Abstract
Background
Malnutrition is confirmed to be associated with poor outcomes in stroke patients. The present study aimed to confirm that being at risk of malnutrition assessed by Nutritional Risk Screening Tool 2002 (NRS-2002) and the Controlling Nutritional Status (CONUT) score predicts poor outcomes at 3 months in acute ischemic stroke (AIS) patients.
Methods
In total, 682 patients with AIS were recruited within 7 days of stroke onset consecutively and 110 were dropped out. They were screened for risk of malnutrition using NRS-2002 and the CONUT score. The primary outcome is the follow-up modified Rankin Scale (mRS) score. Poor outcomes were defined as an (mRS) score ≥ 3 at 3 months post discharge.
Results
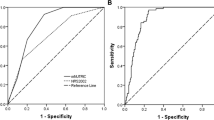
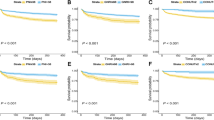
There was a significant difference in the mRS score at 3 months between patients at risk of malnutrition compared to those not at risk assessed by NRS-2002(P < 0.001) and CONUT (P = 0.011). The logistic regression model showed that the risk of malnourishment (according to NRS-2002), low risk of malnourishment (according to CONUT), and the moderate-to-severe risk of malnourishment (according to CONUT) were associated with higher risk of poor outcomes at 3 months (P < 0.001, P = 0.033, and P = 0.007). The multivariate logistic regression model (adjusted for confounding factors) demonstrated that the risk of malnourishment, according to the NRS-2002, was associated with the increasing risk of poor outcomes at 3 months (odds ratio = 2.31; 95% CI: 1.24–4.30; P = 0.008).
Conclusions
The risk of malnutrition assessed by NRS-2002 and CONUT can predict poor outcomes at 3 months in AIS patients. NRS-2002 is superior to CONUT in predicting poor outcomes at 3 months.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
World Health Organization (WHO). The top 10 causes of death. 2017. Geneva: WHO; 2018. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. 2017;135:759–71.
Aliasghari F, Izadi A, Khalili M, Farhoudi M, Ahmadiyan S, Deljavan R. Impact of premorbid malnutrition and dysphagia on ischemic stroke outcome in elderly patients: a community-based study. J Am Coll Nutr. 2019;38:318–26.
Konturek PC, Herrmann HJ, Schink K, Neurath MF, Zopf Y. Malnutrition in hospitals: it was, is now, and must not remain a problem! Med Sci Monit. 2015;21:2969.
Weun CC, Hasnan N, Latif LA, Majid HA. Nutritional status of post-acute stroke patients during rehabilitation phase in hospital. Sains Malays. 2019;48:129–35.
Nip W, Perry L, McLaren S, Mackenzie A. Dietary intake, nutritional status and rehabilitation outcomes of stroke patients in hospital. J Hum Nutr Dietetics. 2011;24:460–9.
Burgos R, Breton I, Cereda E, Desport JC, Dziewas R, Genton L, et al. ESPEN guideline clinical nutrition in neurology. Clin Nutr. 2018;37:354–96.
Wham C, McLean C, Teh R, Moyes S, Peri K, Kerse N. The BRIGHT Trial: what are the factors associated with nutrition risk? J Nutr Health Aging. 2014;18:692–7.
Reber E, Gomes F, Vasiloglou MF, Schuetz P, Stanga Z. Nutritional Risk Screening and Assessment. J. Clin. Med. [Internet]. MDPI AG. 2019;8:1065. https://doi.org/10.3390/jcm8071065.
Lopez Espuela F, Roncero-Martin R, Zamorano JDP, Rey-Sanchez P, Aliaga-Vera I, Portilla Cuenca JC, et al. Controlling Nutritional Status (CONUT) Score as a predictor of all-cause mortality at 3 months in stroke patients. Biol. Res Nurs. 2019;21:564–70.
Reinders I, Volkert D, de Groot LCPGM, Beck AM, Feldblum I, Jobse I, et al. Effectiveness of nutritional interventions in older adults at risk of malnutrition across different health care settings: Pooled analyses of individual participant data from nine randomized controlled trials. Clin Nutr. 2019;38:1797–806.
Naito H, Nezu T, Hosomi N, Aoki S, Kinoshita N, Kuga J, et al. Controlling nutritional status score for predicting 3-mo functional outcome in acute ischemic stroke. Nutrition. 2018;55-56:1–6.
Kokura Y, Maeda K, Wakabayashi H, Nishioka S, Higashi S. High nutritional-related risk on admission predicts less improvement of functional independence measure in geriatric stroke patients: a Retrospective Cohort Study. J Stroke Cerebrovasc Dis. 2016;25:1335–41.
Gomes F, Emery PW, Weekes CE. Risk of malnutrition is an independent predictor of mortality, length of hospital stay, and hospitalization costs in stroke patients. J Stroke Cerebrovasc Dis. 2016;25:799–806.
Wirth R, Smoliner C, Jäger M, Warnecke T, Leischker AH, Dziewas R. Guideline clinical nutrition in patients with stroke. Exp Transl Stroke Med. 2013;5:14.
Kondrup J, Rasmussen HH, Hamberg O, STANGA Z. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22:321–36. Group AahEW
van Bokhorst-de van der Schueren MAE, Guaitoli PR, Jansma EP, de Vet HCW. Nutrition screening tools: Does one size fit all? A systematic review of screening tools for the hospital setting. Clin Nutr. 2014;33:39–58.
