Abstract
Objectives
To investigate if smoking was related to the risk of cataract surgery in diabetic patients.
Methods
A total of 9578 diabetic participants aged 45–65 years were enrolled from the 45 and Up Study, the largest population-based cohort study in Australia. Baseline questionnaire data were linked to the Medicare Benefits Schedule (MBS) and Pharmaceutical Benefits Scheme (PBS) database, which were both available from 2004 to 2016. Cataract surgery was determined according to the MBS. Smoking status were assessed by questionnaire. Cox regression was used to evaluate the association between smoking and incidence of cataract surgery during the follow-up.
Results
During a mean follow-up of 8.4 years, 995 participants underwent cataract surgery with a corresponding incidence of 12.4 cases per 1000 person-years. In all, 10.8% of participants were current smokers at baseline, 38.7% were former smokers, and 50.5% were never smokers. The incidence of cataract surgery was non-significantly higher in never-smoker compared to former or current smokers. Regression analysis showed no significant difference in cataract surgical risk among former, current, and never smokers. In addition, neither time since quitting of smoking nor age at quitting was associated with the risk of cataract surgery, although there was a marginally significant trend in a lower risk of cataract surgery with longer smoking cessation time for participant with normal weight (P for trend = 0.05).
Conclusions
Despite that smoking was found to be related to the cataract and cataract surgery in the general population, we did not find any association between smoking and cataract surgery in diabetic patients.
Similar content being viewed by others
Introduction
Cataract remains a leading cause of blindness and visual impairment worldwide [1]. According to the Global Burden of Disease Study 2010, one-third of the global blindness was attributed to cataract [2]. Despite the decrease in cataract prevalence and improvement in cataract surgery in recent decades, challenges remain to reduce the cataract burden in the aging society. The higher risk of cataract and cataract surgical complications among diabetic patients have been well established [3, 4]. Given that diabetes has been emerging a global epidemic in the modern world (451 million people in 2017) [5], and cataract extraction is the only available effective treatment, which also poses a major financial burden to the health system, identifying modifiable risk factors that may help reduce or delay cataract surgery among diabetic patients has substantial clinical and economic significance.
Smoking is an established risk factor for a wide range of diseases, including cardiovascular disease [6], lung cancer [7], age-related macular degeneration [8], and cataract [9]. There is evidence showing a dose–response effect of smoking on cataract risk and there are also isolated reports of an increased risk of cataract surgery with smoking [10]. Oxidative stress induced by smoking is thought to be, at least in part, the underlying mechanism for increased risk of cataract [11]. It is also reported that smoking could increase the risk of micro and macro-vascular complications of type 2 diabetes through its effect on insulin resistance, inflammation, and dyslipidemia [12, 13]. However, whether smoking could aggravate the risk of cataract surgery among diabetic patients, who are at higher risk of developing cataract, is less investigated.
Effect of smoking cessation on the risk of cataract and cataract surgery had been previously reported [10, 14,15,16], with some revealing a protective effect while others demonstrating that the risk of cataract remains elevated for many years following smoking cessation. In addition to a high cataract surgical rate and large diabetic population, Australia also has a characteristically long history of heavy smoking, high levels of smoking cessation and a low current smoking prevalence [17]. Thus, it is an ideal sample to evaluate the associations between smoking and cataract surgery among diabetic patients for making specific recommendations.
The purpose of this study was to investigate the effects of smoking intensity and cessation on the risk of cataract surgery among working-aged Australians with diabetes. We also assessed the quantitative association between smoking and cataract surgical risk among participants with different smoking intensity, as well as whether smoking cessation could benefit more in certain population subgroups.
Methods
Participants
The Sax Institute’s 45 and Up Study is a large prospective population-based cohort study of 266,896 men and women aged 45 years and over randomly sampled from the Department of Human Services (Formerly Medicare Australia) enrollment database. The study methodology had been described in detail elsewhere [18], and the study population was smaller than previously reported due to participant withdrawals. In brief, baseline participant recruitment was commenced in January 2006 and completed by December 2009. All participants entered the study by completing a mailed self-administered questionnaire and also providing written consent for long-term follow-up and linkage of their health information to routine health databases, including the Medicare Benefits Schedule (MBS) and Pharmaceutical Benefits Scheme (PBS). The overall response rate was nearly 18% and the baseline participants included about 10% of the NSW population aged 45 years and over.
