Abstract
Background/Objectives
To evaluate the outcomes of orbital evisceration with primary implant placement in acutely infected/inflamed eyes, using implant exposure/extrusion as a surrogate of success. To contextualise this with previously published literature.
Subjects/Methods
A retrospective case series of all patients with acutely infected/inflamed eyes undergoing urgent orbital evisceration with primary implants, at a British tertiary centre between January 2006 and August 2018. A systematic literature review of orbital eviscerations with primary implant placement in acute endophthalmitis/infection and recent trauma.
Results
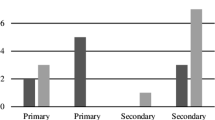
Twenty-six eyes were eviscerated in the context of acute infection/inflammation. Twenty-four eyes had primary orbital implants. Indications for evisceration included endophthalmitis (18/26, 69%), microbial keratitis with corneal perforation (4/26, 15%), non-infectious corneal perforation (3/26, 12%), and recent trauma (1/26, 4.8%). The implants used were acrylic (15/24, 63%), MEDPOR (5/24, 21%), and silicone (4/24, 17%). The follow-up period was 15 months to 14 years. Implant exposure occurred in two (8.3%), managed with implant exchange and scleral reformation in one, and implant removal with dermis fat grafting in the other. One patient (4.2%) had conjunctival wound dehiscence with spontaneous healing. Six (25%) required further surgery for minor complications as follows: conjunctival prolapse, upper lid ptosis with slight sulcus loss, lower lid entropion with shortened fornix, and lower lid ectropion. The systematic literature review showed that the mean rate of orbital implant exposure/extrusion in this subset of patients was 7.8% (95% CI: 2.7%, 12.9%, SD 8.0%), range 0–27%.
Conclusions
In acutely infected/inflamed eyes, the implant exposure/extrusion rate following orbital evisceration with primary implant placement is acceptable.
Similar content being viewed by others
Introduction
Orbital evisceration involves removal of the contents of the globe but leaving the sclera and adnexal tissues intact. It is commonly used to treat ‘painful blind eye’, occurring due to a number of underlying causes such as previous ocular trauma, chronic glaucoma, chronic ocular inflammation, retinal ischaemia, and previous ocular infection. It is generally accepted that evisceration provides better prosthetic motility, cosmesis, and long-term implant stability than does enucleation [1, 2]. Intraocular malignancy is an absolute contraindication to evisceration.
Orbital evisceration is also used to treat endophthalmitis, which is where the controversy lies. Prior to the advent of modern antibiotics, evisceration was preferred to enucleation for endophthalmitis due to the risk of subarachnoid spread of intraocular infection [3]. Its popularity declined following reports of sympathetic ophthalmia [4, 5]. Subsequent studies showed that the incidence of sympathetic ophthalmia is extremely rare. Du Toit et al. reported that in those with penetrating ocular injuries, none of the cases who underwent surgical treatment, including 491 of those treated with evisceration, experienced sympathetic ophthalmia, but that two (0.14%) cases occurred in those patients who had not undergone any ocular surgery [6]. They were limited by a short duration of follow-up (2 weeks to 1 year) [6]. Gürdal et al. reported that none of their 217 patients with penetrating ocular injuries who were treated with evisceration or enucleation were found to have sympathetic ophthalmia, following a mean follow-up period of 10.3 ± 6.6 years. The British Ophthalmological Surveillance Unit prospective study of sympathetic ophthalmia found an incidence of 0.03/100 000 of the general UK population [7]. Ocular surgery (mainly vitreoretinal) was the most common initiating injury, rather than penetrating ocular injury [7]. Modern treatment allowed good visual outcomes, i.e., all patients improved or maintained their visual acuity at 1 year following diagnosis, and 75% obtained a 1-year visual acuity of 6/12 or better [7].
The reported rates of implant exposure following evisceration for all causes are estimated to be between 0 and 67% [8]. Traditionally, the use of primary orbital implants following evisceration for endophthalmitis was discouraged in order to delay primary closure and reduce the risk of implant extrusion [9, 10]. Previous studies have shown this can safely be done [11,12,13]. Proponents of placing primary implants in these cases argue that the worst-case scenario is that the implant requires removal due to exposure/extrusion or to treat a post-operative orbital abscess, but not placing a primary implant is likely to necessitate a second operation [13]. Despite these results [11,12,13], a UK national survey showed that only 43% of respondents would place an orbital implant in those whose eyes were removed for endophthalmitis, and of those, only 50% were placed as primary implants [14].
