Abstract
Exosomes, which are nanoscale vesicles secreted by almost all cell types via paracrine pathways, play a crucial role in intercellular communication. For nearly a decade, exosomes have been widely exploited to develop novel biologic therapeutic strategies for recalcitrant clinical problems such as chronic wounds. Due to the excellent biocompatibility and immune stability of exosomes, exosome-based therapy has shown greater potential for chronic wound healing than other biotherapies (e.g., transplantation of stem cells) and holds great promise for the clinical treatment of chronic wounds. Here, recent advances in regulating the features and biological functions of cell-derived exosomes by biochemical and biophysical cues in the cell microenvironment are systematically summarized. Subsequently, microenvironmental cue-regulated exosomes as therapeutic strategies to improve chronic wound healing by regulating the inflammatory response, promoting cell proliferation and migration, facilitating angiogenesis, and regulating extracellular matrix (ECM) remodeling are discussed, and hydrogel-based exosome delivery systems used in the treatment of chronic wounds are highlighted. Finally, ongoing challenges and future opportunities in this rapidly developing field are proposed.
Similar content being viewed by others
Introduction
Chronic wounds, such as diabetic foot ulcers (DFUs), pressure ulcers (PUs), and venous leg ulcers (VLUs), are skin tissue defects that fail to proceed to the normal wound healing cascade and pass through an inflammatory phase, resulting in chronic inflammation that perpetuates the degree of tissue damage. Clinically, wounds due to any cause that fail to heal or show no healing tendency after treatment for more than a month are considered chronic wounds, which are prevalent and difficult to treat among elderly individuals. Chronic wounds are closely related to high treatment costs and become a large burden for both individuals and the entire health care system1. It has been estimated that in developed countries, the prevalence of chronic wounds ranges from 1.67 per 1000 population to 2.21 per 1000 population2, and the therapy costs are considerable and estimated at ~1–3% of the total health care expenditure3. Current therapeutic options for chronic wounds include routine dressing changes, debridement, infection management, skin tissue transplantation, and negative pressure wound therapy (NPWT)4, which aim to restore skin integrity rather than target wound healing from the perspective of pathophysiological mechanisms. Although efficient, these strategies are associated with several limitations, such as complications, wound recurrence, and variability in their healing effects5. Therefore, a great need remains for advanced therapeutic options for chronic wound healing.
It is now well known that the pathological characteristics of chronic wounds include prolonged exposure to proinflammatory cytokines, imbalanced expression of proteases and their inhibitors, altered availability and activity of growth factors, tissue hypoxia, and high oxidative stress levels6. Based on such in-depth understanding, various advanced biotherapies have been recently developed, such as the use of acellular dermal matrix7, growth factors8 or autologous platelet-rich plasma (PRP)9, and transplantation of stem cells10. Among these strategies, stem cell therapy based on mesenchymal stem cells (MSCs) has been the most promising because MSCs synthesize a substantial amount of growth factors and cytokines, which promote cell migration, proliferation, and vascularization, playing an active role in tissue regeneration11. However, considering the risk of uncontrolled proliferation and graft-versus-host disease (GVHD) associated with MSC transplantation, the direct application of MSC-based therapy is not feasible12. Recently, the therapeutic effect of MSCs in facilitating tissue repair was found to occur mainly through paracrine pathways. As an essential paracrine factor of MSCs, exosomes have been demonstrated to facilitate tissue regeneration in tissues including the myocardium13, bone14, and skin15. Exosomes, which are nanoscale vesicles secreted by cells into the extracellular environment, play a crucial role in intercellular communication16. The application of exosomes avoids the risk of stem cell overproliferation. In addition, exosomes are natural products of the body, leading to a low immune response17. Because their surfaces have intrinsic biochemical characteristics similar to those of cells, exosomes can avoid phagocytosis and bypass lysosomal phagocytosis18. Therefore, exosome-based therapy may hold great potential as a clinical solution for chronic wound healing.
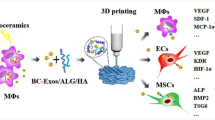
The therapeutic effect of exosomes is exerted when they are internalized or, in some cases, attached to the cell surface, and this effect usually depends on what they carry, which can include DNA, proteins, mRNAs, lipids, and miRNAs19. By transporting these bioactive components, exosomes participate in almost all steps of the wound repair process, including regulating inflammatory responses, promoting cell proliferation and migration, boosting angiogenesis, and regulating extracellular matrix (ECM) remodeling (Fig. 1). The contents of exosomes may vary based on the physiological and pathological states of the original cell20,21, and exosomes may inherit the adaptive changes of parental cells in response to biochemical and biophysical cues in the cell microenvironment, such as ECM mechanics and the oxygen level22,23. Therefore, it is possible to regulate the biological functions of exosomes by changing the cell microenvironment and to thus improve their therapeutic effects in chronic wound healing.
The left side of the figure shows some typical pathological characteristics of chronic wounds, including the presence of many inflammatory cells (e.g., neutrophils and M1 macrophages), overexpression of inflammatory factors (e.g., IL-1 and TNF-α), insufficient expression of growth factors (e.g., VEGF, FGF, and TGF-β), overexpression of MMPs and poor angiogenesis. The right side shows the roles of exosomes in chronic wound healing through, for instance, M1 to M2 phenotypic switching of macrophages, regulation of inflammation, promotion of cell proliferation and angiogenesis, and enhanced collagen formation.
Many original articles and reviews have discussed the applications of exosomes in wound repair, and most have focused on the biogenesis of exosomes and MSC-derived exosomes for tissue engineering24,25,26. In addition, some recent articles have discussed exosome-loaded biomaterials, such as hydrogels and scaffolds, and their applications in wound healing27,28,29. However, how biochemical and biophysical cues in the cell microenvironment mediate the features and biological functions of cell-derived exosomes and how these exosomes exert their therapeutic effects on each crucial process during wound healing are not yet clear. In this review, we fully probe the development of microenvironmental cue-regulated exosomes as therapeutic strategies to improve chronic wound healing. We first systematically summarize the regulatory effects of biochemical and biophysical cues in the cell microenvironment on the features and biological functions of exosomes. Then, cell-derived exosomes are discussed as therapeutic strategies for improving chronic wound healing through various mechanisms. Subsequently, we highlight hydrogel-based delivery systems for maintaining the bioactivity of exosomes and optimizing exosome release. Finally, we conclude with some thoughts on related challenges and future perspectives. This review aims to inspire and encourage research to further understand this flourishing field, to advance the development of microenvironmental cue-regulated exosomes as therapeutic strategies in the field of regenerative medicine, to acquire ideal exosome delivery systems for efficient delivery and to boost potential clinical applications of these cell-derived exosomes.
Regulation of the features and biological functions of cell-derived exosomes by microenvironmental cues
Cell-derived exosomes are extracellular vesicles (EVs) with diameters in the range of 40–160 nm. Exosomes are important mediators of intercellular communication through the paracrine pathway. The transport of exosomal contents, for instance, nucleic acids and proteins, into recipient cells effectively changes the biological responses of the recipient cells30. Because exosomes can regulate complex intracellular pathways, they show great potential in the treatment of many diseases, including central nervous system-related diseases, cardiovascular diseases and cancer progression16. In detail, design strategies for exosomes have been rapidly developed and widely applied in the treatment of tumors and neurological diseases. Most of the strategies are to increase the duration of exosomes in the circulation and to optimize the targeting of exosomes by modifying the surface proteins19. However, in chronic wound repair, distant targeted release of exosomes is not necessary. Different from the strategies mentioned above, preconditioning or modifying the origin cells to overexpress some contents of exosomes to optimize the specific biological functions of exosomes in the wound healing process is considered an important design strategy. For instance, Tao and colleagues overexpressed microRNA-126-3p in synovial mesenchymal stem cell-derived exosomes (SMSC-126-Exos). Such a design strategy could promote the stimulating effect of SMSC-126-Exos on the proliferation of epidermal fibroblasts and vascular endothelial cells27. In addition, exosomes released from nuclear factor erythroid 2-related factor 2 (Nrf2)-overexpressing adipose mesenchymal stem cells accelerated wound healing by promoting vascularization in a diabetic foot ulcer mouse model31. Therefore, cell-derived exosomes loaded with therapeutic agents can be designed and then transported to the desired target. Considering the core role of the loaded components in exerting the biological functions of exosomes, many studies have found that diverse biochemical and biophysical cues in the extracellular microenvironment have remarkable regulatory effects on the production, transport and especially cargo selection of exosomes (Table 1). These regulatory effects can be considered the responses of cells to microenvironmental cues mediated by exosomes through a paracrine pathway32,33. In the following section, we will focus on the regulatory effects of biochemical and biophysical cues in the cell microenvironment on the features of cell-derived exosomes (Fig. 2).