Diabetic participants aged 45–65 years were enrolled for the current study, as most of the participants aged over 65 years had already undergone cataract surgery before baseline [19, 20]. Participants who responded positively to the question “Has a doctor ever told you that you have diabetes” in the baseline questionnaire or those who had been prescribed with diabetes medications according to PBS were identified as positive for diabetes status. Previous evidence from the 45 and Up Study had shown a high sensitivity and specificity for self-reported diabetes [21]. Exclusion criteria of the current study include: [1] gestational diabetes (N = 494); [2] participants who reported an age at diabetes diagnosis older than the baseline age (N = 146); [3] a history of cataract surgery or vitrectomy (N = 203); [4] missing data for smoking (N = 516); [5] participants with a body mass index (BMI) level of < 15 or > 50 kg/m2 (N = 214). Thus, a total of 9578 participants were included for analysis (Fig. 1). Ethics approval for the 45 and Up Study was granted by the University of New South Wales Human Research Ethics Committee. Ethics approval for this specific study was granted by The Royal Victorian Eye and Ear Hospital Human Research Ethics Committee.
Exposures
Smoking status was determined based on participants’ response to the baseline questionnaire, and further classified into three groups: never-smoker, former smoker, and current smoker. Never smokers were based on responses to the questions “Have you ever been a regular smoker?”. Current and former smokers were defined by answer to the question “Are you a regular smoker now?”. Current and former smokers were further asked about the age when they started smoking regularly, the average number of cigarettes they smoked each day, and the age when they stopped smoking regularly. Specific smoking-related questions in the 45 and Up Study had been previously reported [17]. Smoking intensity was calculated as the number of cigarettes and pipes/cigars smoked each day, which was categorized as < 10, 10–15, 16–20 and ≥ 21 cigarettes/day. Cumulative dose was calculated as the number of pack-years of tobacco, and further categorized into four groups: < 10, 10–19, 20–29 and ≥ 30 pack-years. Time since quitting was defined as the duration between the age at quit smoking and the current age, and further categorized into four groups: < 5, 5–14, 15–24, and ≥ 25 years.
Co-variates
Co-variates including baseline age, gender, household income, education level, BMI, history of hypertension (yes/no), history of cardiovascular disease (CVD) (yes/no), insulin treatment (yes/no), diabetes duration, alcohol drinking (yes/no), and physical activity were collected from self-reported questionnaires at baseline. Age was divided into four groups: 45–49, 50–54, 55–59, and 60–65 years (y). Education levels were classified as no qualifications, completion of a certificate or diploma but lower than a university degree, or a university degree or higher. Household income of the participant was categorized into four groups: < $AU20000, $AU20000–40000, $AU40000–70000 and > $AU70000. Diabetes duration was calculated based on participant response to the question “please cross the box and give your age when the condition was first found”, and further classified into four groups: < 5 years, 5–10 years, 10–20 years, and ≥ 20 years. Physical activity (PA) was calculated as the metabolic equivalent intensity level (MET-adjusted) number sessions of PA, which was further categorized into four groups: < 5, ≥ 5–9, 9–14, and ≥ 14 MET-adjusted sessions per week [22]. BMI was calculated from self-reported height and weight, which has been previously validated in this cohort [23]. BMI was categorized according to the WHO recommendation as follows: normal weight (15 to < 24.9 kg/m2), overweight (25.0 to < 29.9 kg/m2), and obese ( ≥ 30.0 to 50 kg/m2).
Outcome
Whether participants had undergone cataract surgery during the follow-up was ascertained by the MBS (Code: 42698 and 42702). Linkage of the 45 and Up Study cohort data to the MBS and PBS data, both available from 2004 to 2016, was done by the Sax Institute using a unique identifier that was provided by the Department of Human Services.