In our unit, we employ urgent orbital evisceration with primary implants for progressing endophthalmitis, irreparable corneal perforation or following trauma where the globe has been irreparably damaged and has become acutely inflamed. We wished to evaluate the outcomes and assess the safety and tolerability of this procedure for this specific set of patients. We also wished to better understand the implant exposure rates reported in the literature for this specific set of patients.
Materials and methods
This was a retrospective consecutive case series. All patients who underwent orbital evisceration at the Royal Hallamshire Hospital, Sheffield, United Kingdom between January 2006 and August 2018 inclusive were identified by searching in Operating Room Management Information System, an electronic record system, for ‘evisceration’ procedures carried out by the two Oculoplastic Consultants in our unit. Case notes for the patients on this list were reviewed by the lead author (SJC), to identify only those eviscerations that were done in an acute setting, according to the criteria described above. Only these ‘emergency eviscerations’ were included. Equivocal cases were discussed amongst the three authors to reach a consensus.
The primary objective was the rate of orbital implant exposure in these emergency eviscerations. Secondary objectives included the rates of post-operative wound dehiscence and the need for further surgery. Demographic data were collected, including age, gender, smoking status, and presence of immunosuppression. Surgical and implant data, indication for evisceration and implant, and the use of systemic antibiotics were also examined. Descriptive statistics and Fisher’s exact test were performed using GraphPad Software QuickCalcs [15].
Surgical method
The surgical method for evisceration is described as follows. A 360o peritomy was performed. The cornea was removed by 360o keratectomy. The intraocular contents were removed with a metal scoop and sent for histological analysis. The uveal tissue was mechanically debrided with a cotton bud and any remaining traces were suctioned with a Fine Frazier Suction 6fgN140 cannula (Pelican Feminine Healthcare Ltd trading as Single Use Surgical, Cardiff, UK). We do not routinely apply absolute alcohol and topical antibiotics into the surgical field. The sclera was divided into two flaps, extending superotemporally to inferonasally reaching the optic nerve, which was islandised completely. Cautery was applied for haemostasis, if required. The orbital implant was passed into the socket using a ‘no touch’ technique to ensure sterility. When placing the implant into the socket, care was taken to prevent posterior tissue drag, by putting anterior traction to hold the scleral flaps upwards out of the socket. Closure was done in either two layers (sclera and Tenon’s capsule as one layer with 5/0 Vicryl and conjunctiva as a separate layer with 7/0 Vicryl) or in three layers (sclera with 5/0 Vicryl, Tenon’s capsule with 6/0 Vicryl, and conjunctiva with 7/0 Vicryl), depending on the operating surgeon. A conformer (Stryker, Kalamazoo, Michigan, USA) was placed in all. All received topical chloramphenicol ointment before JELONET paraffin gauze (Smith & Nephew, Watford, UK) and a pressure dressing was applied. Systemic antibiotics were used in select cases. Sutures were all ETHICON, Inc. (Cincinnati, Ohio, USA), 5/0 Vicryl W9442, 6/0 Vicryl W9760, 7/0 Vicryl W9561.
Literature review
Many studies examining orbital evisceration do not examine evisceration solely in the context of infection, endophthalmitis, or an acutely inflamed eye. Many studies also report the outcomes of eye removal surgery by combining the results for enucleation and evisceration together. In order to contextualise the results of our series, we performed a literature review to elucidate the reported figures for evisceration performed in the setting of an acutely infected or inflamed eye.
We searched MEDLINE as follows: ‘((eye evisceration) OR (orbit evisceration)) AND (endophthalmitis)’ and ‘((eye evisceration) OR (orbit evisceration)) AND (‘Eye Injuries/surgery’[MAJR])’. ‘Eye evisceration’, ‘orbit evisceration’, and ‘endophthalmitis’ were MeSH terms. ‘Eye injuries/surgery’ was a MeSH major topic. ‘Eye’, ‘evisceration’, ‘orbit’, ‘endophthalmitis’, and ‘endophthalmitides’ were searched in all fields. Abstracts were reviewed to identify the relevant papers, which were then considered in detail. Reference lists of those papers and of relevant reviews were checked to identify any other relevant papers that had not already been identified.