The features of exosomes, including production, transport, and cargo selection, can be altered when cells experience different biochemical (e.g., oxygen23,34,35, nitric oxide38, and chemical41,44,45 or biological molecules38,42,46) and biophysical (e.g., mechanical stimulation22, environmental dimensionality51, temperature56, ionizing radiation58, and low-intensity pulsed ultrasound (LIPUS)57) cues in their microenvironment.
Biochemical cues
The oxygen concentration has always been regarded as one of the most important biochemical factors in the cell microenvironment. Altered oxygen levels, including those in hypoxia34 and under oxidative stress35, are the pathophysiological basis of many diseases. Cardiac progenitor cells (CPCs) were found to secrete proangiogenic exosomes in which the miRNA secretome is altered in response to hypoxic conditions (Fig. 3A)34. Dougherty et al. confirmed the regulatory effect of hypoxia on CPC-EVs, where CPCs secreted more EVs and had a better effect in ischemic heart repair under physoxic conditions (5% O2) than under normoxic or hypoxic (1% O2) conditions36. Alternatively, hypoxic adipose mesenchymal stem cell-derived exosomes (ADSC-Exos) have also been proven to promote the angiogenic capacity of human umbilical vein endothelial cells (HUVECs) through VEGF/VEGF-R23. HIF-1α is widely known as a key communicator in cellular adaptation to low-oxygen conditions and in activating angiogenic factors. HIF-1α-overexpressing MSCs had enhanced secretion of exosomes and changed exosomal protein and miRNA levels, which promoted angiogenic capacity37. In addition to hypoxic conditions, exposure to oxidative stress has regulatory effects on exosomes. For example, mast cells exposed to oxidative stress produced exosomes in which expression of their mRNA transcripts was extensively different from exosomes produced by cells cultured under normal conditions, and such exosomes strengthened the tolerance of recipient cells to oxidative stress35. In addition, nitric oxide (NO) was found to be involved in manipulating exosome biofunctions, where NO-stimulated MSCs secreted exosomes with increased miR-126 and VEGF levels, promoting the angiogenic efficacy of MSC-Exos both in vitro and in vivo38. In summary, oxygen levels and the levels of other gaseous components in the cell microenvironment may be important chemical factors that regulate the biological functions of exosomes.
A Hypoxic CPC-Exos altered the miRNA secretome and promoted angiogenesis. (a) Matrigel assay of cardiac endothelial cells treated with CPC-Exos under hypoxic or normoxic conditions. Scale bar, 1 mm. (b) qRT‒PCR analysis of miRNAs regulated in hypoxic CPC exosomes (light bars) and donor CPCs (dark bars). Three miRNAs were found to be increased in recipient endothelial cells. The data are expressed as the mean ± SEM. *p < 0.05, **p < 0.01, ***p < 0.001. Reproduced with permission34. Copyright 2014, Wolters Kluwer Health. B 3,3′-Diindolylmethane (DIM) improved the therapeutic effect of hucMSC-Exos by upregulating Wnt11 expression. (a) H&E staining of wound tissue treated with shGFP-hucMSCs, shGFP-DIM-hucMSCs, shWnt11-hucMSCs, and shWnt11-DIM-hucMCs. (b) Western blot analysis of the expression of Wnt11 in hucMSCs and DIM-hucMSC-Exos. (c) ELISA was used to detect the expression level of Wnt11 in hucMSCs, DIM-hucMSC-derived exosomes, and exosome-free CdM (n = 6; ***p < 0.001). Reproduced with permission41. Copyright 2017, Ivyspring International. C Platelet-derived growth factor (PDGF) promotes exosome-mediated angiogenesis by stimulating EV secretion and altering the protein composition of EVs. (a) Quantitative analysis of vessel-like structure formation in response to EVs in the presence of antibodies against c-kit or SCF (mean ± SEM, #p < 0.05 vs. “control”, *p < 0.05 vs. “PDGF-EVs”, n = 7). (b) Western blot analysis of EVs derived from ASCs under basal conditions (b-EVs), EVs derived from ASCs after PDGF stimulation (PDGF-EVs) and human microvascular endothelial cells (HMECs) after stimulation with these EVs. Reproduced with permission46. Copyright 2014, BioMed Central.
In addition, many researchers have investigated the regulatory effects of chemical or biological molecules on exosome features. For instance, 3,3′-diindolylmethane (DIM), a natural small-molecule compound with potential in tissue injury repair39,40, facilitated the stemness and therapeutic effects of human umbilical cord MSCs (hucMSCs) in wound healing by upregulating Wnt11 expression in hucMSC-derived exosomes (Fig. 3B)41. Heparanase was found to facilitate the production of exosomes derived from tumor cells (e.g., myeloma, lymphoblastoid and breast cancer) and to upregulate exosomal protein cargo involved in tumor progression, such as syndecan-1, HGF, and VEGF42. In addition, some researchers have examined the regulatory effects of pharmaceutical molecules on exosomes. Transfer of the Epstein‒Barr virus (EBV) oncoprotein latent membrane protein 1 (LMP1) via exosomes is associated with NPC metastasis. The tumor suppressor miRNA-203 was found to be downregulated by LMP143. Aspirin was demonstrated to reverse this process by inhibiting exosomal LMP1 secretion by EBV-positive cells and by boosting miR-203 expression44. In addition, the 3-hydroxy-3-methylglutaryl-CoA (HMG CoA) inhibitor simvastatin was found to reduce the synthesis, localization and secretion of exosomes from different donor cells owing to its cholesterol-lowering effect. For example, simvastatin showed a protective effect against atherosclerosis because it reduced exosome production from monocytes and attenuated endothelial cell migration mediated by exosome-enclosed miR-15045. In addition, the ability of biomacromolecules, such as cytokines or growth factors, to regulate the features of exosomes has been investigated. Platelet-derived growth factor (PDGF) was found to stimulate ASC-EV secretion and to alter the protein composition to facilitate angiogenesis. PDGF-stimulated EVs could traffic c-kit and its ligand, stem cell factor (SCF), which are related to proangiogenic activity (Fig. 3C)46. TGF-β1 has also been found to enhance the expression of miR-135b in MSC-derived exosomes and to thus promote chondrocyte proliferation47. All these results indicate that various molecules can be used to influence exosome regulation.
Biophysical cues
Physical changes such as changes in dimensionality, mechanical stimulation, temperature, and radiation in the extracellular environment also influence cell secretion behavior22,48,49. For example, the dimensionality of the environment in which donor cells are located has been confirmed to impact exosome regulation50,51,52. Exosomes released from a 3D tissue-engineered Ewing’s sarcoma type I tumor model were smaller than those in monolayer cultures but had a size distribution similar to that of exosomes in patient plasma. In addition, 3D bioengineered tumor exosomes contained higher mRNA levels of the polycomb histone methyltransferase EZH2, a potential tumor biomarker, than monolayer cultures50. Haraszti and colleagues found improved production of MSC-Exos through 3D culture combined with a method of exosome isolation termed tangential flow filtration (TFF). Moreover, they used exosomes produced with this combined strategy to deliver Huntingtin (Htt) siRNA to neurons and found that these 3D-TFF-derived exosomes were more efficient at siRNA transfer and Htt silencing in neurons than controls, demonstrating that 3D-TFF-derived exosomes more efficiently transferred exosomal cargo (Fig. 4A)51. In addition, 3D spheroid cultured hBM-MSCs generated more exosomes than those prepared by 2D culture. In addition to environmental dimensionality, cellular adhesion itself might also play a crucial role in exosome production. The number of exosomes decreased with increasing cell density in 2D cultured hBM-MSCs, demonstrating that a nonadherent state might facilitate the efficiency of exosome output52. Thus, cells with different environmental dimensionality have different regulatory effects on the secretion and properties of exosomes.