Statistical analysis
Baseline characteristics of the study participants with different smoking status (never, former, or current smokers) were calculated and compared using a χ2-test for categorical variables and t-test for continuous variables. Incidence rates with person-years of follow-up as the denominator were calculated from baseline until the date of cataract surgery or end of follow-up (31 December, 2016), whichever came first. Two Cox proportional hazards models were used to calculate the hazards ratios (HRs) and 95% confidence intervals (CI), to assess the effect of smoking intensity and cumulative dose of smoking on the risk of cataract surgery during the follow-up. The crude model was adjusted for age and gender, and the multivariate model, was further adjusted for income, education level, BMI, history of hypertension, CVD, diabetes (DM) duration, insulin use, alcohol drinking and PA. The association between smoking cessation and cataract surgery was assessed in different subgroups of gender, BMI and insulin treatment groups using the fully adjusted model. The never smokers group were used as the reference group in all the analysis. Missing values for co-variates were treated as separate categories. All analyses were performed using the SAS software (version 9.4; SAS Institute, Inc), and a two-sided P-value of < 0.05 was considered statistically significant.
Results
In this cohort of 9578 diabetic participants (mean [SD] age: 57.3[5.2] years; female: 45.6%), a total of 995 participant underwent cataract surgery during a mean follow-up of 8.4 years (80,373 person-years), corresponding to an incidence rate of 12.4 cases per 1000 person-years. Of all participants at baseline in this study, 10.8% were current smokers, 38.7% were former smokers, and 50.5% were never smokers.
Baseline characteristics of participants with different smoking status are shown in Table 1. Distribution of smoking status was significantly different in participants with different gender (P < 0.001), income (P < 0.001), education level (P < 0.001), CVD history (P < 0.001), and drinking status (P < 0.001). Men were more likely to be current or former smokers than women (P < 0.001). Ever-smokers tended to have a lower income and educational level compared to non-smokers, the likelihoods of CVD and alcohol drinking were also higher in ever-smokers (all P < 0.001). The distribution of age, BMI, and PA were not statistically different among current, former, and never smokers.
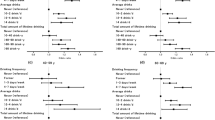
The mean (SD) number of cigarettes smoked per day and pack-year separately was 21.3 ± 10.5 and 41.3 ± 22.9 among current smokers and 24.1 ± 15.8 and 30.4 ± 27.5 among former smokers. The incidence of cataract surgery in never-smoker (11.3%) was higher than that in former smokers (10.4%) and current smokers (7.1%), but the differences were not statistically significant. Table 2 presents the relative risk estimates of cataract surgery by smoking intensity and cumulative dose. In the fully adjusted model, former smokers and current smokers didnot have significantly different risk of cataract surgery as compared to never smokers. In reference to never smokers, the risk of cataract surgery among former smokers with different cumulative smoking dose, smoking intensity, time since quit smoking and age at smoking cessation showed no statistically significant difference. In addition, comparison of current smokers with different smoking cumulative dose and intensity with never smokers also showed no statistically significant difference in cataract surgical risk. In a stratification analysis of the association between smoking cessation and the risk of cataract surgery, compared with never smokers, no significant associations were identified between time since quit smoking and cataract surgery among ever-smokers across different gender, BMI and insulin treatment status (Table 3). One exception was that time since smoking cessation of ≥ 25 years was associated with a lower risk of cataract surgery compared to never smokers in normal weight participants (HR, 0.44; 95% CI, 0.20–0.97), and there was also a marginally significant trend in a lower risk of cataract surgery with longer smoking cessation time for participant with normal weight (P for trend = 0.05).
Discussion
In this large cohort study of working-aged Australians with diabetes, we did not observe any association between smoking intensity or cessation with the risk of cataract surgery, except that longer smoking cessation time appeared to be associated with a lower cataract surgical risk in normal weight participants.
The incidence of cataract surgery among diabetic patients in our study was 12.4 per 1000 person-years, which was significantly higher than reported in similar age groups in the general population, but lower to that reported in other diabetic populations [24,25,26]. One study included 56,510 diabetic patients aged 40 years or above from UK and reported an incidence of cataract surgery of 20.4 per 1000 person-years [24]. The Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) recruited 2366 diabetic patients and reported an incidence of 27.6% in younger-onset group aged above 45 years and 24.9% in the older onset group aged above 30 years during a 10-year follow-up [27]. Granslund et al. [28] conducted a 25-year follow-up study of 727 patients with type 1 diabetes, the incidence of cataract surgery among participants aged 43–83 years was 28.7%. Difference in ethnicity, age distribution, economic status, and health care accessibility might partially explain the difference in reported cataract surgery incidence among previous studies.