Studies describing results of evisceration in the setting of an acutely infected or inflamed eye (e.g., keratitis, endophthalmitis, recent trauma) with a primary implant placed at the time of evisceration were included. Non-English articles and articles published before the year 1990 were excluded. Studies where there was no separation of the results for enucleation and evisceration were excluded. Studies where it was not possible to distinguish eviscerations that had been done in the setting of an acutely infected (e.g., endophthalmitis, keratitis) or acutely inflamed (e.g., recent trauma) eye were excluded. That is, if results were reported as combined with other indications for evisceration (e.g., painful blind eye), these studies were excluded. Studies where primary implants were not placed at the time of evisceration surgery were excluded.
Results
There were 26 eyes (26 patients) who received eviscerations in the context of an acutely infected or inflamed eye. All were planned to have a primary implant, but in two, the decision not to place an orbital implant was made intra-operatively due to the extent of infection. The operations were performed by the named Oculoplastic Consultants and Oculoplastic Fellows. The follow-up period was 15 months to 14 years. Patient characteristics are summarised in Table 1.
Details regarding the underlying aetiology, implants, complications, and further surgery are summarised in Table 2. The majority of cases were due to endophthalmitis (18/26, 69%). Most of these (16/18, 89%) were associated with corneal perforation and microbial keratitis. Of the remaining two endophthalmitis cases, one was secondary to blebitis. The other patient had suffered a globe rupture and re-presented 5 months after primary repair with pus coming from the wound. The decision was made to eviscerate the eye due to endophthalmitis, high risk of perforation, and limited visual potential. In 1 of the 16 endophthalmitis cases associated with microbial keratitis and corneal perforation, there was some clinical suspicion that the endophthalmitis could have come from a co-existing sinus infection rather than from the keratitis. Endophthalmitis was defined either clinically (e.g., evidence of hypopyon or vitritis) or histologically. Unless there was clear evidence clinically or histologically that corneal perforation resulted from a non-infectious process, corneal perforation without endophthalmitis was classed as infectious. Non-infectious corneal perforation (3/26, 12%) was due to corneal melt (1/26, 3.8%), corneal decompensation and bullous keratopathy (1/26, 3.8%), and corneal perforation in a failed corneal graft without any clinical, laboratory, and histological evidence of infection (1/26, 3.8%). There was one (3.8%) globe rupture case where evisceration was done 9 days after primary repair, as the eye was unsalvageable, and the patient was in intractable pain. Histology confirmed the clinical diagnoses. There were no cases of malignancy and no cases of sympathetic ophthalmia identified.
There were 15/24 (63%) acrylic implants (John Weiss International, Harlow, UK), 5/24 (21%) porous polyethylene (MEDPOR) implants (Stryker), and 4/24 (17%) silicone implants (FCI Ophthalmics, Pembroke, Massachusetts, USA). We collected data on the use of pre-operative, intra-operative, and post-operative systemic antibiotics, but there was no pattern identified. It appeared to be dependent on surgeon preference and the case at hand.
Implant exposure occurred in 2/24 (8.3%), both with non-porous primary implants (silicone, acrylic), labelled Patients 7 and 21 in Table 2. The indication for both cases was endophthalmitis with corneal perforation and microbial keratitis. Both patients had a history of smoking, though one had quit for 16 months prior to evisceration. Patient 21 had two-layer closure, and we presume Patient 7 also had two-layer closure based on the closure method recorded in another patient operated on by the same surgeon. There were no other common features between the two cases.
The silicone implant case (Patient 7) was treated with implant exchange for a smaller 16-mm silicone implant following scleral reformation. This patient subsequently required Coleman fat grafting to increase the socket volume, as there was upper sulcus loss with inferior implant migration. Following this, the lower lid was found to be low, which was corrected with lateral tarsal strip surgery. The acrylic implant case (Patient 21) was treated with implant removal and replacement with a dermis fat graft. This patient then subsequently required trim of a devitalised exposed area of the graft and tarsorrhaphy, and there were no further problems following this.