A 3D culture and TFF treatment facilitated the MSC secretion of more exosomes with higher efficiency in transport capacity. (a) Yield of exosomes isolated by 2D-UC, 2D-TFF, 3D-UC, or 3D-TFF (n = 12). (b) Huntingtin (Htt) mRNA levels in neurons treated with exosomes containing Htt siRNA. (c) Time course of fluorescence in primary neurons treated with exosomes containing Cy3-labeled siRNA. Reproduced with permission51. Copyright 2018, Elsevier. B Mechanical stretch regulated EV release and vesicular miRNA expression in MLE-12 cells. (a) The effects of 10% cyclic stretch (left) and 5% continuous stretch (right) on the number of EVs. *p < 0.05 (b) Volcano graph of the miRNA levels in EVs after 5% continuous stretch (left) and 10% cyclic stretch (right). Reproduced with permission22. Copyright 2020, John Wiley and Sons. C Ionizing radiation influenced exosome abundance and molecular composition to promote tumor cell migration. (a) Exosome abundance at 24 h posttreatment with 2 to 8 Gy of radiation (n = 3). (b) Effect of exosomes on the migration of U87MG cells when used as a chemoattractant or upon preincubation of exosomes with the cells (n = 3). (c) CTGF gene expression levels in U87MG cell-derived exosomes and U87MG cells by qRT‒PCR. Data are shown as the mean ± SEM, n = 3. #p < 0.01, *p < 0.05 (d) Immunoblot analysis of IGFBP2 protein levels in U87MG cell-derived exosomes and U87MG cells. Reproduced with permission58. Copyright 2013, Elsevier.
In addition to dimensionality, mechanical stimulation may affect the production and function of exosomes. When mechanical stretch forces were applied to MLE-12 lung epithelial cells, 10% cyclic stretching was found to augment EV release, while 5% continuous stretching did not. On the other hand, both cyclic and continuous mechanical stimulation changed the expression of specific miRNAs inside the vesicles (Fig. 4B)22. Moreover, exosomes released from HUVECs improved angiogenic capacity in the ischemic myocardium after shock wave therapy compared with that in the absence of treatment. RNA interference experiments confirmed that miR-19a-3p is the vesicular component responsible for the mechanical simulation effect53. Furthermore, Pironti et al. established different mechanical stress models including exposure to osmotic stretch in vitro and the sera of mice undergoing cardiac pressure overload in vivo to study the influence of mechanical stress on exosomes54. Mechanical stress was found to induce the release of exosomes containing angiotensin II type I receptor (AT1R). Furthermore, AT1R-enriched exosomes were predominantly released by cardiomyocytes under pressure overload and targeted cardiomyocytes, skeletal myocytes, and mesenteric resistance vessels to elevate systolic blood pressure in response to angiotensin II.
Many other physical cues in the cell microenvironment play a role in the regulation of exosomes. For instance, temperature has been proven to be a critical factor in maintaining the activity of EVs. EVs from human endothelial cells infected with Kaposi’s sarcoma-associated herpesvirus (KSHV) were shown to have the potential to activate the complement system55. Different storage temperatures were discovered to impact the properties of EVs isolated from KSHV-infected human endothelial cells. The number of EVs decreased as the storage temperature rose, and protein markers of EVs and the biological activity of the activated complement system were altered under different temperature conditions56. In addition, low-intensity pulsed ultrasound (LIPUS) could promote the bioactivity of exosomes derived from bone marrow dendritic cells (BMDC-Exos) and could thus induce anti-inflammatory responses57. HUVECs incubated with BMDC-Exos exhibited decreased TNF-α-induced expression of intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1) at both the gene and protein levels. After LIPUS treatment, the BMDC-Exos were enriched in miRNA-16 and miRNA-21, limiting the activation of NF-κB, as reflected by the downregulation of IκB kinase (IKK)-α and phosphorylated p65. By transporting these miRNAs into HUVECs, LIPUS-treated BMDC-Exos impeded TNF-α-induced inflammation by inhibiting the NF-κB signaling pathway. In addition, radiation, another major physical factor in the environment, has been confirmed to significantly impact intercellular communication through various signal transduction systems. For example, ionizing radiation increased the release of exosomes from U87MG glioma cells and promoted the biological functions of exosomes to facilitate the migration of recipient cells (Fig. 4C)58. Furthermore, proteins associated with signaling pathways crucial for cell migration, such as insulin-like growth factor binding protein 2 (IGFBP2) and connective tissue growth factor (CTGF), were increased in irradiated cells and the exosomes released by these cells. In addition, coculture with exosomes derived from irradiated cells enhanced the protein expression of CTGF in recipient cells.
Mechanisms of exosome-based therapeutic strategies for treating chronic wounds
The biological functions of exosomes in regulating complex intracellular pathways have made exosomes promising therapeutic strategies for treating many diseases. Since Valadi et al. discovered that exosomes could implement intercellular communication through transportation of RNA in 2007, exosome-related studies have flourished59. Exosomes were initially studied in the repair of ischemic tissue injuries, such as acute kidney injury and myocardial ischemia‒reperfusion injury60,61,62. Ringhino et al. in 2012 found that endothelial progenitor cell-derived microvesicles improved neovascularization in hind limb ischemia mice63. Since 2015, many studies have focused on the application of exosomes in wound repair, most of which have been conducted on MSC-derived exosomes. With the deepening of research, studies on exosomes in chronic wound repair have been limited to the observation of the healing process, and exploring the mechanisms of exosome functions in the process of wound healing has begun. Specifically, these studies have revealed how exosomes act in different stages of wound healing. As carriers of paracrine signals from cells, exosomes deliver proteins, mRNAs, microRNAs, and other signaling molecules to target cells and promote wound healing through different mechanisms, showing greater advantages than other biotherapies for chronic wound treatment (Table S1). In this section, we describe the specific mechanisms of cell-derived exosomes as therapeutic strategies for improving chronic wound healing (Fig. 5).
Regulation of the inflammatory response
A prolonged inflammatory response is an important factor associated with refractory chronic wounds. Previous studies have shown that the healing of chronic wounds is improved by correcting this extended inflammatory response64. Recent works have shown that cell-derived exosomes mediate the inflammatory response. Thus, these exosomes show great potential for chronic wound treatment. For example, macrophage-derived exosomes (Mø-exos) were proven to have anti-inflammatory effects by reducing the secretion of proinflammatory enzymes and cytokines, contributing to the repair of diabetic wounds by significantly accelerating angiogenesis (Fig. S1A)65. Histological examination showed that Mø-exos significantly reduced infiltrating inflammatory cells, including neutrophils and macrophages, and promoted the formation of granulation tissue characterized by more new blood vessels than those formed in PBS-treated diabetic wounds after 7 days of treatment. Moreover, Mø-exos suppressed the expression of inflammatory cytokines in vivo. Immunohistochemistry staining revealed decreased levels of TNF-α and IL-6 in Mø-exo-treated wound sites compared to those in the controls. Notably, the combination of lipopolysaccharides (LPS) and Mø-exos enhanced inflammatory cell infiltration, elevated the expression of IL-6 and TNF-a, and decreased the formation of neovessels, demonstrating that LPS-induced local inflammation offset exosome-mediated pro-healing effects65. In addition, further studies by Kim and coworkers reported that exosomes derived from M2 macrophages (M2-Exos) could promote cutaneous wound repair by inducing the conversion of macrophages with a proinflammatory M1 phenotype in wounded tissues into macrophages with a reprogrammed M2-like phenotype (Fig. S1B)66. Within 24 h after treatment with M2-Exos, M1- and M2-specific markers (e.g., iNOS and arginase) had clearly been switched off and switched on, respectively, suggesting successful completion of macrophage phenotype switching66. Alternatively, MSC-derived exosomes preconditioned with LPS (LPS pre-Exos) had similar inhibitory effects on chronic inflammatory responses by regulating macrophage polarization. In detail, inflammatory THP-1 cells were converted to M2 macrophages by LPS pre-Exos. The RT‒PCR results showed that the expression of anti-inflammatory cytokines (e.g., TGF-β and IL-10) and M2 macrophage surface markers (e.g., CD163) in THP-1 cells was increased, while the expression of the proinflammatory cytokines TNF-α, IL-1, and IL-6 was reduced after 48 h of LPS pre-Exo treatment under high-glucose conditions (Fig. S1C)67. These exosomal functions were further proven to be achieved via the TLR4, NF-κB, STAT3, and AKT signaling pathways by the transportation of miR-let-7b. In addition, miR-181c in huc-MSC-derived exosomes (hUMSC-Exos) suppressed the inflammatory response by inhibiting the Toll-like receptor 4 (TLR4) signaling pathway in a burned mouse model (Fig. S1D)68. In macrophages with LPS-stimulated inflammation, the protein expression of NF-κB/P65, p-P65, and TLR4 was obviously higher than that in macrophages treated with hUMSC-Exos. Moreover, the expression level of miR-181c was higher in LPS-stimulated macrophages cocultured with hUCMSC-Exos than in LPS-stimulated macrophages without exosome treatment. ELISAs demonstrated that hUCMSC-Exos successfully inhibited IL-1β and TNF-α levels after LPS stimulation but notably increased IL-10 levels. All these results indicated that cell-derived exosomes (e.g., exosomes from macrophages and MSCs) can regulate inflammatory responses, protect injured tissues and accelerate wound healing. In particular, exosomes are rich in miRNAs, which play a crucial role in the regulation of inflammation.
