Abstract
Purpose
To compare the angle-to-angle (ATA) distance, and the repeatability and the reproducibility of these measurements among the three devices.
Methods
We performed the ATA measurements in 26 healthy subjects using anterior segment optical coherence tomography (CASIA2, Tomey, Japan), the Scheimpflug camera (Pentacam HR, Oculus, Wetzlar, Germany), and the combined Placido-ring corneal topography and Scheimpflug camera (TMS-5, Tomey). We also compared the repeatability and the reproducibility of the ATA measurements among these three devices.
Results
The ATA in the CASIA2 group was significantly larger than that in the Pentacam group (Bonferroni test, p = 0.002), or that in the TMS-5 group (p < 0.001). The coefficient variation of the first and second ATA measurements for a single examiner was 0.44% in the CASIA2 group, followed by 0.84% in the TMS-5 group, and 1.92% in the Pentacam group. The coefficient variation of the ATA measurements for two examiners was 0.61% in the CASIA2 group, followed by 0.97% in the TMS-5 group, and 1.84% in the Pentacam group.
Conclusions
The ATA distance measured with the CASIA2 was ~0.40 and 0.56 mm larger than that with the Pentacam and the TMS-5, respectively. The CASIA2 provided the highest repeatability and reproducibility of the ATA measurements, followed by the TMS-5, and the Pentacam. These three instruments cannot be used interchangeably in terms of ATA measurements.
Similar content being viewed by others
Introduction
The posterior chamber phakic intraocular lens (EVO Visian ICLTM; STAAR Surgical, Nidau, Switzerland) has provided good outcomes, in terms of long-term safety and efficacy [1,2,3]. However, there are ongoing concerns about the postoperative complications, such as intraocular pressure rise, corneal endothelial cell loss, cataract formation, and toric lens rotation [1, 4,5,6]. Actually, appropriate ICL size selection is crucial when considering safety issues, since a smaller ICL lens size selection may result in cataract formation and/or toric lens rotation, whereas a larger size selection may result in intraocular pressure rise and/or corneal endothelial cell damage.
Since the ICL is fixated to the ciliary sulcus, it is desirable to directly measure the sulcus-to-sulcus (STS) distance for selecting the proper ICL size [7]. Although we can directly obtain the STS by using ultrasound biomicroscopy, this measurement is invasive, time-consuming, and requires specific skills and experience. Therefore, it is still challenging to accurately determine or estimate the STS distance in daily practice. The manufacturer currently recommends to use the online calculation and ordering system, based on the biometry data of the white-to-white (WTW) distance and the anterior chamber depth. Considering that the correlation of the STS with the angle-to-angle (ATA) distance was much stronger than that with the WTW [8,9,10], ATA measurements may be clinically helpful for precisely estimating the STS and subsequently predicting the optimal ICL lens size. However, a comparison of the ATA measurements of commercially available devices has so far not been performed. Moreover, the repeatability or the reproducibility of ATA measurements has not been fully elucidated among these instruments. It may give us intrinsic insights into ATA measurements and subsequent optimal ICL lens size selection. The purpose of the present study is twofold; to compare the ATA distance, and to assess the repeatability and the reproducibility of the ATA measurements, among three devices in healthy subjects.
Material and methods
Study population
The study protocol was registered with the University Hospital Medical Information Network Clinical Trial Registry (000032314). We enrolled 26 eyes of 26 healthy subjects, who completed optical examinations at the Kitasato University Hospital for refractive surgery consultation, and who had no other ocular diseases, except for refractive errors. The sample size in this study offered 86.5% statistical power at the 5% level in order to detect a 0.50-mm difference in ATA measurements, when the standard deviation (SD) of the mean difference was 0.80 mm. All subjects gave informed consent before the study participation. The study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of the School of Allied Health Sciences of Kitasato University (2017-006).
Angle-to-angle measurements
The ATA distance was measured using three clinically available devices: a swept-source anterior segment optical coherence tomography device (CASIA2TM; Tomey, Nagoya, Japan), a rotating Scheimpflug camera (Pentacam HRTM; Oculus, Wetzlar, Germany), and a combined Placido-disk corneal topography with a Scheimpflug camera (TMS-5TM; Tomey, Nagoya, Japan). Only the right eye of each subject was selected for analysis. The ATA was determined as the horizontal distance between the angle recesses. This were automatically calculated by the CASIA2, and manually calculated by the Pentacam and TMS-5 (Fig. 1).
The CASIA2 is a swept-source anterior segment optical coherence tomography device that uses a wavelength of 1310 nm and measures with a speed of 50,000 axial scans per second. In the anterior segment mode, each 3D image consists of 128 B-scans (cross-sectional images) and 512 A-scans. The collected data are automatically processed by the system to achieve cross-sectional images with a width of 16 mm and a depth of 11 mm, which facilitate the analysis of the corneal shape, the anterior chamber, and the crystalline lens, within 0.3 s.
The Pentacam HR is a rotating Scheimpflug camera that captures 100 Scheimpflug images and obtains 138,000 elevation data points, which are processed to generate entire cross-sectional reconstructions of the anterior segment within 2 s.