We did not find any significant association between implant exposure and the following variables by Fisher’s exact test: porous versus non-porous implant (p = 1.00), smoking ever versus never smoked (p = 0.4783), presence of endophthalmitis versus microbial keratitis without endophthalmitis or non-infectious causes (p = 0.5109), and presence of immunosuppression (p = 0.4831). The main difference in surgical technique was whether there was two-layer or three-layer closure, but this was not found to be significant with Fisher’s exact test for conjunctival prolapse/dehiscence and implant exposure (p = 0.3521) or for implant exposure alone (p = 0.5362).
The majority of patients did not require any further surgery (18/26, 69%). The two patients who did not receive a primary orbital implant did not receive a secondary implant. In one, this was because of an inability to retain a ring conformer post-operatively. The reason was not documented for the other patient. Aside from the two patients with implant exposure, further surgery was required in six other patients for minor reasons as follows: conjunctival prolapse, lower lid ectropion, lower lid entropion with shortened fornix, and upper lid ptosis with slight sulcus loss (see Table 2 for more details). There was one case of conjunctival wound dehiscence, which had healed on its own by the time of planned surgical repair.
Results of the literature review
The literature search yielded 277 abstracts (233 endophthalmitis, 44 trauma). The studies meeting the inclusion criteria are shown in Table 3. To facilitate direct comparison with our study, only the eyes that were eviscerated in the setting of acute infection (e.g., endophthalmitis, keratitis) and acute inflammation (e.g., recent trauma) with primary orbital implants were included in Table 3. Exposure/extrusion rates were calculated based on this.
In two series, there was one case in each where primary implant removal was required in order to resolve a post-operative (3 weeks) orbital abscess [13, 16]. These cases were included as implant extrusion. From these studies, the mean rate of orbital implant exposure/extrusion in this subset of patients was 7.8% (95% CI: 2.7%, 12.9%, SD 8.0%), range 0–27%.
Discussion
Treating acutely infected/inflamed eyes with orbital evisceration and primary implant is relatively uncommon. In 12 years, we had 26 cases requiring urgent evisceration. Twenty-four of those received primary implants. Our rate of implant exposure was 8.3%, which is well within the range of what has been reported, though it is marginally higher than the mean implant exposure/extrusion rate we found with our literature search of 7.8% (Table 3). Four of the 12 studies in Table 3 reported exposure rates of 0% [17,18,19]. In three of these studies, the number of cases was much smaller than in ours, with the number of eligible cases less than ten (Table 3) [17,18,19]. In two of those studies, the follow-up time was less than 1 year (Table 3), so the implant exposure/extrusion rates may have been underreported [18, 19]. It has previously been reported that the usual time for implant extrusion to occur following evisceration is between 2 and 10 years [20]. Other studies have supported that longer follow-up is required to detect implant exposure and extrusion, with reporting mean times to exposure/extrusion following eviscerations of 14 months (range 1–60 months) [21], 22.5 months (range 6 weeks to 4 years) [22], 20.8 months (range 11–36 months) [23], and as late as 52 ± 53.4 months for unpegged implants and 70.2 ± 54.5 months for pegged implants [24].
The prospective cohort series by Liu was comparable to our series in terms of the number of cases included [17]. He reported no cases of implant exposure/extrusion with a mean follow-up time of 43.7 months [17]. He attributed this mainly to his surgical technique and after care procedures, namely removal of contaminated instruments from the surgical field, changing gloves intra-operatively, and waiting for a minimum of 6 weeks before fitting an artificial eye. We also maintained sterility of the implant by utilising a ‘no touch’ technique, and artificial eye fitting for our patients does not routinely occur until at least 6 weeks post-operatively. Liu also cited using larger implant sizes with a mean of 18.3 versus 13.7 mm, when compared to the retrospective case series done in the same unit [17]. In our study, the mean implant size was 19.3 mm, though the exposures occurred in the patients with 18 mm implants. In our literature review, the median size of the implants in which exposures occurred was 18 mm [11,12,13, 16,17,18,19, 25,26,27]. Other differences between our study and Liu’s were that Liu used absolute alcohol and topical gentamicin in the surgical field intra-operatively [17]. The use of absolute alcohol is controversial, as proponents believe it destroys residual uveal tissue and microbes [8, 17, 18], but opponents believe it causes more tissue inflammation and necrosis, which could predispose to implant extrusion [28, 29].
