Abstract
Background
The role of the Global Leadership Initiative on Malnutrition (GLIM) criteria requires further validation. This study was aimed to evaluate the application of the GLIM criteria in patients with intestinal insufficiency and intestinal failure at nutritional risk on admission.
Methods
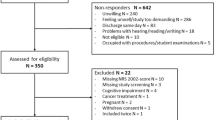
Three hundred and twenty eligible patients with intestinal insufficiency and intestinal failure at nutritional risk admitted to the clinical nutrition center in Jinling hospital from January 1, 2015 to January 1, 2020 were retrospectively identified from a database. GLIM and the European Society for Clinical Nutrition and Metabolism (ESPEN) criteria were used to diagnose malnutrition. Kappa test was conducted to determine consistency between the two diagnostic methods. Paired chi-square test (McNemar test) was used to compare the positive rate of the two diagnostic methods in diagnosing malnutrition. GLIM criteria were used as the reference standard, the receiver operating characteristic curve was used to estimate the diagnostic efficacy of phenotypic criteria (BMI, FFMI, ASMI and SMI) in malnutrition. The consistency to diagnose malnutrition between ESPEN and GLIM criteria was recorded, meanwhile the consistency and efficacy of GLIM phenotypic criteria to diagnose malnutrition were also recorded.
Results
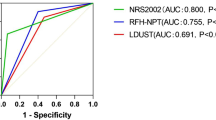
The malnutrition rate of GLIM diagnosis (93.4%) was higher than that of ESPEN diagnosis (80.9%), and the kappa value of the consistency test was 0.459. Combined with etiologic criteria (reduced food intake or assimilation), the incidence of malnutrition diagnosed by fat-free mass index (FFMI) (79.7%) was higher than body mass index (BMI) (70.6%), appendicular skeletal muscle index (ASMI) (55.6%), and skeletal muscle index (SMI) (53.1%) (McNemar test: p < 0.01), and the kappa values of consistency test were 0.561, 0.458, and 0.435, respectively. FFMI and BMI (p = 0.574) and SMI (p = 0.319) showed no statistically significant differences [except ASMI (p < 0.001)] in area under the curve for malnutrition diagnosis.
Conclusion
GLIM criteria showed a higher malnutrition rate than ESPEN criteria. The incidence of malnutrition diagnosed by FFMI was higher than other phenotypic criteria such as BMI, ASMI and SMI among patients with intestinal insufficiency and intestinal failure. The FFMI threshold needs to be combined with different situations to develop different recommendations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Pironi L, Arends J, Baxter J, Bozzetti F, Pelaez RB, Cuerda C, et al. ESPEN endorsed recommendations. Definition and classification of intestinal failure in adults. Clin Nutr. 2015;34:171–80.
Pironi L, Arends J, Bozzetti F, Cuerda C, Gillanders L, Jeppesen PB, et al. ESPEN guidelines on chronic intestinal failure in adults. Clin Nutr. 2016;35:247–307.
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, et al. Diagnostic criteria for malnutrition - An ESPEN Consensus Statement. Clin Nutr. 2015;34:335–40.
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition - A consensus report from the global clinical nutrition community. Clin Nutr. 2019;38:1–9.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101.
Chen LK, Lee WJ, Peng LN, Liu LK, Arai H, Akishita M, et al. Recent Advances in Sarcopenia Research in Asia: 2016 Update From the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2016;17:767.e1–7.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31.
Wang H, Hai S, Cao L, Zhou J, Liu P, Dong BR. Estimation of prevalence of sarcopenia by using a new bioelectrical impedance analysis in Chinese community-dwelling elderly people. BMC Geriatr. 2016;16:216.
Sheean P, Gonzalez MC, Prado CM, McKeever L, Hall AM, Braunschweig CA. American Society for Parenteral and Enteral Nutrition Clinical Guidelines: the validity of body composition assessment in clinical populations. JPEN J Parenter Enter Nutr. 2020;44:12–43.
Wang X, Tian F, Sun H, Zhang L, Gao X, Huang Y, et al. Insulin-like growth factor-1 as a nutritional monitoring factor in patients with chronic intestinal failure. Clin Nutr. 2019;38:1737–44.
Keller H, de van der Schueren MAE, Consortium G, Jensen GL, Barazzoni R, Compher C, et al. Global Leadership Initiative on Malnutrition (GLIM): Guidance on validation of the operational criteria for the diagnosis of protein-energy malnutrition in adults. JPEN J Parenter Enter Nutr. 2020;44:992–1003.
Kondrup J. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22:321–36.
