Abstract
Background
The purpose of this study was to evaluate macula, retinal nerve layer (RNFL), ganglion cell layer (GCL), inner plexiform layer (IPL) and macular nerve fibre layer (mNFL) thickness in patients with pituitary tumours who has normal visual field (VF).
Methods
Thirty-five eyes of 35 patients with pituitary tumours with normal VF and 41 eyes of 41-healthy subjects were underwent a complete ophthalmic examination. The spectral domain- optical coherence tomography (OCT) was used to measure macular and optic disc parameters. Layer-by-layer segmentation was done automatically by using the new software. Data analyses were performed by using SPSS for Windows, version 22.0.
Results
Average of total macula thickness inner temporal (p: 0.006), outer temporal (p < 0.001), inner nasal (p: 0.03), outer nasal (<0.001) were significantly lower in pituitary tumour group than normal group. Average of RNFL (p:0.009), temporal (p: 0.001), superiotemporal (p:0.004) and inferiotemporal (p: 0.01) were significantly lower in pituitary tumour group than normal group. Average of central GCL (p: 0.01) and central NFL (p: 0.03) were significantly lower in pituitary tumour group than normal group. There was no statistically significant difference between the two groups in IPL averages.
Conclusions
Pituitary tumour patients with normal VF had reduced nasal and temporal section of the total macula, temporal RNFL, central mGCL and mNFL thicknesses, reflecting the corresponding to the anatomical substrate of the underlying pathology of chiasmal compression. This indicates that the presence of retinal thinning may be a sign of early detection of anterior visual pathway injury before VF loss becomes apparent.
Similar content being viewed by others
Introduction
Pituitary tumours are common intracranial neoplasm and they constitute 15% of all intracranial neoplasms [1]. They are associated with endocrine system dysfunction, compression signs and symptoms by mass effect to the adjacent structures [2]. Compression of the optic chiasm can lead to loss of visual function by retrograde degeneration to retinal ganglion cells [3]. Neuro-ophthalmic pathologies can be seen as; loss of visual acuity, visual field (VF) defects and optic disc changes. Typically, damage of the crossed nerve fibres which are originating from temporal hemiretina, results with bitemporal hemianopia in the visual field test [4]. Routine screening of VF by automated perimetry is essential [5]. But the prevalence of VF defects in pituitary adenoma varies between 9 and 32% [6].
Optical coherence tomography (OCT) is a device that helps taking cross-sectional images of the retinal structure and quantifying the thickness of the macula layers noninvasively [7]. The macular ganglion cell complex (GCC) composes of the nerve fibre layer, the ganglion cell layer (GCL), and the inner plexiform layer (IPL) [8]. OCT can detect thinned macular GCC and retina nerve fibre layer (RNFL) which could be related with both optic neuropathies and chiasmal compression [7]. The new segmentation software designed for the spectral domain-OCT (SD-OCT) enables the independent quantification of all the retinal layers. The macular RNFL (mRNFL), macular ganglion cell layer (mGCL), and macular interplexiform layer (mIPL) can be measured separately. These three layers are the most affected by optic neuropathies. Previous studies have shown assessment of the optic nerve and macula thicknesses have been performed in patients with chiasmal compression [1, 2].
The purpose of this study is to evaluate macula, RNFL, mGCL, mIPL and macular nerve fibre layer (mNFL) thicknesses in patients with pituitary tumours who has normal VF. We researched whether OCT analysis could be used in neuro-ophthalmology units before VF defects developed.
Materials and methods
Declaration of Helsinki Principles were used, informed consent was confirmed by all participants and was approved by the Ethics Committee of Ankara Training and Researching Hospital. This study is a retrospective study. The consecutive patients with recently established diagnosis of pituitary tumours which had evidence with chiasm impingement at pituitary magnetic resonance images (MRI) with normal VF and who were consulted for neuro-ophthalmological examination before treatment at the Department of Ophthalmology of Ankara Training and Researching Hospital between 2016 and 2019 were enroled. Thirty-five eyes of 35 patients with pituitary tumours who had normal VF, underwent a complete ophthalmic examination. Best corrected visual acuity (BCVA) with LogMAR chart, slit lamp biomicroscopy, intraocular pressure (IOP) measurements with Goldmann applanation tonometer, dilated stereoscopic fundus examination, VF test and SD-OCT were examined.
The main inclusion criteria of the patients with pituitary tumour was evidence with chiasm impingement at pituitary MRI regardless of being macroadenoma or microadenoma. Subjects were excluded if they had myopia >6 diopters; a history of ocular surgery, any anterior segment, retinal, posterior segment or optic nerve disease other than compressive optic neuropathy, any previous radiotherapy or medical treatment because of pituitary adenoma, and if they had a history of diabetic or any other systemic diseases.