Interestingly, there were two other series from the same unit as Liu’s prospective cohort study, but with vastly different exposure/extrusion rates. One was a retrospective series of the outcomes from Liu’s colleagues reported by Liu with an exposure/extrusion rate of 27% [17]. The other was a retrospective series done subsequently by different authors, Chaudhry et al., with an exposure/extrusion rate of 8.3% [26]. In the series of other surgeons described by Liu, there were no posterior sclerotomies used, a mean implant size of 13.7 mm, and a presumed lack of maintaining sterility of the implants [17]. But in Chaudhry’s series, there was no description of surgical method, and their mean implant size was 18 mm [26]. Of the three studies, Liu’s own prospective series was the smallest, and the vastly varied extrusion rates from one single unit suggests that perhaps a larger sample size was required to detect a true effect. Indeed, removing the outlier exposure/extrusion rates from our literature review gives a mean exposure/extrusion rate of 8.9% (95% CI: 4.9%, 12.8%, SD 4.30).
In our series, we did not find any significant association between implant exposure and the presence of endophthalmitis, a history of smoking, type of implant used, or closure technique. This may have been due to a small sample size. Regarding type of implant, Gupta et al. attempted to identify risk factors associated with implant exposure after eviscerations, and found that there was a slight tendency towards implant exposure with infection, a phthisical eye, previous multiple surgeries, and use of a porous implant, but that none of these factors was significantly associated with implant exposure [8]. Custer and Trinkhaus found in pooled data that the rates of exposure in eviscerations were slightly lower in non-porous (4.8%) than in porous (6.6%) implants, but there was no comment as to whether this was a significant difference [30]. Verhoex et al. found that closure technique was not significantly associated with implant exposure, though their technique was slightly different to ours in that they differentiated between closing Tenon’s capsule and conjunctiva together as one layer versus closing them individually in two layers [31], whereas we closed Tenon’s capsule with the sclera and the conjunctiva separately in two layers versus closing Tenon’s capsule, sclera, and conjunctiva separately in three layers.
Surgeon inexperience is another factor that has been speculated to increase the risk of implant exposure. In a study combining the outcomes of enucleation and evisceration, cases performed by the surgeon with a special interest in Orbit and Oculoplastics had an implant exposure rate of 4.5% (1/22) whereas those performed by surgeons with other areas of special interest had an implant exposure rate of 44% (7/16) [21]. Not only was the area of expertise relevant, but also the seniority of the surgeon, as 63% (5/8) of the implant exposures in their series occurred in cases where the surgery was not performed by the senior (Consultant) surgeon, and 60% (3/5) of those were done by surgeons who were not supervised by the senior surgeon [21]. Similarly, in Liu’s prospective study with no implant exposures detected, he reported that even with the procedures performed by residents or fellows under his supervision did not result in implant exposure [17]. However, in our study, the named principal surgeons for the two cases of implant exposure were one each of an Oculoplastic Fellow and of an Oculoplastic Consultant, which suggests that other factors beyond surgeon experience could be involved.
This was a retrospective study, and therefore there were inherent limitations in our study. This resulted in variable follow-up times; however, the most recent patient in our series had at least a 15-month follow-up. It is possible that patients may have presented to their local unit for minor problems and our unit was not subsequently informed. That said, due to the way the service is set up in our area, patients presenting to a local unit with socket problems, including suspected or confirmed implant exposure, are usually referred back to our unit for assessment and management. The exception would be if the patient had moved completely out of our area and a different tertiary centre was geographically closer to them. Fortunately, there were minimal missing data, and this was mainly with regard to pre-operative culture results, which were not available in three of the infected cases. Systemic antibiotic use was quite varied, so we could not perform any meaningful analysis.