The TMS-5 is a combined Placido-ring topographer and a rotating Scheimpflug camera that obtains data by merging Placido-ring topography (up to 7300 data points) and Scheimpflug tomography (up to 40,960 data points) within 2 s.
In each measurement, the patient’s chin was placed on the chin rest and the forehead against the forehead strap. The patient was asked to keep both eyes open and stare at the fixation target. After the image was focused and centered, the instruments automatically began obtaining the measurements. We checked image quality for each eye, and selected only one examination with a high quality factor.
Repeatability and reproducibility
The repeatability (within-examiner differences) and the reproducibility (between-examiner differences) among these instruments were assessed using a method described by Bland and Altman, whereby 95% of the differences or limits of agreement lie between ±1.96 × SD of the mean difference [11]. The measurements were performed by the two independent examiners who were experienced in the use of the instruments. Two readings were taken by the same examiner on each instrument. The sequence of measurements with the three instruments and the order in which examiners one and two took the measurements were randomized. The repeatability and the reproducibility of the ATA measurements was also evaluated by the coefficient of variation (CoV) as a normalized SD.
Statistical analysis
All statistical analyses were conducted using Microsoft Excel 2016 (Microsoft, Redmond, Washington, USA). The Bonferroni test was used to compare the ATA distance among these three devices. The results are represented as mean ± SD, and the level of significance was set at a p value of <0.05.
Results
Data comparison
Table 1 shows the demographics of the study population. Figure 2 shows the data of the ATA measurements among the three devices. The ATA distance in the CASIA2 group (11.72 ± 0.32 mm) was significantly larger than that in the Pentacam group (11.32 ± 0.45 mm) (Bonferroni test, p = 0.016), or that in the TMS-5 group (11.16 ± 0.40 mm) (p < 0.001). There were no significant differences in the ATA distance between the Pentacam and TMS-5 groups (p = 0.420).
Repeatability
The repeatability (within-examiner differences) of the ATA measurements by three devices is shown in Fig. 3. The mean difference of the ATA measurement between measurements 1 and 2 was 0.01 mm (limit of agreement (LoA), −0.16 to 0.18 mm) in the CASIA2 group, −0.04 mm (LoA, −0.87 to 0.80 mm) in the Pentacam group, and −0.09 mm (LoA, −0.36 to 0.18 mm) in the TMS-5 group. The CoV of the ATA measurements 1 and 2 for a single examiner was 0.44% in the CASIA2 group, followed by 0.84% in the TMS-5 group, and 1.92% in the Pentacam group.
Reproducibility
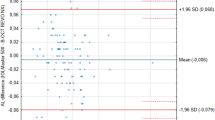
Figure 4 shows the reproducibility (between-examiner differences) of the ATA measurements among three devices. The mean difference between the ATA measurements for two examiners was 0.00 mm (LoA, −0.29 to 0.28 mm) in the CASIA2 group, 0.02 mm (LoA, −0.72 D to 0.77 mm) in the Pentacam group, and −0.01 mm (LoA, −0.41 to 0.40 mm) in the TMS-5 group. The CoV of the ATA measurements for the two examiners was 0.61% in the CASIA2 group, followed by 0.97% in the TMS-5 group, and 1.84% in the Pentacam group.
Discussion
In the present study, our results revealed that the ATA measured with the CASIA2 was significantly larger than that with the Pentacam, or that with the TMS-5, suggesting that these three devices cannot be used interchangeably in terms of ATA measurements. As far as we can ascertain, this is the first study to compare the ATA measurements among multiple instruments in healthy subjects. Although the exact reasons for this discrepancy remains unanswered, we assume that the differences in the principle (optical coherence tomography vs. Scheimpflug camera) and the methodology (automatic vs. manual) of the measurements may contribute to this discrepancy. Overall, our results imply that the ATA distance measured with the CASIA2 was ~0.40 and 0.56 mm larger than that with the Pentacam and the TMS-5, respectively. These differences in the ATA measurements among these three devices were not necessarily negligible for predicting the optimal ICL lens size. Therefore, it should be noted that these three devices cannot be used interchangeably for the optimal ICL size selection in daily practice.
Table 2 summarizes previous studies on the association between ATA and STS. Oh et al. [8] found a significant correlation of STS with ATA (r = 0.924, p < 0.001), but no significant correlation of STS with WTW (r = 0.006, p = 0.976). Reinstein et al. [10] showed that STS was significantly associated with both ATA and WTW (p < 0.001), but its correlation with ATA (r2 = 0.4578) was much higher than that with WTW (r2 = 0.3231). Goldsmith et al. [12] stated that direct ATA measurements using anterior segment optical coherence tomography may improve the sizing of angle-supported phakic intraocular lenses over the conventional estimation using WTW measurements. Nakamura et al. [9] recently showed by using the CASIA2 that the ATA was significantly correlated with the STS (r = 0.677), and that the optimal ICL lens size was highly correlated with the distance between the sclera on the nasal and temporal sides (r = 0.780) as well as the ATA (r = 0.715). These previous findings indicate that ATA is one of the best relevant parameters for predicting STS, which is essential for selecting the optimal ICL lens size in a clinical setting.
