Abstract
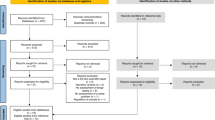
Inadequate sleep (i.e., duration and/or quality) is becoming increasingly recognized as a global public health issue. Interaction via the gut-brain axis suggests that modification of the gut microbial environment via supplementation with live microorganisms (probiotics) or nonviable microorganisms/microbial cell fractions (paraprobiotics) may improve sleep health. This systematic review and meta-analysis aimed to clarify the effect of consuming probiotics/paraprobiotics on subjective and objective sleep metrics. Online databases were searched from 1980 to October 2019 for studies involving adults who consumed probiotics or paraprobiotics in controlled trials, during which, changes in subjective and/or objective sleep parameters were examined. A total of 14 studies (20 trials) were included in meta-analysis. Random effects meta-analyses indicated that probiotics/paraprobiotics supplementation significantly reduced Pittsburgh Sleep Quality Index (PSQI) score (i.e., improved sleep quality) relative to baseline (−0.78-points, 95% confidence interval: 0.395–1.166; p < 0.001). No significant effect was found for changes on other subjective sleep scales, nor objective parameters of sleep (efficiency/latency) measured using polysomnography or actigraphy. Subgroup analysis for PSQI data suggested that the magnitude of the effect was greater (although not statistically) in healthy participants than those with a medical condition, when treatment contained a single (rather than multiple) strain of probiotic bacteria, and when the duration of treatment was ≥8 weeks. Probiotics/paraprobiotics supplementation may have some efficacy in improving perceived sleep health, measured using the PSQI. While current evidence does not support a benefit of consuming probiotics/paraprobiotics when measured by other subjective sleep scales, nor objective measures of sleep; more studies using well-controlled, within-subject experimental designs are needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Joint consensus statement of the American academy of sleep medicine and sleep research society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep. 2015;38:1161–83.
Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep disorders and sleep deprivation: an unmet public health problem. Washington DC, USA: National Academies Press; 2006.
Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The global problem of insufficient sleep and its serious public health implications. Healthcare. 2018;7:1–16.
Elder BL, Ammar EM, Pile D. Sleep duration, activity levels, and measures of obesity in adults. Public Health Nurs. 2016;33:200–5.
Ferrie JE, Kivimaki M, Akbaraly TN, Tabak A, Abell J, Davey Smith G, et al. Change in sleep duration and type 2 diabetes: the Whitehall II study. Diabetes Care. 2015;38:1467–72.
Kita T, Yoshioka E, Satoh H, Saijo Y, Kawaharada M, Okada E, et al. Short sleep duration and poor sleep quality increase the risk of diabetes in Japanese workers with no family history of diabetes. Diabetes Care. 2012;35:313–8.
Tobaldini E, Costantino G, Solbiati M, Cogliati C, Kara T, Nobili L, et al. Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases. Neurosci Biobehav Rev. 2017;74:321–9.
Kakizaki M, Kuriyama S, Sone T, Ohmori-Matsuda K, Hozawa A, Nakaya N, et al. Sleep duration and the risk of breast cancer: the Ohsaki Cohort Study. Br J Cancer. 2008;99:1502–5.
Naismith SL, Rogers NL, Lewis SJ, Terpening Z, Ip T, Diamond K, et al. Sleep disturbance relates to neuropsychological functioning in late-life depression. J Affect Disord. 2011;132:139–45.
Adams RJ, Appleton SL, Taylor AW, Gill TK, Lang C, McEvoy RD, et al. Sleep health of Australian adults in 2016: results of the 2016 Sleep Health Foundation national survey. Sleep Health. 2017;3:35–42.
Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of Healthy Sleep Duration among Adults—United States, 2014. Morb Mortal Wkly Rep. 2016;65:137–41.
The Sleep Council. The Great British bedtime report. United Kingdom; 2017. Available from: https://sleepcouncil.org.uk/wpcontent/uploads/2018/04/The-Great-British-Bedtime-Report-2017.pdf. Accessed 14 Nov 2019.
Medic G, Wille M, Hemels ME. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep. 2017;9:151–61.
Sleep Health Foundation. Asleep on the job: costs of inadequate sleep in Australia. ACT, Australia; 2017. Available from: https://www.sleephealthfoundation.org.au/files/Asleep_on_the_job/Asleep_on_the_Job_SHF_report-WEB_small.pdf. Accessed 10 Nov 2019.