Promotion of cell proliferation and migration
Cell proliferation and migration play fundamental roles in wound repair. Specifically, epithelial cells, fibroblasts, and endothelial cells that migrate to the wound site perform specific functions during wound healing. In detail, fibroblasts fill tissue defects and synthesize ECM, endothelial cells promote angiogenesis, and epithelial cells gradually cover the wound69. MSC-derived exosomes can regulate the proliferation and migration of the above cells by transporting their encapsulated components. For example, exosomes derived from adipose mesenchymal stem cells (ASCs-Exos) could stimulate the proliferation and migration of fibroblasts in a dose-dependent manner to facilitate cutaneous wound healing (Fig. S2A)26. After treatment with ASC-Exos, fibroblast migration at 12 h and 24 h was increased compared to that of the control group, as determined by scratch and Transwell migration assays. In addition, the expression of genes associated with cell migration and proliferation, such as N-cadherin, cyclin-1 and proliferating cell nuclear antigen (PCNA), was upregulated in fibroblasts by ASC-Exos. Furthermore, the high levels of microRNA-21 in ASC-Exos enhanced the migration and proliferation of HaCaT cells through the PI3K/AKT pathway, which indicated that microRNA-21 might be a key cargo in ASC-Exos that promotes cell migration and proliferation70. Similarly, exosomes isolated from human bone marrow MSCs (BMSC-Exos) could induce the growth and promote the migration of fibroblasts from both normal and diabetic wounds. The MTT assay revealed that the growth of these two fibroblast lines was significantly increased in a dose-dependent manner compared to that in controls. Furthermore, the results of the scratch assay indicated the increased migration of fibroblasts from both normal and diabetic wounds in the BMSC-Exo group71. In addition, Zhang’s group found that hUMSC-Exos could reverse acute thermal injury‐induced cell apoptosis via activation of the β‐catenin signaling pathway to accelerate wound healing (Fig. S2B)72. In comparison to PBS, hUMSC-Exos significantly suppressed heat stress‐induced apoptosis in HaCaT cells and primary dermal fibroblasts (DFLs) and promoted their proliferation. Western blot analyses showed lower Bax levels in HaCaT cells and DFLs treated with hUMSC-Exos than in cells without hUMSC-Exo treatment, but Bcl‐2 expression was higher in the hUMSC-Exos group than in the control groups. In addition, the enhanced PCNA expression by hUMSC-Exos indicated an increased level of cell proliferation. The Wnt4 protein in hUMSC-Exos activated the Wnt/β-catenin signaling pathway and enhanced the expression of proliferative proteins (e.g., PCNA, N-cadherin and cyclin D3) in HaCaT cells, thus promoting cell proliferation and migration. This effect was abrogated by the β-catenin inhibitor ICG001. The decreased expression of PCNA, N-cadherin, and cyclin D3 and suppressed cell proliferation and migration observed in the presence of ICG001 confirmed the role of the β-catenin pathway. In addition, under high-cell-density conditions, the hUMSC-Exo-derived protein 14-3-3ζ could activate the Hippo pathway to reverse the Wnt/β-catenin pathway and suppress cell proliferation and migration, preventing excessive repair and scar formation73. In addition to stem cell-derived exosomes, exosomes from other sources are involved in promoting cell proliferation and migration during the wound healing process. For example, exosomes isolated from PRP could promote fibroblast-related functions and facilitate wound healing74. These studies have shown that exosomes derived from diverse sources can enhance the proliferation and migration of cells, especially fibroblasts, thereby accelerating wound healing.
Promotion of angiogenesis
Angiogenesis is considered to be essential for wound healing since it is crucial for the maintenance of oxygen and nutrient delivery. However, this important process is usually compromised in chronic wounds, especially in DUs75. Many recent works have investigated the role of exosomes in the process of angiogenesis during chronic wound repair due to their delivery of proteins and miRNAs. For instance, Chen and colleagues found that urine-derived stem cell exosomes (USC-Exos) could facilitate diabetic wound healing by enhancing angiogenesis by transferring a proangiogenic protein named deleted in malignant brain tumors 1 (DMBT1)76. ASC-Exos were found to upregulate the expression of the proangiogenic genes Ang1 and Flk1, downregulate the expression of the antiangiogenic genes Vash1 and TSP1 in HUVECs and enhance angiogenesis both in vitro and in vivo (Fig. S3A)77. Specifically, ASC-Exos may facilitate the formation of endothelial tip cells to modulate endothelial cell angiogenesis by inhibiting the expression of the angiogenic inhibitor delta-like 4 (DLL4) through the transportation of miRNA-125a. Moreover, a series of miRNAs, such as miR-30b, miR-30c, miR-424, and let-7f, are thought to be transferred by MSC-Exos and to play roles in regulating angiogenesis78. Exosomes derived from human umbilical cord blood-derived endothelial progenitor cells (EPC-Exos) were also demonstrated to have proangiogenic and prohealing effects in diabetic rat models. EPC-Exos could be internalized into endothelial cells and promote their proliferation and migration and enhance tube formation (Fig. S3B)25. Erk1/2 signaling exerts its important effect in promoting angiogenesis responses by EPC-Exos. In addition, MSC-Exos are thought to activate the AKT, STAT3, and NF-κB signaling pathways to induce the upregulation of growth factors (e.g., HGF, IGF1, PDGF, EGF, and FGF), thereby promoting the proliferation and migration of vascular endothelial cells and enhancing angiogenesis71,79. Therefore, exosomes from different sources either directly affect endothelial cells or indirectly act on endothelial cells by upregulating the expression of angiogenesis-related growth factors, thus enhancing endothelial cell proliferation and migration and promoting the formation of new blood vessels.
Regulation of ECM remodeling and inhibition of scar formation
The remodeling phase, which is characterized by ECM remodeling and scar formation, is the last key phase in the wound healing process. An imbalance between the synthesis and degradation of ECM can prevent healing or lead to pathological scar formation80. Numerous exosomes, especially those released from MSCs, have been proven to be involved in the process of ECM remodeling. For example, hUMSC-Exos were found to facilitate the synthesis of elastin and collagen I81. In addition, exosomes derived from human-induced pluripotent stem cell-derived MSCs (hiPSC-MSCs) were demonstrated to promote the expression of collagen I, collagen III and elastin (Fig. S4A)24. Furthermore, endothelial cell-derived exosomes could facilitate the crosslinking of ECM by upregulating lysyl oxidase-like 2 (LOXL-2) under hypoxic conditions82. All these results indicate that exosomes exert their effect on ECM remodeling during wound healing. On the other hand, exosomes have also been found to suppress the excessive production of ECM components and overdifferentiation of fibroblasts into myofibroblasts to prevent scar formation and excessive repair. ADSC-Exos were found to inhibit scar formation by preventing fibroblasts from differentiating into myofibroblasts and regulating the TGF β3/TGF β1, collagen III/collagen I, and MMP3/TIMP1 ratios (Fig. S4B)83. In addition, hUMSC-Exos inhibited the formation of myofibroblasts by transporting specific microRNAs (e.g., miR-145, miR-125b, miR-23a, and miR-21) that target the TGF-β/SMAD2 signaling pathway (Fig. S4C)84. Therefore, exosomes may control collagen synthesis and myofibroblast differentiation at different stages of the wound healing process to achieve ideal wound repair.
Hydrogel-based delivery systems of exosomes in chronic wound treatment
Cell-derived exosomes have shown overwhelming potential in the field of regenerative medicine. However, many challenges in their use alone exist. For example, delivering exosomes at a therapeutic dosage to the target site, especially via systemic injection, is not a simple process. The direct application of exosomes through approaches such as intravenous, subcutaneous, or intraperitoneal injection often leads to rapid exosome clearance from the blood circulation and exosome accumulation in the liver, spleen, lung, and gastrointestinal tract85,86. Furthermore, macrophages in the reticuloendothelial system take up and release the majority of injected exosomes, regardless of the delivery method or cell source87. Therefore, maintaining exosome stability over time after transplantation is a central challenge for their clinical application, and sustained delivery of exosomes that increases their long-term efficiency and concentration is needed. In addition to controllable physicochemical properties, hydrogels with 3D networks have properties similar to those of the native ECM, such as good biocompatibility and biodegradability88. With these advantages, hydrogels have been widely applied to encapsulate and deliver drugs89,90,91, growth factors92,93,94, and other bioactive substances95,96, and have shown satisfactory delivery effects. Recently, many studies on the application of hydrogels for the delivery of exosomes in promoting wound repair have been reported (Table S2)27,29,74,97,98,99,100,101. In this section, we will introduce hydrogel-based exosome delivery systems.