Performing emergency orbital evisceration with primary orbital implantation is relatively uncommon, as shown by the small numbers in our series and in the majority of those reported in our literature review (Table 3). Future studies may include meta-analysis or multi-centre initiatives to increase statistical power. Our implant exposure rate was 2/24 (8.3%). Based on our literature review, this was in the lower end of the quoted rates (0–27%) and closely matched the mean rate of 7.8% (SD 8.0%) [11,12,13, 16,17,18,19, 25,26,27]. We had one case (4.2%) of conjunctival wound dehiscence, which did not require surgical intervention. Cosmetic results were acceptable by most. We would strongly advocate primary implant placement at the time of emergency evisceration. The implant exposure rate following primary orbital implantation is acceptable; and, with or without implant exposure, patients have good functional outcomes.
Summary
What was known before
-
Traditionally, the use of primary orbital implants following orbital evisceration for endophthalmitis was discouraged in order to reduce the risk of implant exposure and extrusion.
-
Previously published case series have shown that primary orbital implants can be safely placed in eyes eviscerated for endophthalmitis.
-
Despite this, the most recent UK national survey on the subject showed that only 21.6% (61/282) of eligible respondents (i.e., surgeons who perform eviscerations) placed a primary orbital implant following evisceration for endophthalmitis [14].
What this study adds
-
Our series confirmed that there are good functional outcomes and an acceptable implant exposure rate (8.3%) following orbital evisceration with primary implant placement in eyes with acute infection or following recent trauma.
-
Our systematic review identified that the mean rate of implant exposure/extrusion following evisceration in this specific set of patients was 7.8% (95% CI: 2.7%, 12.9%; SD 8.0%) with a range of 0–27%.
References
Timothy NH, Freilich DE, Linberg JV. Evisceration versus enucleation from the ocularist’s perspective. Ophthalmic Plast Reconstr Surg. 2003;19:417–20. discussion 20
Gürdal C, Erdener U, Irkeç M, Orhan M. Incidence of sympathetic ophthalmia after penetrating eye injury and choice of treatment. Ocul Immunol Inflamm. 2002;10:223–7.
Migliori ME. Enucleation versus evisceration. Curr Opin Ophthalmol. 2002;13:298–302.
Cytryn A, Perman K. Evisceration. In: Migliori M, editor. Enucleation, evisceration and exenteration of the eye. Boston: Butterworth-Heinemann; 1999. p. 105–12.
Green WR, Maumenee AE, Sanders TE, Smith ME. Sympathetic uveitis following evisceration. Trans Am Acad Ophthalmol Otolaryngol. 1972;76:625–44.
du Toit N, Motala MI, Richards J, Murray AD, Maitra S. The risk of sympathetic ophthalmia following evisceration for penetrating eye injuries at Groote Schuur Hospital. Br J Ophthalmol. 2008;92:61–3.
Kilmartin DJ, Dick AD, Forrester JV. Prospective surveillance of sympathetic ophthalmia in the UK and Republic of Ireland. Br J Ophthalmol. 2000;84:259–63.
Gupta R, Hari P, Khurana B, Kiran A. Risk factors for orbital implant exposure after evisceration: a case control study of 93 patients. Indian J Ophthalmol. 2019;67:1148–51.
Shore JW, Dieckert JP, Levine MR. Delayed primary wound closure. Use to prevent implant extrusion following evisceration for endophthalmitis. Arch Ophthalmol. 1988;106:1303–8.
Walter WL. Update on enucleation and evisceration surgery. Ophthalmic Plast Reconstr Surg. 1985;1:243–52.
Dresner SC, Karesh JW. Primary implant placement with evisceration in patients with endophthalmitis. Ophthalmology. 2000;107:1661–4.
Ozgur OR, Akcay L, Dogan OK. Primary implant placement with evisceration in patients with endophthalmitis. Am J Ophthalmol. 2007;143:902–4.
Tawfik HA, Budin H. Evisceration with primary implant placement in patients with endophthalmitis. Ophthalmology. 2007;114:1100–3.
Viswanathan P, Sagoo MS, Olver JM. UK national survey of enucleation, evisceration and orbital implant trends. Br J Ophthalmol. 2007;91:616–9.
Software G. GraphPad QuickCalcs: analyze continuous data. 2019. https://www.graphpad.com/quickcalcs/contMenu/.
Park YG, Paik JS, Yang SW. The results of evisceration with primary porous implant placement in patients with endophthalmitis. Korean J Ophthalmol. 2010;24:279–83.