Despite a widely acknowledged positive association between smoking and cataract risk in the general population, there are limited studies investigating the effect of current and former smoking on cataract and cataract surgery among diabetic patients, who are at higher risk of cataract development [20, 28,29,30]. Two cross-sectional studies reported that smoking was not associated with cataract among type 2 diabetes [29, 30]. The WESDR reported that the risk of cataract surgery was not increased in former or current smoker [20]. Our study enrolled a large population of Australian with diabetes and followed up for an average of 8.4 years, we found that neither smoking intensity nor smoking cessation was related to cataract surgical risk. Results of our study could add to evidence concerning the association between smoking and cataract surgery in diabetic patients. Although we did identify a marginal significant association between longer smoking cessation time and lower cataract surgical risk in normal weight participants, further studies are needed to confirm this association.
Smoking intensity and cessation had been correlated with cataract and cataract surgery in the general population [10, 14,15,16]. Two reviews had indicated a strong association between smoking and cataract [9, 31], especially among current smokers and for nuclear cataract. One population-based prospective study of 44,371 men reported that current smokers had a 42% increased risk of cataract surgery than never smokers, and the difference reduced to 21% after quitting smoking for >20 years, suggesting that the damage to the lens was reversible. Mechanisms underlying the associations between cigarette smoking and cataract was believed to be associated with oxidative stress. The free radicals from cigarette smoke could directly weaken the lens protein and cell membrane. Smoking could also lead to a lower level of circulating antioxidants and higher level of free radicals, resulting in a higher risk of cataractogenesis. The toxic effect from metal ions and cadmium accumulation could be another possible explanation [32]. However, we did not find any significant association between smoking intensity or cessation with cataract surgical risk in diabetic patients. One possible explanation may be that diabetic patients were more likely to develop cortical cataracts due to higher osmotic stress caused by sorbitol accumulation [3]. While smoking was significantly associated with increased risk of nuclear cataract and subcapsular cataract, smoking was not associated with cortical cataract [9].
Strengths of the current study include data from a population-based cohort, a large study size, a long follow-up, and the availability of multiple co-variates. The study population are ideal for investigating the association between smoking and cataract, given a sufficient sample size for participants with different smoking status, intensity and time since quit smoking. However, some potential limitations should be addressed. First, the baseline participant rate of the 45 and Up Study was only 18% and care should be taken if generalizing the study conclusion to the general population. However, it has been proven that representativeness is less impactful in cohort studies when an association between a potential risk factor and outcome of interest was investigated [33]. Second, participant’s surgical history before 2004 was unavailable in this study. We excluded participants aged over 65 years, who were most likely to have undergone cataract surgery at baseline, therefore reducing the chance of survival bias. A nation-wide survey in Australia reported that the coverage of cataract surgery among those in need was 98.9% in people aged 50 years and older [34]. Third, cataract surgeries performed in public hospitals were not assessed in this study as they were not recorded in the MBS database. This might limit the generalizability of our conclusion, but considering that 72% of cataract surgeries were performed in private setting in Australia, our findings could still offer valuable reference [35]. Lastly, smoking status was based on baseline self-reported questionnaire in our study, which may be subjective to recall bias and cannot reflect the change in life habits during the follow-up. Future studies should focus on investigating the time-to-time associations between smoking and cataract.
In summary, we found that neither smoking sensitivity nor smoking cessation was associated with the risk of cataract surgery among diabetic patients. More studies are needed to reveal the potential mechanisms for the discrepancy between general and diabetic populations. Smoking cessation should still be recommended for people with diabetes due to other beneficial health effect.
Summary
What was known before:
Smoking and smoking intensity and cessation were found to be related to the cataract and cataract surgery in the general population.
What this study adds:
This study did not find any association between smoking and the risk of cataract surgery in diabetic patients, who are at higher risk of developing cataract.
