Abstract
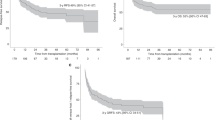
We present a single-center retrospective series of allogeneic bone marrow transplantation (BMT) with the use of posttransplant cyclophosphamide (PTCy) in the setting of nonmalignant hematological conditions. Nine patients were treated between 2013 and 2019. Nonmyeloablative conditioning consisted of antithymocyte globulin, fludarabine, low-dose cyclophosphamide, and total body irradiation (200cGy) followed by allogeneic bone marrow infusion. Post-BMT GVHD prophylaxis was with PTCy, tacrolimus, and mycophenolate mofetil. At a median follow-up of 24 months (range 4, 63), all patients are alive, with donor-derived hematopoiesis and free of significant acute or chronic GVHD. Donors were haploidentical (n = 6), fully matched unrelated (n = 2), and fully matched sibling (n = 1). Neutrophil and platelet engraftment occurred at a median of 21 days and 33 days, respectively, after transplantation. Three patients (3/9, 33%) experienced stage 1–2 acute skin GVHD. The only cases of chronic GVHD are in three patients (3/9, 33%) with ocular disease (two mild, one moderate). No patient has required systemic immunosuppression beyond 12 months after BMT. PTCy-based nonmyeloablative allogeneic BMT is safe and effective for nonmalignant hematologic conditions and should be prospectively compared with historical regimens.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Storb R, Thomas ED, Buckner CD, Clift RA, Johnson FL, Fefer A, et al. Allogeneic marrow grafting for treatment of aplastic anemia. Blood. 1974;43:157–80.
Tolar J, Sodani P, Symons H. Alternative donor transplant of benign primary hematologic disorders. Bone Marrow Transplant. 2015;50:619.
Georges GE, Doney K, Storb R. Severe aplastic anemia: allogeneic bone marrow transplantation as first-line treatment. Blood Adv. 2018;2:2020–8.
O’Boyle F, Bradshaw A, Szydlo RM, de la Fuente J. Haemopoietic stem cell transplantation for diamond blackfan anaemia leads to early and sustained engraftment with good long-term outcomes, but has an increased risk of gut toxicity and lung gvhD. Blood. 2016;128:2679.
Kasamon YL, Bolaños-Meade J, Prince GT, Tsai H-L, McCurdy SR, Kanakry JA, et al. Outcomes of nonmyeloablative HLA-haploidentical blood or marrow transplantation with high-dose post-transplantation cyclophosphamide in older adults. J Clin Oncol. 2015;33:3152–61.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–50.
Bachegowda LS, Shah MV, Veltri LW, Tanase A, Popat U, Anderlini P, et al. HLA-mismatched bone marrow transplantation in severe aplastic anemia. Bone Marrow Transplant. 2017;52:1347.
Bolaños-Meade J, Reshef R, Fraser R, Fei M, Abhyankar S, Al-Kadhimi Z, et al. Three prophylaxis regimens (tacrolimus, mycophenolate mofetil, and cyclophosphamide; tacrolimus, methotrexate, and bortezomib; or tacrolimus, methotrexate, and maraviroc) versus tacrolimus and methotrexate for prevention of graft-versus-host disease with haemopoietic cell transplantation with reduced-intensity conditioning: a randomised phase 2 trial with a non-randomised contemporaneous control group (BMT CTN 1203). Lancet Haematol. 2019;6:e132–43.
Tisdale JF, Eapen M, Saccardi R. HCT for nonmalignant disorders. Biol Blood Marrow Transplant. 2013;19:S6–9.
Bolaños-Meade J, Fuchs EJ, Luznik L, Lanzkron SM, Gamper CJ, Jones RJ, et al. HLA-haploidentical bone marrow transplantation with posttransplant cyclophosphamide expands the donor pool for patients with sickle cell disease. Blood. 2012;120:4285.
DeZern AE, Zahurak M, Symons H, Cooke K, Jones RJ, Brodsky RA. Alternative Donor Transplantation with High-Dose Post-Transplantation Cyclophosphamide for Refractory Severe Aplastic Anemia. Biol Blood Marrow Transplant. 2017;23:498–504.
Harris AC, Young R, Devine S, Hogan WJ, Ayuk F, Bunworasate U, et al. International, multicenter standardization of acute graft-versus-host disease clinical data collection: a report from the mount sinai acute gvhd international consortium. Biol Blood Marrow Transplant. 2016;22:4–10.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11:945–56.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Bacigalupo A, Hows J, Gordon-Smith EC, Gluckman E, Van Lint MT, Congiu M, et al. Bone marrow transplantation for severe aplastic anemia from donors other than HLA identical siblings: a report of the BMT Working Party. Bone Marrow Transplant. 1988;3:531–5.
Perez-Albuerne ED, Eapen M, Klein J, Gross TJ, Lipton JM, Baker KS, et al. Outcome of unrelated donor stem cell transplantation for children with severe aplastic anemia. Br J Haematol. 2008;141:216–23.
Horan J, Wang T, Haagenson M, Spellman SR, Dehn J, Eapen M, et al. Evaluation of HLA matching in unrelated hematopoietic stem cell transplantation for nonmalignant disorders. Blood. 2012;120:2918–24.
Deeg HJ, O’Donnell M, Tolar J, Agarwal R, Harris RE, Feig SA, et al. Optimization of conditioning for marrow transplantation from unrelated donors for patients with aplastic anemia after failure of immunosuppressive therapy. Blood. 2006;108:1485–91.
Passweg JR, Baldomero H, Bader P, Basak GW, Bonini C, Duarte R, et al. Is the use of unrelated donor transplantation leveling off in Europe? The 2016 European Society for Blood and Marrow Transplant activity survey report. Bone Marrow Transplant. 2018;53:1139–48.
Bacigalupo A. Alternative donor transplants for severe aplastic anemia. ASH Educ Program Book. 2018;2018:467–73.
Xu L-P, Jin S, Wang S-Q, Xia L-H, Bai H, Gao S-J, et al. Upfront haploidentical transplant for acquired severe aplastic anemia: registry-based comparison with matched related transplant. J Hematol Oncol. 2017;10:25.
Xu LP, Xu ZL, Wang FR, Mo XD, Han TT, Han W, et al. Unmanipulated haploidentical transplantation conditioning with busulfan, cyclophosphamide and anti-thymoglobulin for adult severe aplastic anaemia. Bone Marrow Transplant. 2018;53:188–92.
Gupta V, Eapen M, Brazauskas R, Carreras J, Aljurf M, Gale RP, et al. Impact of age on outcomes after bone marrow transplantation for acquired aplastic anemia using HLA-matched sibling donors. Haematologica. 2010;95:2119–25.
Bacigalupo A. How I treat acquired aplastic anemia. Blood. 2017;129:1428–36.
Shin SH, Jeon YW, Yoon JH, Yahng SA, Lee SE, Cho BS, et al. Comparable outcomes between younger (40 years) and older (>40 years) adult patients with severe aplastic anemia after HLA-matched sibling stem cell transplantation using fludarabine-based conditioning. Bone Marrow Transplant. 2016;51:1456–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Leick, M., Hunter, B., DeFilipp, Z. et al. Posttransplant cyclophosphamide in allogeneic bone marrow transplantation for the treatment of nonmalignant hematological diseases. Bone Marrow Transplant 55, 758–762 (2020). https://doi.org/10.1038/s41409-019-0725-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-019-0725-8
This article is cited by
-
Systematic overview of HLA-matched allogeneic hematopoietic cell transplantation with post-transplantation cyclophosphamide
International Journal of Hematology (2022)