Abstract
Study design
Descriptive study.
Objectives
To describe functional outcomes using Spinal Cord Independence Measure III (SCIM III) following inpatient rehabilitation among individuals with complete spinal cord injury (SCI) in the low-income setting of Nepal; to evaluate functional changes from rehabilitation admission to discharge and to compare functional outcomes between neurological levels of injury (NLI) at discharge.
Setting
Spinal Injury Rehabilitation Centre (SIRC), Kavrepalanchowk, Nepal.
Methods
We present data of all individuals with complete SCI who completed rehabilitation at SIRC in 2017. Data collected included: demographics, aetiology, neurological assessment, admission/discharge SCIM III scores, and length of stay. Data were analyzed using descriptive statistics. Pre/post-SCIM III scores were analyzed using Related-Samples Wilcoxon signed-rank test. Comparative analysis between NLIs was done using the Kruskal Wallis ANOVA test followed by pairwise Mann–Whitney U tests.
Results
Ninety-six individuals were included. Mean (SD) age was 33.5 (14.2) years, with a male/female ratio of 3.4:1. Median admission and discharge total SCIM III scores for cervical, thoracic and lumbosacral levels were 10 and 21, 16 and 61, and 41 and 79.5, respectively. Median total SCIM III score change between admission and discharge were 11 (p = 0.003), 43 (p < 0.001) and 40 (p = 0.068) for cervical, thoracic and lumbar groups, respectively.
Conclusions
This study is the first of its kind to describe functional outcomes among individuals with complete SCI in the low-income setting of Nepal. All SCI groups showed a positive trend in SCIM III from admission to discharge, with improvements reaching statistical significance among groups with cervical and thoracic NLIs.
Similar content being viewed by others
Introduction
Every year, an estimated 250,000–500,000 people sustain new SCIs around the world [1]. Based on limited data from Nepal, 300–5000 per million individuals sustain new traumatic SCI annually [2]. Falls are the most common cause of SCI in Nepal and South Asia, followed by road traffic injury [3, 4]. In addition, natural disasters known to cause SCI including earthquakes and landslides are common in Nepal [5]. Males more commonly sustain injuries and most of them are of working age with range 32–47 years [3].
Spinal cord injury carries high rates of morbidity and mortality [1]. Initiating specialized SCI care that includes comprehensive, interdisciplinary rehabilitation has been shown to reduce overall morbidity and promote functional independence [1, 6, 7]. Given the dynamic nature of recovery, it is important to assess the functional status of patients throughout the course of inpatient rehabilitation. Assessments of functional outcomes specifically help the interdisciplinary team plan the rehabilitation process, communicate with patients and families about prognosis, and predict long-term functional outcomes [8]. Moreover, the evaluation of the functional status with the neurological level is required to assess the rehabilitation efficiency [9]. The Spinal Cord Independence Measure III (SCIM III) is a disability scale used worldwide to assess changes in an individual’s functional status during SCI rehabilitation [10,11,12]. Individuals with complete SCI are not expected to have significance neurologic recovery, but are expected to have functional improvement with rehabilitation [13]. Therefore, they represent a fairly uniform population with more predictable and uniform outcomes. Target SCIM III scores have been reported for each neurological level of complete injury. However, these targets were established in high-income countries only [14]. Given differences in socioeconomics, medical/rehabilitation treatment options, and assistive technologies between high- and low-income countries, these targets may not be representative for our low-income context.
No study to our knowledge has evaluated SCIM III outcome scores among individuals with complete SCI in low- and/or middle-income countries. Therefore, the objectives of this study were (a) to describe functional outcomes using SCIM III following inpatient rehabilitation among individuals with complete SCI in the low-income setting of Nepal (b) to evaluate functional changes from rehabilitation admission to discharge (c) to compare functional outcomes between neurological levels of injury (NLI) at discharge.
