Abstract
Health care costs attributed to biologics have increased exponentially in the recent years, thus biosimilars offer a possible solution to limit costs while maintaining safety and efficacy. Reducing expenditure is vital to health care especially in developing countries where affordability and access to health care is a major challenge. We discuss the opportunities and the challenges of biosimilars in the field of hematopoietic cell transplantation (HCT) in low- and lower-middle income countries. Developing countries can potentially invest in the forecasted costs reduction by utilizing biosimilars. This can be used to decrease the costs of procedures such as HCT, which is a rapidly growing field in many developing regions. The introduction of biosimilars in the developing regions faces many challenges which include, but are not limited to: legal and regulatory issues, lack of research infrastructure, and the presence of educational barriers. Thus, collaborative efforts are needed to ensure an effective and safe introduction of biosimilars into low- and lower-middle income countries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Change history
15 October 2019
A Correction to this paper has been published: https://doi.org/10.1038/s41409-019-0714-y
References
Patel D, Gillis C, Naggar J, Mistry A, Mantzoros C. The rise of biosimilars: how they got here and where they are going. Metabolism. 2017;75:45–53.
Weise M, Bielsky M, De Smet K, Ehmann F, Ekman N, Giezen T, et al. Biosimilars: what clinicians should know. Blood. 2012;120:5111–7.
Loo J. Industry surveys: biotechnology. Standard & Poor’s. New York; 2014.
Gascon P. The evolving role of biosimilars in haematology–oncology: a practical perspective. Ther Adv Hematol. 2015;6:267–81.
Hirsch B, Lyman G. Biosimilars: a cure to the U.S. health care cost conundrum? Blood Rev. 2014;28:263–8.
Chopra R, Lopes G. Improving access to cancer treatments: the role of biosimilars. J Glob Oncol. 2017;3:596–610.
Blackstone E, Fuhr J. The economics of biosimilars. Am Health Drug Benefits 2013;6:469–78.
Zelenetz AD, Ahmed I, Braud EL, et al. NCCN biosimilars white paper: regulatory, scientific, and patient safety perspectives. J Natl Compr Cancer Netw. 2011;9:S1–S22.
Khera N, Zeliadt S, Lee S. Economics of hematopoietic cell transplantation. Blood. 2012;120:1545–51.
Khera N, Emmert A, Storer B, Sandmaier B, Alyea E, Lee S. Costs of allogeneic hematopoietic cell transplantation using reduced intensity conditioning regimens. Oncologist. 2014;19:639–44.
Hashmi S, Srivastava A, Rasheed W, Adil S, Wu T, Jagasia M, et al. Cost and quality issues in establishing hematopoietic cell transplant program in developing countries. Hematol Oncol Stem Cell Ther 2017;10:167–72.
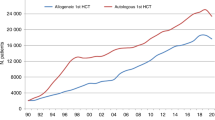
Gratwohl A, Pasquini M, Aljurf M, Atsuta Y, Baldomero H, Foeken L, et al. One million haemopoietic stem-cell transplants: a retrospective observational study. Lancet Haematol. 2015;2:e91–e100.
Baldomero H, Aljurf M, Zaidi S, Hashmi S, Ghavamzadeh A, Elhaddad A, et al. Narrowing the gap for hematopoietic stem cell transplantation in the East-Mediterranean/African region: comparison with global HSCT indications and trends. Bone Marrow Transplant. 2019;54:402–17.
Aljurf M, Nassar A, Hamidieh A, Elhaddad A, Hamladji R, Bazarbachi A, et al. Hematopoietic stem cell transplantation in the Eastern Mediterranean Region (EMRO) 2011–2012: a comprehensive report on behalf of the Eastern Mediterranean Blood and Marrow Transplantation group (EMBMT). Hematol Oncol Stem Cell Ther. 2015;8:167–75.
Gratwohl A, Baldomero H, Aljurf M, Pasquini M, Bouzas L, Yoshimi A, et al. Hematopoietic stem cell transplantation a global perspective. JAMA. 2010;303:1617–24.
Gale R, Seber A, Bonfim C, Pasquini M. Haematopoietic cell transplants in Latin America. Bone Marrow Transplant. 2016;51:898–905.
Bazarbachi A, Labopin M, Ghavamzadeh A, Giebel S, Al-Zahrani H, Ladeb S, et al. Allogeneic matched-sibling hematopoietic cell transplantation for AML: comparable outcomes between Eastern Mediterranean (EMBMT) and European (EBMT) centers. Bone Marrow Transplant. 2013;48:1065–9.