References
Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614–8.
Khairallah M, Kahloun R, Bourne R, Limburg H, Flaxman SR, Jonas JB, et al. Number of people blind or visually impaired by cataract worldwide and in world regions, 1990 to 2010. Invest Ophthalmol Vis Sci. 2015;56:6762–9.
Pollreisz A, Schmidt-Erfurth U. Diabetic cataract-pathogenesis, epidemiology and treatment. J Ophthalmol. 2010;2010:608751.
Goyal S, Joshua Hardin SHU, Ellabban AA, Warner DB, Sallam AB. Review and update of cataract surgery in the diabetic eye. Expert Rev Ophthalmol. 2017;12:359–71.
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
Stallones RA. The association between tobacco smoking and coronary heart disease. Int J Epidemiol. 2015;44:735–43.
Hecht SS. Cigarette smoking and lung cancer: chemical mechanisms and approaches to prevention. Lancet Oncol. 2002;3:461–9.
Velilla S, Garcia-Medina JJ, Garcia-Layana A, Dolz-Marco R, Pons-Vazquez S, Pinazo-Duran MD, et al. Smoking and age-related macular degeneration: review and update. J Ophthalmol. 2013;2013:895147.
Ye J, He JJ, Wang CJ, Wu H, Shi X, Zhang HN, et al. Smoking and risk of age-related cataract: a meta-analysis. Invest Ophth Vis Sci. 2012;53:3885–95.
Lindblad BE, Hakansson N, Svensson H, Philipson B, Wolk A. Intensity of smoking and smoking cessation in relation to risk of cataract extraction: A prospective study of women. Am J Epidemiol. 2005;162:73–9.
Chavez J, Cano C, Souki A, Bermudez V, Medina M, Ciszek A, et al. Effect of cigarette smoking on the oxidant/antioxidant balance in healthy subjects. Am J Ther. 2007;14:189–93.
Bajaj M. Nicotine and insulin resistance: when the smoke clears. Diabetes. 2012;61:3078–80.
Chang SA. Smoking and type 2 diabetes mellitus. Diabetes Metab J. 2012;36:399–403.
Weintraub JM, Willett WC, Rosner B, Colditz GA, Seddon JM, Hankinson SE. Smoking cessation and risk of cataract extraction among US women and men. Am J Epidemiol. 2002;155:72–9.
Christen WG, Glynn RJ, Ajani UA, Schaumberg DA, Buring JE, Hennekens CH, et al. Smoking cessation and risk of age-related cataract in men. Jama-J Am Med Assoc. 2000;284:713–6.
Lindblad BE, Hakansson N, Wolk A. Smoking cessation and the risk of cataract: a prospective cohort study of cataract extraction among men. Jama Ophthalmol. 2014;132:253–7.
Banks E, Joshy G, Weber MF, Liu B, Grenfell R, Egger S, et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med. 2015;13:38.
Banks E, Redman S, Jorm L, Armstrong B, Bauman A, 45 and Up Study Collaborators, et al. Cohort profile: the 45 and up study. Int J Epidemiol.2008;37:941–7.
Schofield D, Cunich M, Kelly S, Passey ME, Shrestha R, Callander E, et al. The impact of diabetes on the labour force participation, savings and retirement income of workers aged 45-64 years in Australia. PLoS ONE. 2015;10:e0116860.
Klein BE, Klein R, Moss SE. Incidence of cataract surgery in the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Am J Ophthalmol. 1995;119:295–300.
Comino EJ, Tran DT, Haas M, Flack J, Jalaludin B, Jorm L, et al. Validating self-report of diabetes use by participants in the 45 and Up Study: a record linkage study. BMC health Serv Res. 2013;13:481.
Australian Institute of Health and Welfare (AIHW). The Active Australia Survey: a guide and manual for implementation, analysis and reporting. Canberra: AIHW; 2003.
Ng SP, Korda R, Clements M, Latz I, Bauman A, Bambrick H, et al. Validity of self-reported height and weight and derived body mass index in middle-aged and elderly individuals in Australia. Aust NZ J Public Health. 2011;35:557–63.