Methods
This is a descriptive study. Data were collected for all individuals with complete SCI admitted to Spinal Injury Rehabilitation Centre (SIRC) in 2017. SIRC is the largest SCI rehabilitation centre in Nepal. The 51-bed centre serves approximately 300 individuals with new SCI every year from every district in the country. Interdisciplinary SCI rehabilitation is lead by a physical medicine and rehabilitation physician and includes physical therapy, occupational therapy, rehabilitation nursing care, psychology, social work, recreational therapy, and peer counselling. Criteria for eligibility were all individuals >3 years of age admitted to SIRC with traumatic and non-traumatic SCI resulting in complete (American Spinal Injury Association Impairment Scale A) injury who completed the entire recommended rehabilitation stay. Completeness was defined as those with complete injuries at the time of discharge from rehabilitation. Exclusion criteria were (a) individuals unable to be accurately assessed using the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) (i.e., concomitant stroke or brain injury resulting in cognitive impairment, paediatric patients unable to accurately participate) and (b) individuals with concomitant orthopaedic or other neurological injury persisting throughout the rehabilitation stay that would alter expected recovery/outcomes following SCI (i.e., traumatic amputation, traumatic brain injury resulting in hemiplegia, brachial plexus injury).
A total of 294 individuals with SCI who admitted to SIRC in 2017 were screened for enrolment. Information collected included age, sex, aetiology, ISNCSCI at admission and discharge, SCIM III scores at admission and discharge, and length of stay (days). Standard care for individuals with SCI at SIRC includes ISNCSCI assessment on admission and discharge by physicians with significant training and experience in this assessment. The ISNCSCI is a well-established tool used by clinicians and researchers to accurately assess and quantify an individual with SCI’s neurological impairment [15, 16].
Spinal Cord Independence Measure III (SCIM III) is a clinician-rated instrument that was developed specifically to measure the level of independence in overall daily life activities for individuals with SCI [10, 17]. It comprised of 19 items across 3 subscales: self-care (feeding, grooming, bathing, dressing), respiratory and sphincter management, and mobility. Mobility is subdivided into ‘room and toilet’ and ‘indoors and outdoors’. Each item is marked based on its assumed clinical relevance to daily life activities of the individual with SCI. The score ranges between 0 and 100 [11, 12, 18,19,20]. An improvement of at least four points results in a small, clinically significant improvement, while an improvement of at least ten points results in a substantial clinical improvement [21]. The SCIM III has been shown to be a valid, reliable, and responsive instrument for use among individuals with SCI [19, 20].
The SCIM III assessment has been part of standard care at SIRC for over 10 years. It is routinely performed on every patient with SCI on admission, discharge, and at regular intervals throughout their stay. Providers including physiotherapists, occupational therapists, and nurses with training and experience administer and record the SCIM III. Admission scores are reported within 1 week of admission and discharge scores are reported within 3 days before discharge. The SCIM III self-care components were scored by occupational therapists, respiration and sphincter management by nurses, and physical therapists scored all mobility components. Total SCIM III score and subscores (self-care, respiration and sphincter management (RSM), mobility room and toilet and mobility indoors and outdoors at admission and at discharge) were de-identified and entered into a database for analysis.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. SIRC’s ethical review committee and the Nepal Health Research Council approved the study and provided oversight. The need for informed consent was waived as the data analyzed for this study were collected as part of SIRC’s standard of care. All data were de-identified prior to analysis.
Statistical analysis
Data were analyzed using SPSS version 24.0 (IBM, New York, USA). All continuous data did not assume normal distribution and were described as median and interquatile range (IQR). The number and percentage (n, %) were described for categorical data. Nonparametric statistics Wilcoxon signed-rank test were used for comparing SCIM III scores at admission and discharge. The Kruskal Wallis ANOVA test was used for comparing total SCIM III and subscale of SCIM III scores among NLIs. Pairwise comparison was done using the Mann–Whitney U tests. The relationship of NLI with discharge total SCIM III score and with SCIM III score change were analyzed using Spearman’s rank correlation coefficient. A two-sided p value <0.05 was defined as statistically significant.