Abdel-Rahman F, Hussein A, Rihani R, Hlalah O, El Taani H, Sharma S, et al. Bone marrow and stem cell transplantation at King Hussein cancer center. Bone Marrow Transplant. 2008;402:S89–S91.
Jaime-Perez J, Heredia-Salazar A, Cantu-Rodriguez O, Gutierrez-Aguirre H, Villarreal-Villarreal C, Mancias-Guerra C, et al. Cost structure and clinical outcome of a stem cell transplantation program in a developing country: the experience in Northeast Mexico. Oncologist. 2015;20:386–92.
Sharma SK, Choudhary D, Gupta N, Dhamija M, Khandelwal V, Kharya G, et al. Cost of hematopoietic stem cell transplantation in India. Mediterr J Hematol Infect Dis. 2014;6:e2014046.
Lyman G, Zon R, Harvey R, Schilsky R. Rationale, opportunities, and reality of biosimilar medications. New Engl J Med. 2018;378:2036–44.
Biosimilar Product Information. Fda.gov. https://www.fda.gov/drugs/developmentapprovalprocess/howdrugsaredevelopedandapproved/approvalapplications/therapeuticbiologicapplications/biosimilars/ucm580432.htm (2018).
Centrally authorised biosimilar medicines| European Medicines Agency. Ema.europa.eu. https://www.ema.europa.eu/medicines/field_ema_web_categories%253Aname_field/Human/ema_group_types/ema_medicine/field_ema_med_status/authorised-36/ema_medicine_types/field_ema_med_biosimilar/search_api_aggregation_ema_medicine_types/field_ema_med_biosimilar (2018).
Lisenko K, Baertsch MA, Meiser R, Pavel P, Bruckner T, Kriegsmann M, et al. Comparison of biosimilar filgrastim, originator filgrastim, and lenograstim for autologous stem cell mobilization in patients with multiple myeloma. Transfusion. 2017;57:2359–65. Oct
Sivgin S, Karakus E, Keklik M, Zararsiz G, Solmaz M, Kaynar L, et al. Evaluation of the efficacy and safety of original filgrastim (Neupogen®), biosimilar filgrastim (Leucostim®) and Lenograstim (Granocyte®) in CD34+ peripheral hematopoietic stem cell mobilization procedures for allogeneic hematopoietic stem cell transplant donors. Transfus Apher Sci. 2016;54:410–5.
Sivgin S, Karakus E, Kaynar L, Kurnaz F, Pala C, Keklik M, et al. The comparison of Filgrastim (Neupogen®), biosimilar filgrastim (Leucostim®) and Lenograstim (Granocyte®) as a first line peripheral blood stem cell mobilization strategy in autologous hematopoieitic stem cell transplantation: a single center experience from Turkey. Transfus Apher Sci. 2013;48:315–20.
Corbin M, Peyton-Thomas B, Selby C, Bozeman A, Leary C, Devarakonda S, et al. Efficacy of a tbo-filgrastim protocol for stem cell engraftment in autologous stem cell transplant. Biol Blood Marrow Transplant. 2017;23:S417–S418.
Harada K, Yamada Y, Konishi T, Nagata A, Takezaki T, Kaito S, et al. Comparison of transplant outcomes and economic costs between biosimilar and originator filgrastim in allogeneic hematopoietic stem cell transplantation. Int J Hematol. 2016;104:709–19.
Ianotto J, Ngo Sack F, Couturier M, Tempescul A, Mugnier N, Delepine P, et al. Biosimilars of filgrastim in autologous stem cell transplant: reduction in granulocyte-colony stimulating factor costs, but similar effects on bone marrow recovery. Leuk Lymphoma. 2013;55:74–77.
León-González M, León-Peña AA, Vallejo-VIllalobos MF, Núñez-Cortés AK, Ruiz-Argüelles A, Ruiz-Argüelles GJ. Mexican biosimilar filgrastim for autologous hematopoietic stem cell mobilization and transplantation. Rev Investig Clin. 2016;68:181–3.
Halim L, Márquez M, Maas-Bakker R, Castañeda-Hernández G, Jiskoot W, Schellekens H. Quality comparison of biosimilar and copy filgrastim products with the innovator product. Pharm Res. 2018;35:1–12.
Najjar R, Sharma S, Farraj R, Muffarrej D, Haroun A, Hashem H, et al. Comparable efficacy of peripheral stem cell mobilization using biosimilar Filgrastim Nivestim® to original Neupogen® in healthy donors. Bone Marrow Transplantation: 2019 53:766.