Forty-one eyes of 41-healthy participants without pituitary adenoma and with a normal ophthalmic examination were enroled as control group in the study. The inclusion criteria of normal individuals were; age >18 years, spherical refraction between +3.00 and −6.00 diopters, cylinder refraction within ±3.00 diopters and an IOP of <20 mm Hg. Exclusion criteria included history of ocular surgery, any anterior and posterior segment disease or optic nerve disease, including known glaucoma or optic nerve disease other than compressive optic neuropathy and a history of diabetic or any other systemic diseases.
The SD-OCT (Spectralis, Heidelberg, Germany; software version 6.0) was used to measure macular and optic disc parameters. All subjects were examined using the standard macula protocol of the OCT. Images had to have a quality index of at least 20 to be included in the study. The new software for the Spectralis OCT can perform layer-by-layer segmentation that includes: total retinal thickness, inner retinal layers, mRNFL, mGCL, mIPL, macular inner nuclear layer, macular outer plexiform layer, macular outer nuclear layer, photoreceptors, and retina pigment epithelium. The three layers in these nine zones were used in this study; mGCL, mIPL and mRNFL.
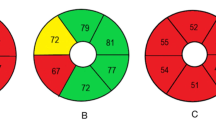
Early Treatment Diabetic Retinopathy Study (ETDRS) circle is the retinal thickness map analysis of the different layers for each of seven areas (Fig. 1). The circle consists of three rings; 1-mm (central), 3-mm (inner), and 6-mm (outer) diameter at the fovea. The inner and outer rings were then divided into four zones: superior, nasal, inferior, and temporal. Global macular volume for each layer also was recorded.
Early Treatment Diabetic Retinopathy Study (ETDRS) circle is the retinal thickness map analysis of the different layers for each of seven areas. The circle consists of three rings; 1-mm, 3-mm, and 6-mm diameter at the fovea. The inner and outer rings were then divided into four zones: superior, nasal, inferior, and temporal. Global macular volume for each layer also was recorded. Layer-by-layer segmentation was done automatically by using the new software for the Spectralis OCT. The following macular measurements were described; inner retinal layers, mRNFL, mGCL, mIPL, macular inner nuclear layer, macular outer plexiform layer, macular outer nuclear layer, photoreceptors, and retina pigment epithelium.
VF was performed using a Humphrey HFA II 750 automated field analyser (Humphrey-Zeiss Instruments, Dublin, CA). The 30-2 Swedish interactive threshold algorithm program was used. The VF reliability criteria included <20% fixation loss and <20% false negative and false positive rates. Perimetry was performed within 1 week of clinical examination and OCT measurements.
Patients were required to have a normal VFs result depending on absence of a temporal VF defect. Normal VF defined as none a cluster of three points with a probability <5% on the pattern deviation map, including at least one point with a probability of <1% or a cluster of two points with a probability of <1% with respect to the vertical meridian. All patients with a definite vertically demarcated temporal field loss in either eye on the pattern deviation map in VF were excluded.
Statistical analyses
Data analyses were performed by using SPSS for Windows, version 22.0 (SPSS Inc., Chicago, IL, United States). The distribution of continuous variables were determined by Kolmogorov Smirnov test. Levene test was used for the evaluation of homogeneity of variances. Continuous data were described as mean ± SD. Categorical data were described as number of cases (%). While the differences in normally distributed variables among more than two independent groups were analysed by one-way ANOVA. On the other hand, Kruskal Wallis test was applied for comparisons of the not normally data. When the p-value from one-way ANOVA or Kruskal Wallis test statistics were statistically significant, post hoc LSD or Conover’s non-parametric multiple comparison test were used to know which group differs from others. It was evaluated degrees of relation between variables with pearson correlation or spearman correlation analysis. p-value < 0.05 was accepted as significant level on all statistical analysis.
Results
A total of 76 eyes of 76 participants divided in two groups. Thirty-five subjects in pituitary tumour group and 41 subjects in control group were analysed. The mean age of pituitary tumour group was 39.9 ± 12.7 years and normal group was 32.98 ± 7.41 years. BCVA, IOP were similar in patient and control groups. The general characteristics of subjects are shown in Table 1.
Average of the total macula thickness of inner temporal (p: 0.006), outer temporal (p < 0.001), inner nasal (p: 0.03) and outer nasal (<0.001) thickness were significantly lower in pituitary tumour group than normal group. Average of RNFL (p: 0.009), temporal (p: 0.001), superiotemporal (p:0.004) and inferiotemporal (p: 0.01) were significantly lower in pituitary tumour group than normal group. Average of central GCL (p: 0.01) and central NFL (p:0.03) were significantly lower in pituitary tumour group than normal group. There was no statistically significant difference between the two groups in IPL averages.