Direct encapsulation of exosomes in hydrogels
To date, most hydrogel-based delivery systems have encapsulated exosomes directly in hydrogels. Exosomes are typically mixed with a polymer solution and crosslinking agents before hydrogel gelation or are incorporated into porous hydrogel scaffolds after hydrogel crosslinking. As the hydrogels degrade in vivo, the encapsulated exosomes are gradually released. For example, alginate (Alg)-based hydrogels were used to deliver ADSC-Exos for the repair of full-thickness skin defects28. The release of ADSC-Exos from an Alg-based hydrogel was sustained for 172 h, and more than 50% of the total exosome release was completed in the first 72 h, suggesting reliable and continuous delivery. Loading ADSC-Exos into an Alg-based hydrogel accelerated wound repair by promoting cell migration and proliferation, collagen deposition and angiogenesis in comparison with wound repair in the untreated control group and the group treated with Alg alone. In addition, specific degradation-sensitive hydrogels have been developed to more efficiently deliver exosomes in different microenvironments. Loading of a thermosensitive chitosan (CS) hydrogel with exosomes from human placenta-derived MSCs (hP-MSCs) improved their retention and stability in vivo (Fig. 6A)102. Labeled exosomes gradually increased both in the surroundings after incubation with CS-Exos at 37 °C in vitro and in mouse ischemic hindlimbs after the injection of CS-Exos in vivo, suggesting sustained release of thermosensitive CS-Exos. This approach enhanced the stability of exosomes derived from hP-MSCs and improved their therapeutic effects, thus facilitating tissue repair after ischemic injury. Zhou et al. introduced an MMP2-sensitive self-assembling peptide (KMP2) hydrogel containing an MMP2-cleavable motif for the treatment of ischemia‒reperfusion (I/R) injury (Fig. 6B)103. Due to enzymatic degradation by MMP2, the network structure of the KMP2 hydrogel was destroyed, and the loaded EVs were then released. In response to MMP2, the KMP2 hydrogel increased mass loss and accelerated the release of MSC-EVs, demonstrating controlled release of EVs from the KMP2 hydrogel. Moreover, the released EVs maintained their properties, such as their antiapoptotic (e.g., Fas and Bax) and anti-inflammatory (e.g., MCP-1, IL-1β, and ICAM-1) potency in HK2 cells under hypoxia-reoxygenation (H/R) conditions in vivo.
A Thermosensitive chitosan (CS) hydrogel for the sustained release of exosomes from hP-MSCs. (a) Optical images of the CS solution (I) and hydrogel (II). (b) Scanning electron microscopy image of the CS hydrogel. (c) The rheological properties of the CS hydrogel with temperature changes were analyzed by rheological measurements. (d) Sustained release of Exos from the CS hydrogel was tested by tracking Gluc signals using bioluminescence imaging (BLI) analysis. (e) In vivo monitoring of the retention of transplanted CS-Exos or Exos through the tracking of Gluc signals by BLI analysis. (f) The stability of the main functional molecule miR-126 in CS-Exos or Exos at 37 °C was assessed by real-time qPCR analysis. (g) Quantitative analysis of Gluc signals indicated the retention of Exos in (e). *p < 0.05, **p < 0.01. Reproduced with permission102. Copyright 2018, American Chemical Society. B MMP2-sensitive KMP2 hydrogel for the controlled release of MSC-EVs. (a) Schematic illustration of the KMP2 hydrogel for enhanced EV release and tissue repair. (b) Degradation of the KMP2 hydrogel with or without MMP2 was measured by gel mass loss. (c) In vitro release of EVs from KMP2 hydrogels in PBS or an MMP2 solution (0.4 or 4 mg/ml, n = 3). *p < 0.05, **p < 0.01, PBS group vs. MMP2_0.4 group; #p < 0.05, ##p < 0.01, PBS group vs. MMP2_4 group; &p < 0.05, &&p < 0.01, MMP2_0.4 group vs. MMP2_4 group. (d) Real-time PCR analysis of Bax and Fas mRNA levels in HK2 cells. (e) Western blot analysis of ICAM-1 and IL-1β protein levels in HK2 cells. HK2 cells were exposed to hypoxia-reoxygenation (H/R) and were treated with 10 μg protein/ml fresh EVs or released EVs. *p < 0.05, **p < 0.01, H/R group vs. Con group; #p < 0.05, ##p < 0.01, Fresh EVs group vs. H/R group. Reproduced with permission103. Copyright 2019, Elsevier.
Encapsulation of exosomes in hydrogels through physical/chemical interactions
In addition to the direct incorporation of exosomes into hydrogels, some researchers have used physical or chemical interactions to implement the encapsulation of exosomes in hydrogels and their release. For instance, Pluronic F127 grafting polyethylenimine (PEI) and aldehyde pullulan (APu) were used to synthesize a polysaccharide-based FEP hydrogel by a Schiff base reaction; ADSC-derived exosomes were encapsulated into the hydrogel via electrostatic interactions and were released in a pH-responsive manner (Fig. 7A)104. Although sustained exosome release by FEP hydrogel was observed for 21 days, faster exosome release occurred at pH 5.5 than at pH 7.5 due to the presence of a pH-sensitive C=N bond in the FEP hydrogel. In addition, Helena et al. encapsulated PCL-modified small extracellular vesicles (SEVs) in cysteine-modified hyaluronic acid (HA) through chemical interactions between the terminal acrylate groups on PCL and the thiol groups on HA, yielding a light-triggerable HA hydrogel containing SEVs (Fig. 7B)105. Due to the formation of a photolabile orthonitrobenzyl ester bond, controlled release of the SEVs could be achieved upon UV/blue light irradiation. In addition, release of the SEVs was dependent on the number of irradiations and the exposure time. A significant difference in full-thickness wound repair was observed in animals treated with the HA hydrogel+EVs+light irradiation group compared with the control groups, indicating improved wound healing with the controlled release system. Overall, the utilization of hydrogels as exosome delivery systems may be a promising way to achieve sustained therapeutic effects on chronic wounds.
A ADSC-derived exosomes were loaded in an FEP hydrogel through electrostatic interactions and released in response to pH changes. (a) Schematic illustration of the synthesis of a multifunctional FEP hydrogel scaffold. (b) Schematic of exosome release from the FEP scaffold dressing. (c) Representative pH-dependent release profile of loaded exosomes in the FHE scaffold dressing. Reproduced with permission104. Copyright 2019, American Chemical Society. B Light-triggerable HA hydrogel for the controlled release of SEVs. (a) Schematic illustration of the formation of the light-triggerable HA hydrogel containing SEVs (hydrogel is translucid: a1, swollen gel in PBS; a2, swollen gel in DMEM). Photocleavage of the HA hydrogel over time demonstrating that the release of SEVs was dependent on (b) the number of irradiations and (c) the exposure time. *p < 0.05, **p < 0.01, ***p < 0.001, UV-light group vs. nonirradiated group; #p < 0.05, ##p < 0.01, ###p < 0.001, blue-light group vs. nonirradiated group. Reproduced with permission105. Copyright 2019, American Chemical Society.
Conclusion and future perspectives
For decades, exosomes have been widely exploited to develop novel strategies for tissue regeneration, drug delivery, and disease diagnosis and treatment106. Among exosomes derived from biological sources, MSC-derived exosomes have shown great promise in the field of regenerative medicine, as they can inherit most of the regenerative effects of MSCs107. As drug carriers, exosomes and liposomes have complementary advantages and disadvantages. Liposomes are commonly used nanoparticle-based drug delivery systems due to their high biocompatibility and low toxicity. Liposomes are composed of phospholipids and cholesterol, which are the main components of cell membranes, making them the first artificial drug carriers to receive clinical approval108. To date, liposomes with the advantages of high loading and good protection for drugs have been able to meet the requirements of commercial mass production. However, problems with immunogenicity and poor targeting still restrain the application of liposomes for ideal drug delivery109. In comparison, exosomes, as natural vesicles released by cells, have great immune compatibility. Moreover, with a variety of proteins on their membranes (e.g., tetraspinins), exosomes are provided with high and specific organotropism, which is one of the major goals of all types of nanoparticle-based drug delivery systems. It is worth noting that there are also some disadvantages of exosomes as drug carriers, such as insufficient productivity, low drug load, and high clearance rate in the circulation110. Therefore, the development of various types of designed exosomes or liposome-based artificial exosomes for targeted drug delivery is currently under in-depth study111. In the field of wound repair, exosomes transport a variety of bioactive contents and participate in almost the entire wound healing process; for example, they regulate inflammatory responses, promote cell proliferation and migration, boost angiogenesis, and regulate ECM remodeling. All these findings have proven that cell-derived exosomes have great potential as therapeutic strategies for chronic wound healing. However, some challenges still remain. We conclude with some opinions on the extraction and purification of exosomes, the safety and application of exosomes, the regulatory effects of microenvironmental cues on cell-derived exosomes, and exosome delivery systems.