Liu D. A comparison of implant extrusion rates and postoperative pain after evisceration with immediate or delayed implants and after enucleation with implants. Trans Am Ophthalmological Soc. 2005;103:568–91.
Tari AS, Malihi M, Kasaee A, Tabatabaie SZ, Hamzedust K, Musavi MF, et al. Enucleation with hydroxyapatite implantation versus evisceration plus scleral quadrisection and alloplastic implantation. Ophthalmic Plast Reconstructive Surg. 2009;25:130–3.
Zheng C, Wu AY. Enucleation versus evisceration in ocular trauma: a retrospective review and study of current literature. Orbit (Amst, Neth). 2013;32:356–61.
Zolli CL. Implant extrusion in eviscerations. Ann Ophthalmol. 1988;20:127–32.
McElnea EM, Ryan A, Fulcher T. Porous orbital implant exposure: the influence of surgical technique. Orbit. 2014;33:104–8.
Alwitry A, West S, King J, Foss AJ, Abercrombie LC. Long-term follow-up of porous polyethylene spherical implants after enucleation and evisceration. Ophthalmic Plast Reconstructive Surg. 2007;23:11–5.
Wang JK, Lai PC, Liao SL. Late exposure of the bioceramic orbital implant. Am J Ophthalmol. 2009;147:162–70.
Lin CW, Liao SL. Long-term complications of different porous orbital implants: a 21-year review. Br J Ophthalmol. 2017;101:681–5.
Ababneh OH, AboTaleb EA, Abu Ameerh MA, Yousef YA. Enucleation and evisceration at a tertiary care hospital in a developing country. BMC Ophthalmol. 2015;15:120.
Chaudhry IA, AlKuraya HS, Shamsi FA, Elzaridi E, Riley FC. Current indications and resultant complications of evisceration. Ophthalmic Epidemiol. 2007;14:97–3.
Tripathy D, Rath S. Evisceration with primary orbital implant in fulminant endophthalmitis/panophthalmitis. Orbit. 2015;34:279–83.
Berens C, Breakey AS. Evisceration utilizing an intrascleral implant. Br J Ophthalmol. 1960;44:665–71.
Hardy T, Rose G. Moorfields manual of ophthalmology. 2nd ed. London, UK: JP Medical Ltd; 2014. Jackson T, editor
Custer PL, Trinkaus KM. Porous implant exposure: Incidence, management, and morbidity. Ophthalmic Plast Reconstructive Surg. 2007;23:1–7.
Verhoekx JSN, Coolman AR, Tse WHW, Paridaens D. A single- versus double-layered closure technique in anophthalmic surgery. Ophthalmic Plast Reconstr Surg. 2017;33:329–33.
Acknowledgements
The authors acknowledge Dr Hardeep Singh Mudhar, Consultant Ophthalmic Pathologist, and Adam Meeney, Advanced Practitioner/Consultant Biomedical Scientist, for their work in providing histological analysis. The affiliation for both is: National Specialist Ophthalmic Pathology Service (NSOPS), Department of Histopathology, Royal Hallamshire Hospital, Sheffield, England, UK.
Author information
Authors and Affiliations
Contributions
SJC collected and analysed the study data, conducted the literature search, screened potentially eligible studies for the literature search, extracted and analysed the data from the literature search, updated reference lists, wrote the manuscript, and created the three tables included in this manuscript. JHYT contributed to the design of the study protocol, arbitrated potentially eligible study cases, and reviewed the manuscript. ZIC conceived the study idea and protocol, arbitrated potentially eligible study cases, and reviewed the manuscript. All authors had full access to the data in the study and final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chiu, S.J., Tan, J.H.Y. & Currie, Z.I. To implant or not to implant: emergency orbital eviscerations with primary orbital implants. Eye 35, 3077–3086 (2021). https://doi.org/10.1038/s41433-020-01382-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01382-0
This article is cited by
-
Surgical outcomes of orbital evisceration with primary orbital implant placement in patients with endophthalmitis
Eye (2023)
-
A Sandwich-Like Oral Mucosa Graft–Conjunctiva In Situ–Dermis-Fat Graft for Reconstruction of the Anophthalmic Socket with Ocular Infection History
Ophthalmology and Therapy (2022)