Macular segmentation, optic disc and macular thickness analysis were summarized in Tables 2 and 3.
Discussion
The GCL accounts for up to 40% of the thickness in the macular area. The macular thickness can point to possible ganglion cell loss. These structures that could be measured by OCT has been accepted as useful diagnostic value for chiasmal damage [7]. In previous studies, patients with chiasmal compression showed significant thinning of the retinal thickness on the nasal macular area, which were associated with the severity of VF damage [9, 10]. The thickness of nasal hemi-retina in these patients predominantly depends on damaging of the crossed fibres. Our study demonstrated that the temporal macular thickness was significantly lower as well as the nasal macular thickness in pituitary tumour group before VF defect occurs. The macular thickness measurements may be used as an indicator of neuronal loss and could clinically prove the damage caused by pituitary tumour.
Monterio et al. [11] reported that average RNFL thickness is the most frequently abnormal parameter in eyes with band atrophy (BA) caused by chiasmal compression. The other studies also have demonstrated that temporal sides of RNFL thickness reduction is correlated with bitemporal hemianopia defect [10, 12, 13]. Danesh-Meyer et al. suggested that patients with RNFL thinning had more severe VF defects even they had good visual acuity. And they suggested RNFL measurement was the prespecified marker for axonal loss in chiasmal compression [14, 15]. Our results also suggest that total and temporal side of RNFL were significantly lower in patients with pituitary tumour even if they had normal VF. This findings confirm the anatomical architecture of the crossing nerve fibres in human eyes.
GCC parameters is useful in evaluating structural damage in patients with chiasmal compression [4, 14]. Akashi et al. [8] demonstrated that the inner macular parameters in the nasal hemiretina had significantly higher diagnostic ability to detect BA in chiasmal compression. Tan et al. [6] also suggested that the GCC map could be correlated with VF defects. Also, in another study, 75% of 12 eyes with temporal VF depression had significant decrease in GCC thickness, predominantly in the nasal hemi-retina [14]. Those studies included pituitary tumour patients with temporal hemianopsia. But also, there are recently published studies which demonstrate thinning of inner retina layers with normal VF in pituitary tumours. Zhang et al. [16] found thinner GCL in pituitary non-functional adenoma with chiasm compression patients without VF defect. Likewise, Tieger et al. [17] studied twenty-three patients with chiasmal compression, six patients had no VF defect and these patients showed statistically significant loss of GCC compared with control group. Blanch et al. studied with seven sellar tumour patients with normal visual function but no evidence of compressive chiasmopathy in MRI. They suggested that GCC analysis is more sensitive than VF testing with standard automated perimetry in the detection of compressive chiasmopathy or optic neuropathy [2]. In Lee et al. study [18], eyes with chiasmal compression showed thinning of the macular RNFL, GCL, IPL in patients with partial to no recovery of VF after tumour excision. In another study, 12 pituitary adenoma patients who had optic chiasmal compression without VF defect, had found significantly thinner mGCIPL in the superior, superonasal, inferonasal, and inferior sectors [19]. Similar to these studies, we found central mGCL and central mNFL thicknesses were significantly lower in pituitary tumour patients who had normal VF test. Our results suggest that mGCL and mNFL may be useful for early detection of optic neuropathy caused by pituitary tumours.
In conclusion, patients with pituitary tumour had thinner nasal and temporal macula, temporal RNFL, central mGCL and mNFL layers before VF defects developed. In addition, these results may be accepted to be showing that OCT is clinically useful for detecting damage of optic nerve when VF testing is unreliable.
Thus, we may say that nasal macular, temporal RNFL, central mGCL and mNFL measurements can be used as a diagnostic test for patients with pituitary tumours. However, inevitably both VF and OCT examinations remain important at detecting damage due to pituitary tumours.
Summary
What was known before
-
Pituitary tumours cause thinner ganglion cell complex, retina nerve fibre layer, macula
What this study adds
-
Retina nerve fibre layer, ganglion cell layer and macular nerve fibre layer can be thinner in pituitary adenoma with normal visual field.
-
These parameters may be diagnostic value for pituitary adenoma, especially visual field test is unreliable.
References
Cennamo G, Auriemma RS, Cardone D, Grasso LFS, Velotti N, Simeoli C, et al. Evaluation of the retinal nerve fibre layer and ganglion cell complex thickness in pituitary macroadenomas without optic chiasmal compression. Eye. 2015;29:797–802.