-
1.
The ultimate goal of the use of exosomes is to achieve clinical therapeutic results, but there is still a long way to go. First, the insufficient production of exosomes is the most vital problem. Traditional approaches for the extraction and purification of exosomes are quite complex. Some recently developed techniques, such as EXODUS112, can achieve ultrafast isolation of exosomes from biofluids with high purity and high yield. Second, standards related to vesicle size, purity, and contamination levels and identification of specific biomarkers are lacking. Methods to distinguish exosomes based on cell source have not been developed, and a proteomic analysis of exosomes has not been carried out. Finally, any clinical applications must be based on safety. However, as of now, studies assessing the safety of exosome-based therapies are in their infancy, and many uncertainties regarding their safety remain. For example, the pro- and anticancer effects of exosomes in different applications are still controversial. Exosomes may accelerate cancer progression through direct interactions or by secreting various factors113. Further studies are necessary to determine the effective dose range for the safe clinical application of exosomes.
-
2.
Heterogeneity among exosomes due to their diverse origins is a crucial issue that cannot be ignored. Even among exosomes from the same kind of cells or biospecimens, it is not clear whether exosomes differ among individuals. In addition, the extracellular microenvironment can influence cell secretion51. Cell-derived exosomes can inherit the adaptive changes of their parental cells in response to environmental features and mainly show changes in their production, quality and the components that they encapsulate; such changes can influence the therapeutic efficiency of exosomes. Cell preconditioning may be a way to resolve this issue. We have summarized the regulatory effects of some biochemical and biophysical cues in the extracellular microenvironment on the features of exosomes. Hence, it is possible to regulate the biological functions of cell-derived exosomes by altering the cell microenvironment to promote therapeutic efficiency or even achieve personalized treatments, which is an emerging area that may serve as a research focus for future studies.
-
3.
To enhance therapeutic efficiency, hydrogel-based delivery systems for the sustained and precise release of exosomes during treatment have been developed. Stimulus-responsive hydrogels may provide customizable methods of exosome delivery. However, the clinical application of hydrogel-based delivery systems in vivo still faces many challenges. For example, residual crosslinkers or components in hydrogels are toxic and carcinogenic. Uncontrollable crosslinking of pH- or temperature-sensitive hydrogels can occur, which can block the needle during injection. Therefore, it is necessary to optimize the conditions under which the gel forms to prevent premature gel formation. In addition, the release profiles of hydrogel-based delivery systems determined in vitro may not be applicable to in vivo applications. The effects of the in vivo microenvironment on delivery efficiency still need to be explored.
Change history
12 October 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41427-023-00503-x
References
Rice, J. B. et al. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care 37, 651–658 (2014).
Martinengo, L. et al. Prevalence of chronic wounds in the general population: systematic review and meta-analysis of observational studies. Ann. Epidemiol. 29, 8–15 (2019).
Olsson, M. et al. The humanistic and economic burden of chronic wounds: a systematic review. Wound Repair Regen. 27, 114–125 (2019).
Frykberg, R. G. & Banks, J. Challenges in the treatment of chronic wounds. Adv. Wound Care. 4, 560–582 (2015).
Akopian, G. et al. Outcomes of conventional wound treatment in a comprehensive wound center. Am. Surg. 72, 314–317 (2006).
Nunan, R., Harding, K. G. & Martin, P. Clinical challenges of chronic wounds: searching for an optimal animal model to recapitulate their complexity. Dis. Model Mech. 7, 1205–1213 (2014).
Chou, P.-R. et al. Supercritical carbon dioxide-decellularized porcine acellular dermal matrix combined with autologous adipose-derived stem cells: its role in accelerated diabetic wound healing. Int. J. Med. Sci. 17, 354–367 (2020).
Boeringer, T., Gould, L. J. & Koria, P. Protease-resistant growth factor formulations for the healing of chronic wounds. Adv. Wound Care. 9, 612–622 (2020).
Oneto, P. & Etulain, J. PRP in wound healing applications. Platelets 32, 189–199 (2020).
Huang, Y.-Z., Gou, M., Da, L.-C., Zhang, W.-Q. & Xie, H.-Q. Mesenchymal stem cells for chronic wound healing: current status of preclinical and clinical studies. Tissue Eng. Part B Rev. 26, 555–570 (2020).
Shin, L. & Peterson, D. A. Human mesenchymal stem cell grafts enhance normal and impaired wound healing by recruiting existing endogenous tissue stem/progenitor cells. Stem Cells Transl. Med. 2, 33–42 (2013).
Volarevic, V. et al. Ethical and safety issues of stem cell-based therapy. Int. J. Med. Sci. 15, 36–45 (2018).
Song, Y. et al. Human umbilical cord blood-derived MSCs exosome attenuate myocardial injury by inhibiting ferroptosis in acute myocardial infarction mice. Cell Biol. Toxicol. 37, 51–64 (2020).
Liu, W. et al. Hypoxic mesenchymal stem cell-derived exosomes promote bone fracture healing by the transfer of miR-126. Acta Biomater. 103, 196–212 (2020).
Ferreira, Ad. F. & Gomes, D. A. Stem cell extracellular vesicles in skin repair. Bioengineering 6, 4 (2018).
Kalluri, R. & LeBleu, V. S. The biology, function, and biomedical applications of exosomes. Science 367, eaau6977 (2020).
El Andaloussi, S., Mäger, I., Breakefield, X. O. & Wood, M. J. A. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat. Rev. Drug Discov. 12, 347–357 (2013).
Xu, J., Camfield, R. & Gorski, S. M. The interplay between exosomes and autophagy—partners in crime. J. Cell Sci. 131, jcs215210 (2018).
Hood, J. L. & Wickline, S. A. A systematic approach to exosome-based translational nanomedicine. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 4, 458–467 (2012).
Colombo, M., Raposo, G. & Théry, C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu. Rev. Cell Dev. Biol. 30, 255–289 (2014).
Schorey, J. S. & Harding, C. V. Extracellular vesicles and infectious diseases: new complexity to an old story. J. Clin. Investig. 126, 1181–1189 (2016).
Najrana, T. et al. Mechanical stretch regulates the expression of specific miRNA in extracellular vesicles released from lung epithelial cells. J. Cell. Physiol. 235, 8210–8223 (2020).
Han, Y., Ren, J., Bai, Y., Pei, X. & Han, Y. Exosomes from hypoxia-treated human adipose-derived mesenchymal stem cells enhance angiogenesis through VEGF/VEGF-R. Int. J. Biochem. Cell Biol. 109, 59–68 (2019).
Zhang, J. et al. Exosomes released from human induced pluripotent stem cells-derived MSCs facilitate cutaneous wound healing by promoting collagen synthesis and angiogenesis. J. Transl. Med. 13, 49 (2015).
Zhang, J. et al. Exosomes derived from human endothelial progenitor cells accelerate cutaneous wound healing by promoting angiogenesis through Erk1/2 signaling. Int. J. Biol. Sci. 12, 1472–1487 (2016).
Hu, L. et al. Exosomes derived from human adipose mensenchymal stem cells accelerates cutaneous wound healing via optimizing the characteristics of fibroblasts. Sci. Rep. 6, 32993 (2016).
Tao, S. C. et al. Chitosan wound dressings incorporating exosomes derived from microRNA-126-overexpressing synovium mesenchymal stem cells provide sustained release of exosomes and heal full-thickness skin defects in a diabetic rat model. Stem Cells Transl. Med. 6, 736–747 (2017).
Shafei, S. et al. Exosome loaded alginate hydrogel promotes tissue regeneration in full-thickness skin wounds: an in vivo study. J. Biomed. Mater. Res. A. 108, 545–556 (2020).
Wang, C. et al. Engineering bioactive self-healing antibacterial exosomes hydrogel for promoting chronic diabetic wound healing and complete skin regeneration. Theranostics 9, 65–76 (2019).
Schorey, J. S. & Bhatnagar, S. Exosome function: from tumor immunology to pathogen biology. Traffic 9, 871–881 (2008).
Li, X. et al. Exosomes from adipose-derived stem cells overexpressing Nrf2 accelerate cutaneous wound healing by promoting vascularization in a diabetic foot ulcer rat model. Exp. Mol. Med. 50, 29 (2018).
Wang, X. et al. Cardiomyocytes mediate anti-angiogenesis in type 2 diabetic rats through the exosomal transfer of miR-320 into endothelial cells. J. Mol. Cell Cardiol. 74, 139–150 (2014).