U.S. Food and Drug Administration. Rituximab; Highlights of prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/103705s5367s5388lbl.pdf. Accessed 18 Nov 2018.
Kharfan-Dabaja MA, Cutler CS. Rituximab for prevention and treatment of graft-versus-host disease. Int J Hematol. 2011;93:578–85. May
Cutler C, Kim HT, Bindra B, Sarantopoulos S, Ho VT, Chen YB, et al. Rituximab prophylaxis prevents corticosteroid-requiring chronic GVHD after allogeneic peripheral blood stem cell transplantation: results of a phase 2 trial. Blood. 2013;122:1510–7. Aug
Cutler C, Miklos D, Kim HT, Treister N, Woo SB, Bienfang D, et al. Rituximab for steroid-refractory chronic graft-versus-host disease. Blood. 2006;108:756–62. Jul
Arai S, Sahaf B, Narasimhan B, Chen GL, Jones CD, Lowsky R, et al. Prophylactic rituximab after allogeneic transplantation decreases B-cell alloimmunity with low chronic GVHD incidence. Blood. 2012;119:6145–54. Jun
Hodge G, Hodge S, Chambers D, Reynolds PN, Holmes M. Bronchiolitis obliterans syndrome is associated with absence of suppression of peripheral blood Th1 proinflammatory cytokines. Transplantation. 2009;88:211–8. Jul
Yalniz FF, Hefazi M, McCullough K, Litzow MR, Hogan WJ, Wolf R, et al. Safety and efficacy of infliximab therapy in the setting of steroid-refractory acute graft-versus-host disease. Biol Blood Marrow Transplant. 2017;23:1478–84. Sep
De Jong CN, Saes L, Klerk CPW, Van der Klift M, Cornelissen JJ, Broers AEC. Etanercept for steroid-refractory acute graft-versus-host disease: a single center experience. PLoS ONE. 2017;12:e0187184. Oct
Park JH, Lee HJ, Kim SR, Song GW, Lee SK, Park SY, et al. Etanercept for steroid-refractory acute graft versus host disease following allogeneic hematopoietic stem cell transplantation. Korean J Intern Med. 2014;29:630–6.
Yanik G, Hellerstedt B, Custer J, et al. Etanercept (Enbrel) administration for idiopathic pneumonia syndrome after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2002;8:395–400.
Fullmer JJ, Fan LL, Dishop MK, Rodgers C, Krance R. Successful treatment of bronchiolitis obliterans in a bone marrow transplant patient with tumor necrosis factor-alpha blockade. Pediatrics. 2005;116:767–70.
Eleryan MG, Akhiyat S, Rengifo-pardo M, Ehrlich A. Biosimilars: potential implications for clinicians. Clin Cosmet Investig Dermatol. 2016; 9:135–42.
Mulcahy AW, Hlavka JP, Case SR. Biosimilar cost savings in the United States: initial experience and future potential. Santa Monica, CA: RAND; 2017.
Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman MH. Poverty and access to health care in developing countries. Ann N Y Acad Sci 2008;1136:161–71.
O’Donnell O. Access to health care in developing countries: breaking down demand side barriers. Cad Saude Publica. 2007;23:2820–34.
Qureshi ZP, Magwood JS, Singh S, et al. Rituximab and biosimilars: equivalence and reciprocity. Biosimilars. 2013;2013:19–25.
What’s next for biosimilars in emerging markets? McKinsey & Company; 2019. https://www.mckinsey.com/industries/pharmaceuticals-and-medical-products/our-insights/whats-next-for-biosimilars-in-emerging-markets.
Rägo L, Sillo H, ‘t Hoen E, Zweygarth M. Regulatory framework for access to safe, effective quality medicines. Antivir Ther. 2014;19:69–77.
Pezzola A, Sweet CM. Global pharmaceutical regulation: the challenge of integration for developing states. Glob Health 2016;85:1–18.
Krishnan A, Mody R, Malhotra H. Global regulatory landscape of biosimilars: emerging and established market perspectives. Biosimilars. 2015; 5:19–32.
Guidance for industry: scientific considerations in demonstrating biosimilarity to a reference product (draft guidance). US Food and Drug Administration; 2015http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM291128.pdf.
Biosimilars in the EU: information guide for healthcare professionals. European Medicines Agency and the European Commission; 2017https://www.ema.europa.eu/documents/leaflet/biosimilars-eu-information-guide-healthcare-professionals_en.pdf.