Results
Among the 294 individuals admitted for rehabilitation during the study period, 166 were not eligible due to incomplete/non-SCI, interfering conditions, or insufficient data. Of the remaining 128 individuals, 96 individuals completed rehabilitation and were included in data analysis (Fig. 1). The mean (SD) age was 33.5 (14.2) years, ranging from 4 to 83 years old with a male-to-female ratio of 3.4:1 (Table 1). The majority of individuals were young, belonging to the age group 16–45 years. The most common level of injury was thoracic (84.4%), specifically T11. The most common mechanism of injury was fall, followed by road traffic injury. Median (IQR) time between SCI and admission to the rehabilitation facility was 27 (17–52) days. The mean (SD) length of stay at the rehabilitation centre was 84.4 (40.6) days.
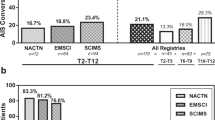
Median total and subscale SCIM III scores changed significantly from admission to discharge (p < 0.001) and are presented in Table 2. Median admission, discharge, and change in total SCIM III by NLI are presented in Tables 3 and 4. Statistically significant improvement in SCIM III score at discharge was noted among individuals with both cervical and thoracic NLIs. The small proportion of individuals with lumbosacral NLIs demonstrated a positive trend in SCIM III prior to discharge (Table 3). Median SCIM III subscale scores at the time of discharge for every NLI are presented in Table 5. The total SCIM III discharge scores and change in scores were inversely correlated with NLI (r = 0.466, p < 0.001 and r = 0.371, p = 0.001).
Discussion
This study is the first of its kind to describe functional outcomes among individuals with complete SCI in the low-income setting of Nepal. All groups showed a positive trend in SCIM III from admission to discharge, with improvements reaching statistical significance among groups with cervical (p = 0.003) and thoracic (p < 0.001) NLIs. For rehabilitation professionals participating in the care of individuals with SCI, having expected SCIM III discharge scores based on NLI may serve to inform the goals and duration of individuals’ rehabilitation plan.
Aidinoff et al. performed a study to establish target SCIM III values for each neurological level of complete SCI [14]. They did this by calculating total and subscale SCIM III scores and gain at discharge for 128 individuals with complete SCI from six different countries. As all participants in this study were from high-income countries, we were specifically interested in how our findings from a resource-limited, low-income country would compare. Our observed SCIM III discharge scores compared to Aidinoff et al.’s [14] results appear relatively similar. Exceptions include consistently lower mobility scores for individuals with tetraplegia in Nepal. This may be explained by our rugged terrain; inaccessible physical infrastructure, which limits individuals’ outdoor mobility; as well as non-availability of powered wheelchairs in Nepal. In addition, individuals with thoracic-level injuries in Nepal showed comparatively lower respiration/sphincter management scores. This may be related to the reality that our management options for neurogenic bladder are substantially limited. We currently do not have access to intervesicular agents including botulinum toxins, vanillanoid compounds, propantheline or intravesicular oxybutinyn. Surgical bladder augmentation, catheterizable abdominal stomas, and cutaneous ileal conduit diversions are not available. Electrical stimulation, sphincterotomy, artificial sphincters, and stents are also not available. Most oral medications (anticholinergics and alpha-adrenergic blockers), indwelling catheters, and clean intermittent catheters are readily available.
Ackerman et al. performed a study to analyze functional gains among individuals with motor complete (AIS A and B) SCI during a post-acute rehabilitation programme in the high-income setting of the United States [22]. They found median SCIM III at rehabilitation admission of 42, at discharge 50, with a statistically significant median improvement of 5 points. This admission SCIM III score of 42 is notably higher than our finding of 16 (14.25–17). This difference may be due to the active presence of rehabilitation services within the acute tertiary care hospitals in the States, while many of our patients had received very little rehabilitation prior to admission to SIRC. Furthermore, the median time from injury to rehabilitation in Ackerman’s study was 98.5 days vs. 27 (17–52) days in our study, another factor that likely contributes to this difference.