Becker C, Schneider C, Aballea S, Bailey C, Bourne R, Jick S, et al. Cataract in patients with diabetes mellitus-incidence rates in the UK and risk factors. Eye. 2018;32:1028–35.
Nowak MS, Grabska-Liberek I, Michalska-Malecka K, Grzybowski A, Koziol M, Niemczyk W, et al. Incidence and characteristics of cataract surgery in Poland, during 2010–2015. Int J Environ Res Public Health. 2019;16: pii: E2188. https://doi.org/10.3390/ijerph16122188.
Daien V, Le Pape A, Heve D, Carriere I, Villain M. Incidence and characteristics of cataract surgery in France from 2009 to 2012: A National Population Study. Ophthalmology. 2015;122:1633–8.
Klein R, Klein BE, Moss SE, Cruickshanks KJ. The Wisconsin Epidemiologic Study of Diabetic Retinopathy: XVII. The 14-year incidence and progression of diabetic retinopathy and associated risk factors in type 1 diabetes. Ophthalmology. 1998;105:1801–15.
Grauslund J, Green A, Sjolie AK. Cataract surgery in a population-based cohort of patients with type 1 diabetes: long-term incidence and risk factors. Acta Ophthalmol. 2011;89:25–9.
Olafsdottir E, Andersson DK, Stefansson E. The prevalence of cataract in a population with and without type 2 diabetes mellitus. Acta Ophthalmol. 2012;90:334–40.
Raman R, Pal SS, Adams JS, Rani PK, Vaitheeswaran K, Sharma T. Prevalence and risk factors for cataract in diabetes: Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetics Study, report no. 17. Invest Ophthalmol Vis Sci. 2010;51:6253–61.
Kelly SP, Thornton J, Edwards R, Sahu A, Harrison R. Smoking and cataract: review of causal association. J Cataract Refr Surg. 2005;31:2395–404.
Ramakrishnan S, Sulochana KN, Selvaraj T, Rahim AA, Lakshmi M, Arunagiri K. Smoking of beedies and cataract—cadmium and vitamin-C in the lens and blood. Brit J Ophthalmol. 1995;79:202–6.
Mealing NM, Banks E, Jorm LR, Steel DG, Clements MS, Rogers KD. Investigation of relative risk estimates from studies of the same population with contrasting response rates and designs. BMC Med Res Methodol. 2010;10:26.
Foreman J, Xie J, Keel S, van Wijngaarden P, Crowston J, Taylor HR, et al. Cataract surgery coverage rates for Indigenous and non-Indigenous Australians: the National Eye Health Survey. Med J Aust. 2017;207:256–61.
Australian Commission on Safety and Quality in Health Care. Cataract surgery. Surgical interventions. 2016;305–14 https://www.safetyandquality.gov.au/search/cataract
Acknowledgements
This research was completed using data collected through the 45 and Up Study (www.saxinstitute.org.au). The 45 and Up Study is managed by the Sax Institute in collaboration with major partner Cancer Council NSW; and partners: the National Heart Foundation of Australia (NSW Division); NSW Ministry of Health; NSW Government Family & Community Services—Ageing, Carers and the Disability Council NSW; and the Australian Red Cross Blood Service. We thank the many thousands of people participating in the 45 and Up Study.
Funding
Professor Mingguang receives support from the University of Melbourne at Research Accelerator Program and the CERA Foundation. The Center for Eye Research Australia (CERA) receives Operational Infrastructure Support from the Victorian State Government. The specific project is funded by Australia China Research Accelerator Program at CERA. Professor Mingguang is also supported by the Fundamental Research Funds of the State Key Laboratory in Ophthalmology, National Natural Science Foundation of China (81420108008). The sponsor or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Han, X., Wu, C., Yan, X. et al. Are smoking intensity and cessation related to cataract surgical risk in diabetic patients? Findings from the 45 and Up Study. Eye 34, 383–391 (2020). https://doi.org/10.1038/s41433-019-0550-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0550-8
This article is cited by
-
NDRG2 Promotes Lens Epithelial Cells Senescence via NLRP3/Caspase1-Mediated Pyroptosis
Applied Biochemistry and Biotechnology (2023)