Blanch RJ, Micieli JA, Oyesiku NM, Newman NJ, Biousse V. Optical coherence tomography retinal ganglion cell complex analysis for the detection of early chiasmal compression. Pituitary. 2018;21:515–23.
Mete O, Asa SL. Clinicopathological correlations in pituitary adenomas. Brain Pathol. 2012;22:443–53.
Lee JP, Park IW, Chung YS. The volume of tumor mass and visual field defect in patients with pituitary macroadenoma. Korean J Ophthalmol. 2011;25:37–41.
Moon CH, Hwang SC, Ohn YH, Park TK. The time course of visual field recovery and changes of retinal ganglion cells after optic chiasmal decompression. Invest Ophthalmol Vis Sci. 2011;52:7966–73.
Tan O, Chopra V, Lu AT, Schuman JS, Ishikawa H, Wollstein G, et al. Detection of macular ganglion cell loss in glaucoma by Fourier-domain optical coherence tomography. Ophthalmology. 2009;116:2305–14.
Gnanalingham KK, Bhattacharjee S, Pennington R, Ng J, Mendoza N. The time course of visual field recovery following transphenoidal surgery for course of visual field recovery following transphenoidal surgery for pituitary adenomas: predictive factors for a good outcome. J Neurol Neurosurg Psychiatry. 2005;76:415–9.
Akashi A, Kanamori A, Ueda K, Matsumoto Y, Yamada Y, Nakamura M. The detection of macular analysis by SD-OCT for optic chiasmal compression neuropathy and nasotemporal overlap. Invest Ophthalmol Vis Sci. 2014;55:4667–72.
Moura FC, Medeiros FA, Monteiro ML. Evaluation of macular thickness measurements for detection of band atrophy of the optic nerve using optical coherence tomography. Ophthalmology. 2007;114:175–81.
Monteiro ML, Costa-Cunha LV, Cunha LP, Malta RF. Correlation between macular and retinal nerve fibre layer Fourier-domain OCT measurements and visual field loss in chiasmal compression. Eye. 2010;24:1382–90.
Monterio ML, Moura FC, Medeiros FA. Diagnostic ability of optical coherence tomography with a normative database to detect band atrophy of the optic nerve. Am J Ophthalmol. 2007;143:896–9.
Kanamori A, Nakamura M, Matsui N, Nagai A, Nakanishi Y, Kusuhara S, et al. Optical coherence tomography detects characteristic retinal nerve fiber layer thickness corresponding to band atrophy of the optic discs. Ophthalmology. 2004;111:2278–83.
Ohkubo, et al. Relationship between macular ganglion cell complex parameters and visual field parameters after tumor resection in chiasmal compression. Jpn J Ophthalmol. 2012;56:68–75.
Danesh-Meyer HV, Papchenko T, Savino PJ, Law A, Evans J, Gamble GD. In vivo retinal nerve fiber layer thickness measured by optical coherence tomography predicts visual recovery after surgery for parachiasmal tumors. Invest Ophthalmol Vis Sci. 2008;49:1879–85.
Danesh-Meyer HV, Wong A, Papchenko T, Matheos K, Stylli S, Nichols A, et al. Optical coherence tomography predicts visual outcome for pituitary tumors. J Clin Neurosci. 2015;22:1098–104.
Zhang X, Ma J, Wang YH, Gan LY, Li L, Wang XQ, et al. The correlation of ganglion cell layer thickness with visual field defect in non-functional pituitary adenoma with optic chiasm. Zhonghua Yan Ke Za Zhi. 2019;55:186–94.
Tieger MG, Hedges TR 3rd, Ho J, Erlich-Malona NK, Vuong LN, Athappilly GK, et al. Ganglion cell complex loss in chiasmal compression by brain tumors. J Neuroophthalmol. 2017;37:7–12.
Lee GI, Park KA, Son G, Kong DS, Oh SY. Optical coherence tomography analysis of inner and outer retinal layers in eyes with chiasmal compression caused by suprasellar tumours. Acta Ophthalmol. 2019. https://doi.org/10.1111/aos.14271.
Yum HR, Park SH, Park HY, Shin SY. Macular ganglion cell analysis determined by cirrus HD optical coherence tomography for early detecting chiasmal compression. PLoS ONE 2016;11:e0153064.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Orman, G., Sungur, G. & Culha, C. Assessment of inner retina layers thickness values in eyes with pituitary tumours before visual field defects occur. Eye 35, 1159–1164 (2021). https://doi.org/10.1038/s41433-020-1032-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1032-8