Our results also revealed that the CASIA2 provided the highest repeatability and reproducibility of the ATA measurements, followed by the TMS-5, and the Pentacam in healthy subjects, as evidenced by the narrow LoA and small CoV. This is also the first study to assess the detailed repeatability and reproducibility of ATA measurements using the Bland Altman plots and the CoV. We believe that this information is clinically helpful for precisely determining the ATA and subsequently predicting the optimal ICL lens size. The ATA distance can be automatically obtained by the CASIA2, whereas it needs to be manually acquired by the Pentacam and the TMS-5. Moreover, the Scheimpflug camera inevitably induces halation at the peripheral portion of the cornea. We assume that the automatic measurement and no occurrence of halation at the peripheral area both contribute to the highest repeatability and reproducibility of the ATA measurements in the CASIA2 group.
In summary, our results may support the view that the ATA distance measured with the CASIA2 was significantly larger than that with the Pentacam, or that with the TMS-5, and that the CASIA2 provided the highest repeatability and reproducibility of the ATA measurements, followed by the TMS-5, and the Pentacam. We should be aware that these instruments cannot be used interchangeably in terms of ATA measurements.
Summary
What was known before
Angle-to-angle (ATA) measurements may be helpful for selecting the optimal phakic intraocular lens size.
However, ATA measurement have not so far been compared among different devices.
What this study adds
The ATA distance measured with the CASIA2 was significantly larger than that with the Pentacam, or that with the TMS-5, indicating that these instruments cannot be used interchangeably in terms of ATA measurements.
References
Igarashi A, Shimizu K, Kamiya K. Eight-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Am J Ophthalmol. 2014;157:532–9.
Shimizu K, Kamiya K, Igarashi A, Shiratani T. Early clinical outcomes of implantation of posterior chamber phakic intraocular lens with a central hole (Hole ICL) for moderate to high myopia. Br J Ophthalmol. 2012;96:409–12.
Shimizu K, Kamiya K, Igarashi A, Shiratani T. Intraindividual comparison of visual performance after posterior chamber phakic intraocular lens with and without a central hole implantation for moderate to high myopia. Am J Ophthalmol. 2012;154:486–94.
Kamiya K, Shimizu K, Kobashi H, Igarashi A, Komatsu M. Three-year follow-up of posterior chamber toric phakic intraocular lens implantation for moderate to high myopic astigmatism. PLoS ONE. 2013;8:e56453.
Sheng XL, Rong WN, Jia Q, Liu YN, Zhuang WJ, Gu Q, et al. Outcomes and possible risk factors associated with axis alignment and rotational stability after implantation of the Toric implantable collamer lens for high myopic astigmatism. Int J Ophthalmol. 2012;5:459–65.
Rodríguez-Una I, Rodríguez-Calvo PP, Fernández-Vega Cueto L, Lisa C, Fernández-Vega Cueto A, Alfonso JF. Intraocular pressure after implantation of a phakic collamer intraocular lens with a central hole. J Refract Surg. 2017;33:244–9.
Kojima T, Yokoyama S, Ito M, Horai R, Hara S, Nakamura T, et al. Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol. 2012;153:632–7.
Oh J, Shin HH, Kim JH, Kim HM, Song JS. Direct measurement of the ciliary sulcus diameter by 35-megahertz ultrasound biomicroscopy. Ophthalmology. 2007;114:1685–8.
Nakamura T, Isogai N, Kojima T, Yoshida Y, Sugiyama Y. Implantable collamer lens sizing method based on swept-source anterior segment optical coherence tomography. Am J Ophthalmol. 2018;187:99–107.
Reinstein DZ, Archer TJ, Silverman RH, Rondeau MJ, Coleman DJ. Correlation of anterior chamber angle and ciliary sulcus diameters with white-to-white corneal diameter in high myopes using artemis VHF digital ultrasound. J Refract Surg. 2009;25:185–94.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Goldsmith JA, Li Y, Chalita MR, Westphal V, Patil CA, Rollins AM, et al. Anterior chamber width measurement by high-speed optical coherence tomography. Ophthalmology. 2005;112:238–44.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saito, A., Kamiya, K., Fujimura, F. et al. Comparison of angle-to-angle distance using three devices in normal eyes. Eye 34, 1116–1120 (2020). https://doi.org/10.1038/s41433-019-0653-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0653-2
This article is cited by
-
Comparison of corneal and lens density measurements obtained by Pentacam and CASIA2 in myopes
BMC Ophthalmology (2023)
-
Repeatability and Interobserver Reproducibility of a Swept-Source Optical Coherence Tomography for Measurements of Anterior, Posterior, and Total Corneal Power
Ophthalmology and Therapy (2023)
-
Swept-source optical coherence tomography and ultrasound biomicroscopy study of anterior segment parameters in primary angle-closure glaucoma
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)