. Arch Ophthalmol. 1965;74:172–4.
Dinning WJ. Steroids and the eye-indications and complications. Postgrad Med J. 1976;52:634–8.
Nissenkorn I, Wood TO. Secondary bacterial infections in herpes simplex keratitis. Ann Ophthalmol. 1982;14:757–9.
Boisjoly HM, Pavan-Langston D, Kenyon KR, Baker AS. Superinfections in herpes simplex keratitis. Am J Ophthalmol. 1983;96:354–61.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–9.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Green M, Apel A, Stapleton F. Risk factors and causative organisms in microbial keratitis. Cornea 2008;27:22–7.
Khoo P, Cabrera-Aguas M, Hollhumer R, Watson S. An educational video to improve the diagnostic yield from corneal scrapes for microbial keratitis. Clin Exp Ophthalmol. 2017;45:84.
Bell SM, Pham JN, Rafferty DL, Allerton JK. Antibiotic susceptibility testing by CDS method. Department of Microbiology (SEALS)-St George Hospital. 2016. http://cdstest.net.
Watson S, Cabrera-Aguas M, Khoo P, Pratama R, Gatus BJ, Gulholm T, et al. Keratitis antimicrobial resistance surveillance program, Sydney, Australia: 2016 annual report. Clin Exp Ophthalmol. 2019;47:20–5.
Robaei D, Chan UT, Khoo P, Cherepanoff S, Li Y-C, Hanrahan J, et al. Corneal biopsy for diagnosis of recalcitrant microbial keratitis. Graefes Arch Clin Exp Ophthalmol. 2018;256:1527–33.
Biomerieux. Argene, HSV1 HSV2 VZV R-gene real time detection and quantification kit. Marcy-l′Etoile, France: Biomerieux; 2016.
Lee J, Lai J, Yick D, Tse R. Retrospective case series on the long-term visual and intraocular pressure outcomes of phacomorphic glaucoma. Eye 2010;24:1675–80.
Green M, Apel A, Naduvilath T, Stapleton F. Clinical outcomes of keratitis. Clin Exp Ophthalmol. 2007;35:421–6.
Leibovitch I, Lai TF, Senarath L, Hsuan J, Selva D. Infectious keratitis in South Australia: emerging resistance to cephazolin. Eur J Ophthalmol. 2005;15:23–6.
Parmar P, Salman A, Kalavathy CM, Kaliamurthy J, Thomas PA, Jesudasan CA. Microbial keratitis at extremes of age. Cornea 2006;25:153–8.
Kunimoto DY, Sharma S, Garg P, Gopinathan U, Miller D, Rao GN. Corneal ulceration in the elderly in Hyderabad, south India. Br J Ophthalmol. 2000;84:54.
Passos RM, Cariello AJ, Yu MC, Hofling-Lima AL. Microbial keratitis in the elderly: a 32-year review. Arq Bras Oftalmol. 2010;73:315–9.
Toriyama K, Suzuki T, Shiraishi A. Characteristics of infectious keratitis in old and very old patients. J Ocul Pharm Ther. 2018;34:565–9.
Srinivasan M, Mascarenhas J, Rajaraman R, Ravindran M, Lalitha P, O’Brien KS, et al. The steroids for corneal ulcers trial (SCUT): secondary 12-month clinical outcomes of a randomized controlled trial. Am J Ophthalmol. 2014;157:327–33.e3.
Green M, Hughes I, Hogden J, Sara S, Apel A, Stapleton F. High-dose steroid treatment of bacterial keratitis. Cornea. 2019;38:135–40.
Cabrera-Aguas M, Kerdraon Y, Watson SL. Diagnosis using polymerase chain reaction and outcomes in herpes simplex keratitis. Acta Ophthalmol. 2020. https://doi.org/10.1111/aos.14601.
Acknowledgements
The authors acknowledge the corneal unit at the Sydney Eye Hospital who managed the patients with microbial keratitis in this case series.
Funding
Professor Stephanie Watson is supported by the Sydney Medical School Foundation. The Sydney Eye Hospital Foundation supported the study.
Author information
Authors and Affiliations
Contributions
MC-A was responsible for designing the protocol, writing the protocol and manuscript, extracting and analysing data, interpreting results, updating the reference list and creating tables. PK was responsible for data extraction and provided feedback on the manuscript. CRRG was responsible for interpreting results and provided feedback on the manuscript. MML was responsible of providing raw data, interpreting results and provided feedback on the manuscript. SLW was responsible for designing the protocol, writing the protocol, interpreting results and provided feedback on the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cabrera-Aguas, M., Khoo, P., George, C.R.R. et al. Predisposing factors, microbiological features and outcomes of patients with clinical presumed concomitant microbial and herpes simplex keratitis. Eye 36, 86–94 (2022). https://doi.org/10.1038/s41433-021-01440-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01440-1