Hafner M, Stepanek M, Taylor J, Troxel WM, van Stolk C. Why sleep matters—the economic costs of insufficient sleep: a cross-country comparative analysis. Rand Health Q. 2017;6:11.
Grandner MA, Jackson NJ, Izci-Balserak B, Gallagher RA, Murray-Bachmann R, Williams NJ, et al. Social and behavioral determinants of perceived insufficient sleep. Front Neurol. 2015;6:1–14.
Hale L, Emanuele E, James S. Recent updates in the social and environmental determinants of sleep health. Curr Sleep Med Rep. 2015;1:212–7.
Park JB, Nakata A, Swanson NG, Chun H. Organizational factors associated with work-related sleep problems in a nationally representative sample of Korean workers. Int Arch Occup Environ Health. 2013;86:211–22.
Vézina-Im L-A, Moreno JP, Thompson D, Nicklas TA, Baranowski T. Individual, social and environmental determinants of sleep among women: protocol for a systematic review and meta-analysis. BMJ Open. 2017;7:e016592.
Espiritu JRD. Aging-related sleep changes. Clin Geriatr Med. 2008;24:1–14.
LeBlanc M, Mérette C, Savard J, Ivers H, Baillargeon L, Morin CM. Incidence and risk factors of insomnia in a population-based sample. Sleep. 2009;32:1027–37.
Shrivastava D, Jung S, Saadat M, Sirohi R, Crewson K. How to interpret the results of a sleep study. J Community Hosp Intern Med Perspect. 2014;4:24983.
Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, et al. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013;36:1747–55.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Johns MW. A new method for measuring daytime sleepiness: the epworth sleepiness scale. Sleep. 1991;14:540–5.
Yamamoto Y. Standardization of revised version of OSA sleep inventory for middle age and aged. Brain Sci Ment Dis. 1999;10:401–9.
Aili K, Astrom-Paulsson S, Stoetzer U, Svartengren M, Hillert L. Reliability of actigraphy and subjective sleep measurements in adults: the design of sleep assessments. J Clin Sleep Med. 2017;13:39–47.
Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4:487–504.
Milner CE, Belicki K. Assessment and treatment of insomnia in adults: a guide for clinicians. J Couns Devel. 2010;88:236–44.
Krystal AD. A compendium of placebo-controlled trials of the risks/benefits of pharmacological treatments for insomnia: The empirical basis for U.S. clinical practice. Sleep Med Rev. 2009;13:265–74.
Attele AS, Xie JT, Yuan CS. Treatment of insomnia: an alternative approach. Alter Med Rev. 2000;5:249–59.
Leach MJ, Page AT. Herbal medicine for insomnia: a systematic review and meta-analysis. Sleep Med Rev. 2015;24:1–12.
Pearson NJ, Johnson LL, Nahin RL. Insomnia, trouble sleeping, and complementary and alternative medicine: analysis of the 2002 national health interview survey data. Arch Intern Med. 2006;166:1775–82.
Merritt SL, Gyllenhaal C, Peterson SD, Block KI, Gochenour T. Herbal remedies: efficacy in controlling sleepiness and promoting sleep. Nurse Pr Forum. 2000;11:87–100.
Lakhan SE, Vieira KF. Nutritional and herbal supplements for anxiety and anxiety-related disorders: systematic review. Nutr J. 2010;9:42–56.
Food and Agriculture Organization/World Health Organization. Report of a joint FAO/WHO expert consultation on evaluation of health and nutritional properties of probiotics in food including powder milk with live lactic acid bacteria. World Health Organization and Food and Agriculture Organization of the United Nations. Cordoba, Argentia; 2001. Available from: http://www.fao.org/3/a-a0512e.pdf. Accessed 22 Oct 2019.
de Almada CN, Almada CN, Martinez RCR, Sant’Ana AS. Paraprobiotics: evidences on their ability to modify biological responses, inactivation methods and perspectives on their application in foods. Trends Food Sci Technol. 2016;58:96–114.
Mayer EA, Tillisch K, Gupta A. Gut/brain axis and the microbiota. J Clin Invest. 2015;125:926–38.
Wallace CJK, Milev R. The effects of probiotics on depressive symptoms in humans: a systematic review. Ann Gen Psychiatry. 2017;16:1–10.
Benton D, Williams C, Brown A. Impact of consuming a milk drink containing a probiotic on mood and cognition. Eur J Clin Nutr. 2007;61:355–61.