Haraszti, R. A. et al. Serum deprivation of mesenchymal stem cells improves exosome activity and alters lipid and protein composition. iScience 16, 230–241 (2019).
Gray, W. D. et al. Identification of therapeutic covariant microRNA clusters in hypoxia-treated cardiac progenitor cell exosomes using systems biology. Circ. Res. 116, 255–263 (2015).
Eldh, M. et al. Exosomes communicate protective messages during oxidative stress; possible role of exosomal shuttle RNA. PLoS One 5, e15353 (2010).
Dougherty, J. A. et al. Human cardiac progenitor cells enhance exosome release and promote angiogenesis under physoxia. Front. Cell Dev. Biol. 8, 130 (2020).
Gonzalez-King, H. et al. Hypoxia inducible factor-1α potentiates jagged 1-mediated angiogenesis by mesenchymal stem cell-derived exosomes. Stem Cells 35, 1747–1759 (2017).
Du, W. et al. Enhanced proangiogenic potential of mesenchymal stem cell-derived exosomes stimulated by a nitric oxide releasing polymer. Biomaterials 133, 70–81 (2017).
Busbee, P. B., Nagarkatti, M. & Nagarkatti, P. S. Natural indoles, indole-3-carbinol (I3C) and 3,3’-diindolylmethane (DIM), attenuate staphylococcal enterotoxin B-mediated liver injury by downregulating miR-31 expression and promoting caspase-2-mediated apoptosis. PLoS ONE 10, e0118506 (2015).
Elliott, D. M., Nagarkatti, M. & Nagarkatti, P. S. 3,39-Diindolylmethane ameliorates staphylococcal enterotoxin B–induced acute lung injury through alterations in the expression of microRNA that target apoptosis and cell-cycle arrest in activated T cells. J. Pharmacol. Exp. Ther. 357, 177–187 (2016).
Shi, H. et al. 3,3’-Diindolylmethane stimulates exosomal Wnt11 autocrine signaling in human umbilical cord mesenchymal stem cells to enhance wound healing. Theranostics 7, 1674–1688 (2017).
Thompson, C. A., Purushothaman, A., Ramani, V. C., Vlodavsky, I. & Sanderson, R. D. Heparanase regulates secretion, composition, and function of tumor cell-derived exosomes. J. Biol. Chem. 288, 10093–10099 (2013).
Zuo, L. L. et al. Cadherin 6 is activated by Epstein-Barr virus LMP1 to mediate EMT and metastasis as an interplay node of multiple pathways in nasopharyngeal carcinoma. Oncogenesis 6, 402 (2017).
Zuo, L. et al. Targeting exosomal EBV-LMP1 transfer and miR-203 expression via the NF-κB pathway: the therapeutic role of aspirin in NPC. Mol. Ther. Nucleic Acids 17, 175–184 (2019).
Kulshreshtha, A. et al. Simvastatin mediates inhibition of exosome synthesis, localization and secretion via multicomponent interventions. Sci. Rep. 9, 16373 (2019).
Lopatina, T. et al. Platelet-derived growth factor regulates the secretion of extracellular vesicles by adipose mesenchymal stem cells and enhances their angiogenic potential. Cell Commun. Signal. 12, 26 (2014).
Wang, R., Xu, B. & Xu, H. TGF-β1 promoted chondrocyte proliferation by regulating Sp1 through MSC-exosomes derived miR-135b. Cell Cycle 17, 2756–2765 (2018).
Kao, J.-K. et al. Heat-shock pretreatment reduces expression and release of TSLP from keratinocytes under Th2 environment. Pediatr. Allergy Immunol. 27, 62–69 (2016).
Jelonek, K., Widlak, P. & Pietrowska, M. The influence of ionizing radiation on exosome composition, secretion and intercellular communication. Protein Pept. Lett. 23, 656–663 (2016).
Villasante, A. et al. Recapitulating the size and cargo of tumor exosomes in a tissue-engineered model. Theranostics 6, 1119–1130 (2016).
Haraszti, R. A. et al. Exosomes produced from 3D cultures of MSCs by tangential flow filtration show higher yield and improved activity. Mol. Ther. 26, 2838–2847 (2018).
Kim, M., Yun, H.-W., Park, D. Y., Choi, B. H. & Min, B.-H. Three-dimensional spheroid culture increases exosome secretion from mesenchymal stem cells. Tissue Eng. Regen. Med. 15, 427–436 (2018).
Gollmann-Tepeköylü, C. et al. miR-19a-3p containing exosomes improve function of ischaemic myocardium upon shock wave therapy. Cardiovasc. Res. 116, 1226–1236 (2020).
Pironti, G. et al. Circulating exosomes induced by cardiac pressure overload contain functional angiotensin II type 1 receptors. Circulation 131, 2120–2130 (2015).
Jeon, H. et al. Extracellular vesicles from KSHV-infected endothelial cells activate the complement system. Oncotarget 8, 99841–99860 (2017).
Park, S. J., Jeon, H., Yoo, S.-M. & Lee, M.-S. The effect of storage temperature on the biological activity of extracellular vesicles for the complement system. Vitr. Cell. Dev. Biol. Anim. 54, 423–429 (2018).
Li, X., Li, X., Lin, J., Sun, X. & Ding, Q. Exosomes derived from low-intensity pulsed ultrasound-treated dendritic cells suppress tumor necrosis factor-induced endothelial inflammation. J. Ultrasound Med. 38, 2081–2091 (2019).
Arscott, W. T. et al. Ionizing radiation and glioblastoma exosomes: implications in tumor biology and cell migration. Transl. Oncol. 6, 638–648 (2013).
Valadi, H. et al. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 9, 654–659 (2007).
Bruno, S. et al. Mesenchymal stem cell-derived microvesicles protect against acute tubular injury. J. Am. Soc. Nephrol. 20, 1053–1067 (2009).
Gatti, S. et al. Microvesicles derived from human adult mesenchymal stem cells protect against ischaemia-reperfusion-induced acute and chronic kidney injury. Nephrol. Dial. Transpl. 26, 1474–1483 (2011).
Lai, R. C. et al. Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury. Stem Cell Res. 4, 214–222 (2010).
Ranghino, A. et al. Endothelial progenitor cell-derived microvesicles improve neovascularization in a murine model of hindlimb ischemia. Int. J. Immunopathol. Pharmacol. 25, 75–85 (2012).
Zhao, R., Liang, H., Clarke, E., Jackson, C. & Xue, M. Inflammation in chronic wounds. Int. J. Mol. Sci. 17, 2085 (2016).
Li, M. et al. Macrophage-derived exosomes accelerate wound healing through their anti-inflammation effects in a diabetic rat model. Artif. Cells Nanomed. Biotechnol. 47, 3793–3803 (2019).
Kim, H. et al. Exosome-guided phenotypic switch of M1 to M2 macrophages for cutaneous wound healing. Adv. Sci. 6, 1900513 (2019).
Ti, D. et al. LPS-preconditioned mesenchymal stromal cells modify macrophage polarization for resolution of chronic inflammation via exosome-shuttled let-7b. J. Transl. Med. 13, 308 (2015).
Li, X. et al. Exosome derived from human umbilical cord mesenchymal stem cell mediates MiR-181c attenuating burn-induced excessive inflammation. EBioMedicine 8, 72–82 (2016).
Singer, A. J. & Clark, R. A. Cutaneous wound healing. N. Engl. J. Med. 341, 738–746 (1999).
Yang, C. et al. Highly-expressed micoRNA-21 in adipose derived stem cell exosomes can enhance the migration and proliferation of the HaCaT cells by increasing the MMP-9 expression through the PI3K/AKT pathway. Arch. Biochem. Biophys. 681, 108259 (2020).
Shabbir, A., Cox, A., Rodriguez-Menocal, L., Salgado, M. & Van Badiavas, E. Mesenchymal stem cell exosomes induce proliferation and migration of normal and chronic wound fibroblasts, and enhance angiogenesis in vitro. Stem Cells Dev. 24, 1635–1647 (2015).
Zhang, B. et al. HucMSC-exosome mediated-Wnt4 signaling is required for cutaneous wound healing. Stem Cells 33, 2158–2168 (2015).
Zhang, B. et al. HucMSC exosome-delivered 14-3-3ζ orchestrates self-control of the Wnt response via modulation of YAP during cutaneous regeneration. Stem Cells 34, 2485–2500 (2016).
Guo, S. C. et al. Exosomes derived from platelet-rich plasma promote the re-epithelization of chronic cutaneous wounds via activation of YAP in a diabetic rat model. Theranostics 7, 81–96 (2017).