This study includes data from just one centre in Nepal, therefore generalizability of these SCIM III scores to other populations may be limited. In addition, while a sample size of 96 is relatively large for studies including individuals with complete SCI, the small number in subgroups limits our ability to compare data across settings. As described above, only 96 of 128 potentially eligible individuals were included in data analysis. Incomplete documentation and individuals not completing rehabilitation led to this exclusion of a large portion (25%) of eligible individuals. At our centre, individuals may not complete rehabilitation for a variety of reasons include leaving early against medical advice and/or being transferred to acute care hospitals due to complications. The absence of these individuals in analysis may skew the results. Finally, we did not assess inter-rater reliability of the SCIM III in this study, which may limit our findings.
A recommended next step would be a multi-centre study including other low- and middle-income countries to further establish target SCIM III scores by NLI across settings. Specific to our context, the following are warranted: identifying and removing barriers to completing SCI rehabilitation; exploring interventions to improve sphincter and mobility outcomes among individuals with SCI in Nepal.
Conclusion
This study is the first of its kind to describe functional outcomes among individuals with complete SCI in the low-income setting of Nepal. All SCI groups showed a positive trend in SCIM III from admission to discharge, with improvements reaching statistical significance among groups with cervical and thoracic NLIs.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Bickenbach J, Officer A, Shakespeare T, Von Groote P, World Health Organization. International perspectives on spinal cord injury, WHO Library, 2013. http://www.who.int/disabilities/policies/spinal_cord_injury/en/. Accessed 3 Oct 2018.
Scovil CY, Ranabhat MK, Craighead IB, Wee J. Follow-up study of spinal cord injured patients after discharge from inpatient rehabilitation in Nepal in 2007. Spinal Cord. 2012;50:232–7. https://doi.org/10.1038/sc.2011.119
Parajuli B, Acharya K, Shrestha D. Epidemiology of traumatic spinal cord injury in Nepal: a systematic review. Asian. J Med Sci. 2020;11:121–8. https://doi.org/10.3126/ajms.v11i6.30151.
Willott A, Dhakal R, Groves C, Mytton J, Ellis M The demographics and traumatic causes of spinal cord injury in Nepal: an observational study. Trauma. 2020:1460408620941342. https://doi.org/10.1177/1460408620941342.
Mytton J, Bhatta S, Thorne M, Pant PJCM Understanding the burden of injuries in Nepal: a systematic review of published studies. 2019;6:1673654. https://doi.org/10.1080/2331205X.2019.1673654.
Wolfe DL, Hsieh JT, Mehta S Rehabilitation practices and associated outcomes following spinal cord injury. Spinal cord injury rehabilitation evidence. 2010:44–90. https://scireproject.com/evidence/rehabilitation-evidence/rehabilitation-practices/whatsci-rehabilitaion. Assessed 2 Oct 2018.
Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Early acute management in adults with spinal cord injury: a clinical practice guideline for health-care professionals. Paralyzed Veterans of America; 2008. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2582434/. Accessed 15 Sep 2016.
Post MW, Dallmeijer AJ, Angenot EL, van Asbeck FW, van der Woude LH. Duration and functional outcome of spinal cord injury rehabilitation in the Netherlands. J Rehabil Res Dev. 2005;42:75–85. https://doi.org/10.1682/jrrd.2004.10.0133
Wirth B, van Hedel HJ, Kometer B, Dietz V, Curt A Changes in activity after a complete spinal cord injury as measured by the Spinal Cord Independence Measure II (SCIM II). Neurorehabil Neural Repair. 2008;22:145–53. https://doi.org/10.1038/s41394-021-00452-zhttps://doi.org/10.1177/1545968307306240.