Bahat G, Tufan F, Tufan A, Karan MA. The ESPEN guidelines on enteral nutrition-geriatrics: need for its promotion in practice. Clin Nutr. 2016;35:985.
McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically Ill patient: society of critical care medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enter Nutr. 2009;33:277–316.
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36:11–48.
Casirati A, Vandoni G, Della Valle S, Greco G, Platania M, Colatruglio S, et al. Nutritional status and body composition assessment in patients with a new diagnosis of advanced solid tumour: Exploratory comparison of computed tomography and bioelectrical impedance analysis. Clin Nutr. 2021;40:1268–73.
Kim D, Sun JS, Lee YH, Lee JH, Hong J, Lee JM. Comparative assessment of skeletal muscle mass using computerized tomography and bioelectrical impedance analysis in critically ill patients. Clin Nutr. 2019;38:2747–55.
White JV, Guenter P, Jensen G, Malone A, Schofield M, Academy Malnutrition Work G. et al. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enter Nutr. 2012;36:275–83.
Sanchez-Rodriguez D, Locquet M, Reginster JY, Cavalier E, Bruyere O, Beaudart C. Mortality in malnourished older adults diagnosed by ESPEN and GLIM criteria in the SarcoPhAge study. J Cachexia Sarcopenia Muscle. 2020;11:1200–11.
Yilmaz M, Atilla FD, Sahin F, Saydam G. The effect of malnutrition on mortality in hospitalized patients with hematologic malignancy. Supportive Care Cancer. 2019;28:1441–8.
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36:49–64.
Jensen GL, Mirtallo J, Compher C, Dhaliwal R, Forbes A, Grijalba RF, et al. Adult starvation and disease-related malnutrition: a proposal for etiology-based diagnosis in the clinical practice setting from the International Consensus Guideline Committee. Clin Nutr. 2010;29:151–3.
Allard JP, Keller H, Gramlich L, Jeejeebhoy KN, Laporte M, Duerksen DR. GLIM criteria has fair sensitivity and specificity for diagnosing malnutrition when using SGA as comparator. Clin Nutr. 2020;39:2771–7.
Matsumoto Y, Iwai K, Namikawa N, Matsuda S, Wakano C, Heya H, et al. The relationship between existing nutritional indicators and Global Leadership Initiative on Malnutrition (GLIM) criteria: A one-institution cross-sectional analysis. Clin Nutr. 2020;39:3099–104.
Akazawa N, Kishi M, Hino T, Tsuji R, Tamura K, Moriyama H. Using GLIM criteria, cutoff value for low BMI in Asian populations discriminates high or low muscle mass: a cross-sectional study. Nutrition 2021;81:110928.
Emsley C, King S, Nyulasi I, Snell G. A GLIMmer of insight into lung transplant nutrition: Enhanced detection of malnutrition in lung transplant patients using the GLIM criteria. Clin Nutr. 2021;40:2521–6.
Wang Y, Chen X, Wang Y, Liu Z, Fang Y, Peng Z, et al. Body composition measurement improved performance of GLIM criteria in diagnosing malnutrition compared to PG-SGA in ambulatory cancer patients: a prospective cross-sectional study. Nutrients. 2021;13:2744.
Clark AB, Reijnierse EM, Lim WK, Maier AB. Prevalence of malnutrition comparing the GLIM criteria, ESPEN definition and MST malnutrition risk in geriatric rehabilitation patients: RESORT. Clin Nutr. 2020;39:3504–11.
Jin M, Du H, Zhang Y, Zhu H, Xu K, Yuan X, et al. Characteristics and reference values of fat mass index and fat free mass index by bioelectrical impedance analysis in an adult population. Clin Nutr. 2019;38:2325–32.
Schutz Y, Kyle UU, Pichard C. Fat-free mass index and fat mass index percentiles in Caucasians aged 18-98 y. Int J Obes Relat Metab Disord. 2002;26:953–60.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gomez J, et al. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr. 2004;23:1430–53.
Acknowledgements
We thank Ruting Shen, Sitong Liu for aiding data collection. This project was supported by the National Science and Technology Research Funding for Public Welfare Medical Projects (201502022).
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: HL, XW, and XG. Performed the study: HL, LZ, XG, YZ, and XW. Analyzed the data: HL. Wrote the manuscript: HL. Reviewed the manuscript: LZ, XG, YZ, and XW. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Liu, H., Gao, X., Zhang, L. et al. Application of the GLIM criteria in patients with intestinal insufficiency and intestinal failure at nutritional risk on admission. Eur J Clin Nutr 76, 1003–1009 (2022). https://doi.org/10.1038/s41430-022-01084-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01084-8