Parkar SG, Kalsbeek A, Cheeseman JF. Potential role for the gut microbiota in modulating host circadian rhythms and metabolic health. Microorganisms. 2019;7:1–21.
Zhao D, Yu Y, Shen Y, Liu Q, Zhao Z, Sharma R, et al. Melatonin synthesis and function: evolutionary history in animals and plants. Front Endocrinol. 2019;10:1–16.
Wong RK, Yang C, Song GH, Wong J, Ho KY. Melatonin regulation as a possible mechanism for probiotic (VSL#3) in irritable bowel syndrome: a randomized double-blinded placebo study. Dig Dis Sci. 2015;60:186–94.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
van Rosendal SP, Osborne MA, Fassett RG, Coombes JS. Guidelines for glycerol use in hyperhydration and rehydration associated with exercise. Sports Med. 2010;40:113–29.
Maher CG, Moseley AM, Sherrington C, Elkins MR, Herbert RD. A description of the trials, reviews, and practice guidelines indexed in the PEDro database. Phys Ther. 2008;88:1068–77.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12.
Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Bouter LM, et al. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51:1235–41.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Chichester, UK: John Wiley & Sons; 2011.
Nishida K, Sawada D, Kuwano Y, Tanaka H, Sugawara T, Aoki Y, et al. Daily administration of paraprobiotic lactobacillus gasseri CP2305 ameliorates chronic stress-associated symptoms in Japanese medical students. J Funct Foods. 2017;36:112–21.
Cohen J. Statistical power analysis for behavioral sciences. NewYork, NY: Routledge; 1988.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Shrivastava D, Jung S, Saadat M, Sirohi R, Crewson K. How to interpret the results of a sleep study. J Community Hosp Intern Med Perspect. 2014;4:1–4.
Durlak JA. How to select, calculate, and interpret effect sizes. J Pediatr Psychol. 2009;34:917–28.
Takada M, Nishida K, Gondo Y, Kikuchi-Hayakawa H, Ishikawa H, Suda K, et al. Beneficial effects of Lactobacillus casei strain Shirota on academic stress-induced sleep disturbance in healthy adults: a double-blind, randomised, placebo-controlled trial. Benef Microbes. 2017;8:153–62.
Khalesi S, Sun J, Buys N, Jayasinghe R. Effect of probiotics on blood pressure: a systematic review and meta-analysis of randomized, controlled trials. Hypertension. 2014;64:897–903.
Zhang Q, Wu Y, Fei X. Effect of probiotics on glucose metabolism in patients with type 2 diabetes mellitus: A meta-analysis of randomized controlled trials. Medicina. 2016;52:28–34.
Nikbakht E, Khalesi S, Singh I, Williams LT, West NP, Colson N. Effect of probiotics and synbiotics on blood glucose: a systematic review and meta-analysis of controlled trials. Eur J Nutr. 2018;57:95–106.
Nakagawa M, Yamamoto H, Kawaji M, Miura N, Wakame K, Endo T. Effects of lactic acid bacteria-containing foods on the quality of sleep: a placebo-controlled, double-blinded, randomized crossover study. Funct Food Health Dis. 2018;8:579–96.
Kato-Kataoka A, Nishida K, Takada M, Suda K, Kawai M, Shimizu K, et al. Fermented milk containing Lactobacillus casei strain shirota prevents the onset of physical symptoms in medical students under academic examination stress. Benef Microbes. 2016;7:153–6.
Marotta A, Sarno E, Del Casale A, Pane M, Mogna L, Amoruso A, et al. Effects of probiotics on cognitive reactivity, mood, and sleep quality. Front Psych. 2019;10:1–11.
Nakakita Y, Tsuchimoto N, Takata Y, Nakamura T. Effect of dietary heat-killed Lactobacillus brevis SBC8803 (SBL88™) on sleep: a non-randomised, double blind, placebo-controlled, and crossover pilot study. Benef Microbes. 2016;7:501–9.
Dhiman RK, Rana B, Agrawal S, Garg A, Chopra M, Thumburu KK, et al. Probiotic vsl#3 reduces liver disease severity and hospitalization in patients with cirrhosis: a randomized, controlled trial. Gastroenterology. 2014;147:1327–37.e3.
Diop L, Guillou S, Durand H. Probiotic food supplement reduces stress-induced gastrointestinal symptoms in volunteers: a double-blind, placebo-controlled, randomized trial. Nutr Res. 2008;28:1–5.