Chauhan M, Malik S. Regulatory guidelines for approval of biosimilars In India, Europe, Brazil And China: a comprehensive overview. Int J Pharm Pharm Sci. 2016;8:7.
Biosimilars in Brazil. Pinheironeto.com.br. 2019http://www.pinheironeto.com.br/Documents/Artigos/Biosimilars_Brazil_JAN2017.pdf.
Guidance for registration of biosimilars. Jordan Food & Drug Administration; 2014 http://old.jfda.jo/Download/News/239_530.pdf.
Guideline for registration of biosimilar products. Central Administration for Pharmaceutical Affairs: Ministry of health. http://www.eda.mohp.gov.eg/Files/304_guidelines%20after%20correction.pdf.
Guideline on biosimilar product: quality considerations. Saudi Arabia Food & Drug Administration; 2017 https://www.sfda.gov.sa/ar/drug/resources/DocLib2/Guideline-on-biosimilar-products.pdf.
Guidelines on similar biologic: regulatory requirements for marketing authorization in India. http://cdsco.nic.in/writereaddata/Proposed%20Guidelines%20for%20Similar%20Biologic%202016.pdf.
Guidelines for ensuring the quality, safety and efficacy of biosimilar products. Japanese Pharmaceuticals and Medical Devices Agency. https://www.pmda.go.jp/files/000206248.pdf.
Alhawassi T, Abuelizz H, Almetwazi M, Mahmoud M, Alghamdi A, Alruthia Y, et al. Advancing pharmaceuticals and patient safety in Saudi Arabia: a 2030 vision initiative. Saudi Pharm J. 2018;26:71–74.
Cheraghali A. Biosimilars; a unique opportunity for Iran national health sector and national pharmaceutical industry. DARU J Pharma Sci. 2012;20:1–4.
Declerck P, Danesi R, Petersel D, Jacobs I. The language of biosimilars: clarification, definitions, and regulatory aspects. Drugs. 2017;77:671–7.
Surendiran A, Pradhan SC, Adithan C. Role of pharmacogenomics in drug discovery and development. Indian J Pharmacol. 2008;40:137–43.
Ortega VE, Meyers DA. Pharmacogenetics: implications of race and ethnicity on defining genetic profiles for personalized medicine. J Allergy Clin Immunol. 2014;133:16–26.
Amerson RM, Strang CW. Addressing the challenges of conducting research in developing countries. J Nurs Scholarsh. 2015;47:584–91. Nov
Jacobs I, Singh E, Sewell KL, et al. Patient attitudes and understanding about biosimilars: an international cross sectional survey. Patient Prefer Adherence. 2016;10:937–48.
Tomaszewski D. Biosimilar naming conventions: pharmacist perceptions and impact on confidence in dispensing biologics. J Manag Care Spec Pharm. 2016;22:919–26.
Cohen H, Beydoun D, Chien D, et al. Awareness, knowledge, and perceptions of biosimilars among specialty physicians. Adv Ther. 2017;33:2160–72.
Cook J, McGrath M, Dixon M, Switchenko J, Harvey R, Pentz R. Academic oncology clinicians’ understanding of biosimilars and information needed before prescribing. Ther Adv Med Oncol. 2019;11:1–12.
Farhat F, Othman A, el Karak F, Kattan J. Review and results of a survey about biosimilars prescription and challenges in the Middle East and North Africa region. SpringerPlus. 2016;5:2113.
Acknowledgements
Leadership of the CIBMTR’s Health Services and International Studies working committee.
Author information
Authors and Affiliations
Contributions
IM, MA, and SKH wrote the first draft of the paper. All authors vouch for the accuracy and contents of the paper. All authors approved the final version of the draft.
Corresponding author
Ethics declarations
Conflict of interest
SKH: Honorarium: Mallinckrodt, Novartis, Janssen. Advisory board: Novartis, Janssen.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muhsen, I.N., Hashmi, S.K., Niederwieser, D. et al. Worldwide Network for Blood and Marrow Transplantation (WBMT) perspective: the role of biosimilars in hematopoietic cell transplant: current opportunities and challenges in low- and lower-middle income countries. Bone Marrow Transplant 55, 698–707 (2020). https://doi.org/10.1038/s41409-019-0658-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-019-0658-2
This article is cited by
-
Hematopoietic stem cell transplantation activity in China 2019: a report from the Chinese Blood and Marrow Transplantation Registry Group
Bone Marrow Transplantation (2021)