Kota, S. K. et al. Aberrant angiogenesis: the gateway to diabetic complications. Indian J. Endocr. Metab. 16, 918–930 (2012).
Chen, C. Y. et al. Exosomal DMBT1 from human urine-derived stem cells facilitates diabetic wound repair by promoting angiogenesis. Theranostics 8, 1607–1623 (2018).
Liang, X., Zhang, L., Wang, S., Han, Q. & Zhao, R. C. Exosomes secreted by mesenchymal stem cells promote endothelial cell angiogenesis by transferring miR-125a. J. Cell Sci. 129, 2182–2189 (2016).
Gong, M. et al. Mesenchymal stem cells release exosomes that transfer miRNAs to endothelial cells and promote angiogenesis. Oncotarget 8, 45200–45212 (2017).
Anderson, J. D. et al. Comprehensive proteomic analysis of mesenchymal stem cell exosomes reveals modulation of angiogenesis via nuclear factor-kappaB signaling. Stem Cells 34, 601–613 (2016).
Xue, M. & Jackson, C. J. Extracellular matrix reorganization during wound healing and its impact on abnormal scarring. Adv. Wound Care. 4, 119–136 (2015).
Kim, Y.-J. et al. Exosomes derived from human umbilical cord blood mesenchymal stem cells stimulates rejuvenation of human skin. Biochem. Biophys. Res. Commun. 493, 1102–1108 (2017).
Jong, O. G., Balkom, B. W. M., Gremmels, H. & Verhaar, M. C. Exosomes from hypoxic endothelial cells have increased collagen crosslinking activity through up‐regulation of lysyl oxidase‐like 2. J. Cell. Mol. Med. 20, 342–350 (2016).
Wang, L. et al. Exosomes secreted by human adipose mesenchymal stem cells promote scarless cutaneous repair by regulating extracellular matrix remodelling. Sci. Rep. 7, 13321 (2017).
Fang, S. et al. Umbilical cord-derived mesenchymal stem cell-derived exosomal microRNAs suppress myofibroblast differentiation by inhibiting the transforming growth factor-β/SMAD2 pathway during wound healing. Stem Cells Transl. Med. 5, 1425–1439 (2016).
Takahashi, Y. et al. Visualization and in vivo tracking of the exosomes of murine melanoma B16-BL6 cells in mice after intravenous injection. J. Biotechnol. 165, 77–84 (2013).
Smyth, T. et al. Biodistribution and delivery efficiency of unmodified tumor-derived exosomes. J. Control. Release 199, 145–155 (2015).
Wiklander, O. P. B. et al. Extracellular vesicle in vivo biodistribution is determined by cell source, route of administration and targeting. J. Extracell. Vesicles. 4, 26316 (2015).
Annabi, N. et al. 25th anniversary article: rational design and applications of hydrogels in regenerative medicine. Adv. Mater. 26, 85–123 (2014).
Chen, X. et al. Magnetic and self-healing chitosan-alginate hydrogel encapsulated gelatin microspheres via covalent cross-linking for drug delivery. Mat. Sci. Eng. C.-Mater. 101, 619–629 (2019).
Mahanta, A. K. et al. Nanoparticle-induced controlled drug delivery using chitosan-based hydrogel and scaffold: application to bone regeneration. Mol. Pharm. 16, 327–338 (2019).
Wei, W. et al. Synthesis and characterization of a multi-sensitive polysaccharide hydrogel for drug delivery. Carbohyd. Polym. 177, 275–283 (2017).
Neuerburg, C. et al. Growth factor-mediated augmentation of long bones: evaluation of a BMP-7 loaded thermoresponsive hydrogel in a murine femoral intramedullary injection model. J. Orthop. Surg. Res. 14, 297 (2019).
Chan, S. J. et al. Promoting neuro-supportive properties of astrocytes with epidermal growth factor hydrogels. Stem Cells Transl. Med. 8, 1242–1248 (2019).
Zhang, X. et al. Stimulation of wound healing using bioinspired hydrogels with basic fibroblast growth factor (bFGF). Int. J. Nanomed. 13, 3897–3906 (2018).
Ding, L. et al. A self-assembled RNA-triple helix hydrogel drug delivery system targeting triple-negative breast cancer. J. Mater. Chem. B. 8, 3527–3533 (2020).
Chen, Z. et al. Targeted delivery of CRISPR/Cas9-mediated cancer gene therapy via liposome-templated hydrogel nanoparticles. Adv. Funct. Mater. 27, 1703036 (2017).
Xu, N. et al. Wound healing effects of a Curcuma zedoaria polysaccharide with platelet-rich plasma exosomes assembled on chitosan/silk hydrogel sponge in a diabetic rat model. Int. J. Biol. Macromol. 117, 102–107 (2018).
Wang, C. et al. The fabrication of a highly efficient self-healing hydrogel from natural biopolymers loaded with exosomes for the synergistic promotion of severe wound healing. Biomater. Sci. 8, 313–324 (2019).
Zhang, Y. et al. Preparation of exosomes encapsulated nanohydrogel for accelerating wound healing of diabetic rats by promoting angiogenesis. Mat. Sci. Eng. C.-Mater. 120, 111671 (2021).
Shi, Q. et al. GMSC-derived exosomes combined with a chitosan/silk hydrogel sponge accelerates wound healing in a diabetic rat skin defect model. Front. Physiol. 8, 904 (2017).
Zhao, D. et al. GelMA combined with sustained release of HUVECs derived exosomes for promoting cutaneous wound healing and facilitating skin regeneration. J. Mol. Histol. 51, 251–263 (2020).
Zhang, K. et al. Enhanced therapeutic effects of mesenchymal stem cell-derived exosomes with an injectable hydrogel for hindlimb ischemia treatment. ACS Appl. Mater. Inter. 10, 30081–30091 (2018).
Zhou, Y. et al. Injectable extracellular vesicle-released self-assembling peptide nanofiber hydrogel as an enhanced cell-free therapy for tissue regeneration. J. Control. Release 316, 93–104 (2019).
Wang, M. et al. Efficient angiogenesis-based diabetic wound healing/skin reconstruction through bioactive antibacterial adhesive ultraviolet shielding nanodressing with exosome release. ACS Nano 13, 10279–10293 (2019).
Henriques-Antunes, H. et al. The kinetics of small extracellular vesicle delivery impacts skin tissue regeneration. ACS Nano 13, 8694–8707 (2019).
He, C., Zheng, S., Luo, Y. & Wang, B. Exosome theranostics: biology and translational medicine. Theranostics 8, 237–255 (2018).
Rani, S., Ryan, A. E., Griffin, M. D. & Ritter, T. Mesenchymal stem cell-derived extracellular vesicles: toward cell-free therapeutic applications. Mol. Ther. 23, 812–823 (2015).
Almeida, B., Nag, O. K., Rogers, K. E. & Delehanty, J. B. Recent progress in bioconjugation strategies for liposome-mediated drug delivery. Molecules 25, 5672 (2020).
Allen, T. M. & Cullis, P. R. Liposomal drug delivery systems: from concept to clinical applications. Adv. Drug Deliv. Rev. 65, 36–48 (2013).
Zhang, Y. et al. Exosome: a review of its classification, isolation techniques, storage, diagnostic and targeted therapy applications. Int. J. Nanomed. 15, 6917–6934 (2020).
Antimisiaris, S. G., Mourtas, S. & Marazioti, A. Exosomes and exosome-inspired vesicles for targeted drug delivery. Pharmaceutics 10, 218 (2018).
Chen, Y. et al. Exosome detection via the ultrafast-isolation system: EXODUS. Nat. Methods 18, 212–218 (2021).
Lin, R., Wang, S. & Zhao, R. C. Exosomes from human adipose-derived mesenchymal stem cells promote migration through Wnt signaling pathway in a breast cancer cell model. Mol. Cell. Biochem. 383, 13–20 (2013).
Acknowledgements
This work was supported by the National Natural Science Foundation of China (11972279), the Young Elite Scientist Sponsorship Program by CAST (2018QNRC001), and the Natural Science Foundation of Shaanxi Province (2020JQ-060).
Author information
Authors and Affiliations
Contributions
W.D., J.L., and Y.M. contributed to the paper design, figure and table preparation, and paper editing and revision. Y.D. and J.W. contributed to figure preparation. T.H. contributed to the literature collection. B.G., H.G., and F.X. contributed to the review of the paper.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dai, W., Dong, Y., Han, T. et al. Microenvironmental cue-regulated exosomes as therapeutic strategies for improving chronic wound healing. NPG Asia Mater 14, 75 (2022). https://doi.org/10.1038/s41427-022-00419-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41427-022-00419-y