Majeed M, Nagabhushanam K, Arumugam S, Majeed S, Ali F. Bacillus coagulans MTCC 5856 for the management of major depression with irritable bowel syndrome: a randomised, double-blind, placebo controlled, multi-centre, pilot clinical study. Food Nutr Res. 2018;62:1–13.
Nishida K, Sawada D, Kawai T, Kuwano Y, Fujiwara S, Rokutan K. Para-psychobiotic Lactobacillus gasseri CP2305 ameliorates stress-related symptoms and sleep quality. J Appl Microbiol. 2017;123:1561–70.
Kelly JR, Allen AP, Temko A, Hutch W, Kennedy PJ, Farid N, et al. Lost in translation? The potential psychobiotic Lactobacillus rhamnosus (JB-1) fails to modulate stress or cognitive performance in healthy male subjects. Brain Behav Immun. 2017;61:50–9.
Monoi N, Matsuno A, Nagamori Y, Kimura E, Nakamura Y, Oka K, et al. Japanese sake yeast supplementation improves the quality of sleep: a double-blind randomised controlled clinical trial. J Sleep Res. 2016;25:116–23.
Sawada D, Kawai T, Nishida K, Kuwano Y, Fujiwara S, Rokutan K. Daily intake of Lactobacillus gasseri CP2305 improves mental, physical, and sleep quality among Japanese medical students enrolled in a cadaver dissection course. J Funct Foods. 2017;31:188–97.
Yamamura S, Morishima H, Kumano-go T, Suganuma N, Matsumoto H, Adachi H, et al. The effect of Lactobacillus helveticus fermented milk on sleep and health perception in elderly subjects. Eur J Clin Nutr. 2009;63:100–5.
Bernhardt V, Rothkotter HJ, Kasten E. Psychological stress in first year medical students in response to the dissection of a human corpse. GMS Z Med Ausbild. 2012;29:1–17.
Bob MH, Popescu CA, Armean MS, Suciu SM, Buzoianu AD. Ethical views, attitudes and reactions of Romanian medical students to the dissecting room. Rev Med Chir Soc Med Nat Iasi. 2014;118:1078–85.
Russa AD, Mligiliche L. Inspiring Tanzanian medical students into the profession: appraisal of cadaveric dissection stress and coping strategies. Ital J Anat Embryol. 2014;119:268–76.
Ehlers CL, Somes C, Seifritz E, Rivier JE. CRF/NPY interactions: a potential role in sleep dysregulation in depression and anxiety. Depress Anxiety. 1997;6:1–9.
Opp MR. Corticotropin-releasing hormone involvement in stressor-induced alterations in sleep and in the regulation of waking. Adv Neuroimmunol. 1995;5:127–43.
Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46:124–32.
Takada M, Nishida K, Kataoka-Kato A, Gondo Y, Ishikawa H, Suda K, et al. Probiotic Lactobacillus casei strain Shirota relieves stress-associated symptoms by modulating the gut-brain interaction in human and animal models. Neurogastroenterol Motil. 2016;28:1027–36.
Bravo JA, Forsythe P, Chew MV, Escaravage E, Savignac HM, Dinan TG, et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci USA. 2011;108:16050–5.
Lastella M, Lovell GP, Sargent C. Athletes’ precompetitive sleep behaviour and its relationship with subsequent precompetitive mood and performance. Eur J Sport Sci. 2014;14:S123–S30.
Geiger-Brown JM, Rogers VE, Liu W, Ludeman EM, Downton KD, Diaz-Abad M. Cognitive behavioral therapy in persons with comorbid insomnia: a meta-analysis. Sleep Med Rev. 2015;23:54–67.
Johns MW. Sleep propensity varies with behaviour and the situation in which it is measured: the concept of somnificity. J Sleep Res. 2002;11:61–7.
Author information
Authors and Affiliations
Contributions
All authors were involved in the conception and design of this review. CI and SK were responsible for collating manuscripts and retrieving data. CI conducted the analysis of the data. All authors contributed to the drafting and revising of the article, and the final approval of the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Irwin, C., McCartney, D., Desbrow, B. et al. Effects of probiotics and paraprobiotics on subjective and objective sleep metrics: a systematic review and meta-analysis. Eur J Clin Nutr 74, 1536–1549 (2020). https://doi.org/10.1038/s41430-020-0656-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-0656-x