Zhang Y, Zhang X. Controlling nutritional status score, a promising prognostic marker in patients with gastrointestinal cancers after surgery: a systematic review and meta-analysis. Int J Surg. 2018;55:39–45.
Yoshihisa A, Kanno Y, Watanabe S, Yokokawa T, Abe S, Miyata M, et al. Impact of nutritional indices on mortality in patients with heart failure. Open Heart 2018;5:e000730.
Ureshino H, Kusaba K, Kidoguchi K, Sano H, Nishioka A, Itamura H, et al. Clinical impact of the CONUT score and mogamulizumab in adult T cell leukemia/lymphoma. Ann. Hematatol. 2018;98:465–71.
Adams JrHP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993;24:35–41.
Kondrup J. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr 2003;22:321–36.
De Ulíbarri JI, González-Madroño A, de Villar NG, González P, González B, Mancha A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20:38–45.
Yoo S-H, Kim JS, Kwon SU, Yun S-C, Koh J-Y, Kang D-W. Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. Arch Neurol. 2008;65:39–43.
Collaboration FT. Poor nutritional status on admission predicts poor outcomes after stroke: observational data from the FOOD trial. Stroke. 2003;34:1450–6.
van Zwienen-Pot J, Visser M, Kuijpers M, Grimmerink M, Kruizenga H. Undernutrition in nursing home rehabilitation patients. Clin Nutr. 2017;36:755–9.
Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Inter Aging. 2012;7:287–98.
World Health Organization. Physical status: the use of and interpretation of anthropometry, Report of a WHO Expert Committee. Geneva, Switzerland: WHO; 1995.
Power L, de van der Schueren MAE, Leij-Halfwerk S, Bauer J, Clarke M, Visser M, et al. Development and application of a scoring system to rate malnutrition screening tools used in older adults in community and healthcare settings—a MaNuEL study. Clin Nutr 2019;38:1807–19.
Mould J. Nurses ‘must’control of the nutritional needs of stroke patients. Br J Nurs. 2009;18:1410–4.
Elia M, Stratton RJ. An analytic appraisal of nutrition screening tools supported by original data with particular reference to age. Nutrition. 2012;28:477–94.
O’donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–23.
Dávalos A, Ricart W, Gonzalez-Huix F, Soler S, Marrugat J, Molins A, et al. Effect of malnutrition after acute stroke on clinical outcome. Stroke. 1996;27:1028–32.
Heuschmann PU, Kircher J, Nowe T, Dittrich R, Reiner Z, Cifkova R, et al. Control of main risk factors after ischaemic stroke across Europe: data from the stroke-specific module of the EUROASPIRE III survey. Eur J Prevent Cardiol. 2015;22:1354–62.
Liang J, Liu W, Sun J, Gu X, Ma Q, Tong W. Analysis of the risk factors for the short-term prognosis of acute ischemic stroke. Int J Clin Exp Med. 2015;8:21915–24.
Chen C-F, Lai C-L, Lin H-F, Liou L-M, Lin R-T. Reappraisal of heart rate variability in acute ischemic stroke. Kaohsiung J Med Sci. 2011;27:215–21.
Tomii Y, Toyoda K, Suzuki R, Naganuma M, Fujinami J, Yokota C, et al. Effects of 24-hour blood pressure and heart rate recorded with ambulatory blood pressure monitoring on recovery from acute ischemic stroke. Stroke. 2011;42:3511–7.
Cederholm T, Jensen G, Correia MIT, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition–a consensus report from the global clinical nutrition community. J cachexia Sarcopenia Muscle. 2019;10:207–17.
Acknowledgements
We thank all the patients participated in the study.
Funding
This work was supported by project of the Science Committee in Wenzhou China. (Project number: Y20190561).
Author information
Authors and Affiliations
Contributions
ZC performed analyses and drafted the article; BZ and MZ designed the study and critically reviewed the paper; YW, HC, RF, CL, SY and ZL performed epidemiological investigation and data collection. All authors approved the final version of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Co-coressponding authors: Man-man Zhang, Bei-lei Zhu
Rights and permissions
About this article
Cite this article
Cai, Zm., Wu, Yz., Chen, Hm. et al. Being at risk of malnutrition predicts poor outcomes at 3 months in acute ischemic stroke patients. Eur J Clin Nutr 74, 796–805 (2020). https://doi.org/10.1038/s41430-020-0605-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-0605-8
This article is cited by
-
High Systemic Inflammatory Protein Index Is Associated with Clinically Ineffective Reperfusion in Acute Anterior Circulation Ischemic Stroke Patients Undergoing Endovascular Treatment
Molecular Neurobiology (2024)
-
The association between malnutrition status and hemorrhagic transformation in patients with acute ischemic stroke receiving intravenous thrombolysis
BMC Neurology (2023)
-
Association between malnutrition and stroke-associated pneumonia in patients with ischemic stroke
BMC Neurology (2023)
-
Malnutrition and cerebral intraparenchymal damage in patients with thrombosis of dural sinuses and/or cerebral veins
BMC Neurology (2023)
-
The relationship between the baseline geriatric nutritional risk index (GNRI) and neurological function at the convalescence stage in patients with stroke: a cross-sectional study
BMC Geriatrics (2023)