Catz A, Itzkovich M. Spinal Cord independence measure: comprehensive ability rating scale for the spinal cord lesion patient. J Rehabil Res Dev. 2007;44:65–8. https://doi.org/10.1682/jrrd.2005.07.0123
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. The spinal cord independence measure (SCIM): sensitivity to functional changes in subgroups of spinal cord lesion patients. Spinal Cord. 2001;39:97–100. https://doi.org/10.1038/sj.sc.3101118
Nitsch KP, Stipp KL. Measurement characteristics and clinical utility of the spinal cord independence measure-III among individuals with spinal cord injury. Arch Phys Med Rehabil. 2016;97:1601–3. https://www.archives-pmr.org/article/S0003-9993(16)00107-6/pdf.
Mazwi NL, Adeletti K, Hirschberg RE. Traumatic spinal cord injury: recovery, rehabilitation, and prognosis. Curr Trauma Rep. 2015;1:182–92. https://doi.org/10.1007/s40719-015-0023-x.
Aidinoff E, Front L, Itzkovich M, Bluvshtein V, Gelernter I, Hart J, et al. Expected spinal cord independence measure, third version, scores for various neurological levels after complete spinal cord lesions. Spinal Cord. 2011;49:893–6. https://doi.org/10.1038/sc.2011.32
Schuld C, Franz S, Brüggemann K, Heutehaus L, Weidner N, Kirshblum SC, et al. International standards for neurological classification of spinal cord injury: impact of the revised worksheet (revision 02/13) on classification performance. J Spinal Cord Med. 2016;39:504–12. https://doi.org/10.1080/10790268.2016.1180831
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4066420/.
Almeida CD, Coelho JN, Riberto M. Applicability, validation and reproducibility of the Spinal Cord Independence Measure version III (SCIM III) in patients with non-traumatic spinal cord lesions. Disabil Rehabil. 2016;38:2229–34. https://doi.org/10.3109/09638288.2015.1129454
Mahmoud H, Qannam H, Zbogar D, Mortenson B. Spinal cord injury rehabilitation in Riyadh, Saudi Arabia: time to rehabilitation admission, length of stay and functional independence. Spinal Cord. 2017;55:509–14. https://doi.org/10.1038/sc.2016.165
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29:1926–33. https://doi.org/10.1080/09638280601046302
Spinal Cord Injury Research Evidence (SCIRE Project). Spinal Cord Independence Measure III. Accessed 3 October 2018: https://scireproject.com/outcome-measures/outcome-measure-tool/spinal-cord-independence-measure-scim/#1467983894080-2c29ca8d-88af. Accessed 3 Oct 2018.
Scivoletto G, Tamburella F, Laurenza L, Molinari M. The spinal cord independence measure: how much change is clinically significant for spinal cord injury subjects. Disabil Rehabil. 2013;35:1808–13. https://doi.org/10.3109/09638288.2012.756942https://pubmed.ncbi.nlm.nih.gov/23343359/.
Ackerman P, Morrison S, McDowell S, Vazquez L. Using the Spinal Cord Independence Measure III to measure functional recovery in a post-acute spinal cord injury program. Spinal Cord. 2010;48:380–7. https://doi.org/10.1038/sc.2009.140
Acknowledgements
The authors would like to thank Spinal Injury Rehabilitation Centre, Nepal.
Author information
Authors and Affiliations
Contributions
PK was responsible for designing the study, data collection, analysis, interpretation, and writing the manuscript. CJ contributed to data analysis, interpretation, and writing the manuscript. RD contributed to data interpretation and writing the manuscript. CCG contributed to study design, data analysis, interpretation, and writing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khatri, P., Jalayondeja, C., Dhakal, R. et al. Functional outcome following inpatient rehabilitation among individuals with complete spinal cord injury in Nepal. Spinal Cord Ser Cases 7, 93 (2021). https://doi.org/10.1038/s41394-021-00452-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00452-z