Abstract
Introduction
Calcification of the ligamentum flavum can cause acute neck pain and compression of the spinal cord, which can induce myelopathy. However, there are very few reports of acute exacerbation of myelopathy due to a pseudogout attack of the cervical ligamentum flavum, and there are no reports of that after a cervical spinal cord injury. Here, we report the case of a patient with acute neck pain and tetraplegia caused by pseudogout attack of the cervical ligamentum flavum after cervical central spinal cord injury.
Case presentation
A 78-year-old man experienced mild tetraplegia after falling. He was diagnosed with cervical spinal cord injury without radiographic abnormality. Four days after the injury, he developed fever and his paralysis worsened. Magnetic resonance imaging revealed increasing of spinal stenosis at the C4–5 level. Computed tomography revealed calcification of the ligamentum flavum at the same level. C3 laminectomy and C4-5 laminoplasty were performed. A collection of turbid yellow fluid was found in the ligamentum flavum. A histopathological examination revealed evidence of calcium pyrophosphate dihydrate crystals in the fluid.
Discussion
With increase in the aging population in Japan, the patients with acute exacerbation of myelopathy due to pseudogout in the cervical spine following spinal cord injury without radiographic abnormality may increase in the future. Computed tomography is useful for the diagnosis of such cases.
Similar content being viewed by others
Introduction
Calcium pyrophosphate dihydrate (CPPD) crystal deposition disease (also known as pseudogout) is well known to induce acute arthritis in joints such as the knee and the wrist [1]. Aging is one of the risk factors for pseudogout, and the elderly population is rapidly increasing in Japan [2]. Calcification of the ligamentum flavum sometimes causes acute neck pain and compression of the spinal cord [3], which can induce myelopathy [4]. However, there are few reports of acute exacerbation of myelopathy due to a pseudogout attack of the cervical ligamentum flavum, and there are no reports of that after a cervical spinal cord injury.
Although trauma is known to be one of the risk factors for pseudogout [5], there are no reports of myelopathy due to a pseudogout attack following spinal cord injury. We report a case of a patient with acute neck pain and tetraplegia due to a pseudogout attack of the cervical ligamentum flavum following cervical spinal cord injury.
Case presentation
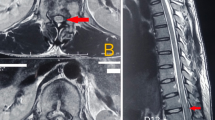
A 78-year-old man with a history of antiplatelet therapy for cerebral infarction slipped and fell on level surface. He had no neck pain. Physical examination revealed tetraplegia of American Spinal Injury Association impairment scale (AIS) D with a neurological level of injury of C6. Plain radiography did not indicate any evidence of fractures, while magnetic resonance imaging (MRI) indicated cervical spinal stenosis at the level of the C3–5 vertebrae (Fig. 1). We diagnosed it as cervical spinal cord injury without radiographic abnormality (SCIWORA). He was admitted for conservative care. On the next day after the injury, he had acute neck pain and developed a moderately high fever (37.8 °C) while he was lying at rest. There were no specific findings in other joints. He was administered nonsteroidal anti-inflammatory drugs. Three days after injury, his paralysis deteriorated to AIS C and his neurological level of injury went up to C4 accompanied by an inflammatory response; his white blood cell count and C-reactive protein levels were 8700/μL (normal range, 3500–9300/μL) and 9.70 mg/dL (normal range, 0–0.3 mg/dL), respectively. A cervical MRI revealed an increasing spinal stenosis at the level of the C4–5 vertebrae (Fig. 2). Computed tomography (CT) revealed calcification of the ligamentum flavum at the same level (Fig. 3).
C3 laminectomy and C4-5 laminoplasty were performed. A turbid fluid collection was found in the ligamentum flavum. A histopathological examination revealed evidence of CPPD crystals in the fluid, and neutrophils indicative of inflammatory changes were observed in the surrounding tissue (Fig. 4). The patient’s postoperative course was uneventful; his condition improved to AIS D on follow-up 1 year later.
Discussion
This patient’s course shows two important clinical issues. First, pseudogout attacks of the cervical ligamentum flavum can cause acute exacerbation of cervical myelopathy. Second, an aging population may be at a risk of developing SCIWORA and pseudogout.
Acute neck pain and fever are often caused by crowned dens syndrome or by crystal-induced arthritis of the lateral atlantoaxial joint in the elderly [3]. We previously reported a case of acute neck pain caused by pseudogout attack of calcified cervical ligamentum flavum [3]. There have been some reports of spinal canal stenosis due to CPPD crystal deposition [4]. Myelopathy due to deposition of CPPD crystals in the ligamentum flavum of the cervical spine has been occasionally reported [4]. However, there has been no report of acute exacerbation of cervical myelopathy due to a pseudogout attack of the cervical ligamentum flavum following SCIWORA. This clinical manifestation should be considered as a differential diagnosis in cases of acute neck pain and paralysis, especially when calcification of the cervical ligamentum flavum exists.
Neurological deterioration might be caused by secondary injury in SCI; nevertheless, recovery is spontaneous in most cases of SCIWORA [6]. In this case, we believe that pseudogout was the cause for acute fever and neck pain followed by exacerbation of the neurological findings.
Our institution is located in a rural district with a super-aged population (people aged 65 or older comprised 37.2% of the population in 2019) [7, 8]. Risk of SCIWORA increases with aging [2, 8], and its incidence rate is expected to increase as the population ages. Furthermore, aging is an independent risk factor for pseudogout [9]. With an aging population and an increase in the number of cases of SCIWORA, the patients with rapidly progressive neurological deterioration of myelopathy due to pseudogout in the cervical spine following SCIWORA may increase in the future.
For diagnosis of such cases, CT and MRI are important. In this case, MRI was used to assess spinal cord compression, but CT was added as it was difficult to identify the cause, which was noted as calcification of the cervical ligamentum flavum on the CT. In cases of acute exacerbation of myelopathy after trauma, spinal cord compression due to CPPD deposition should be considered as a differential diagnosis, and CT scan should be performed to support definitive diagnosis.
References
Richette P, Bardin T, Doherty M. An update on the epidemiology of calcium pyrophosphate dehydrate crystal deposition disease. Rheumatology. 2009;48:711–5.
Miyakoshi N, Suda K, Kudo D, Sakai H, Nakagawa Y, Mikami Y, et al. A nationwide survey on the incidence and characteristics of traumatic spinal cord injury in Japan in 2018. Spinal Cord. 2020. https://doi.org/10.1038/s41393-020-00533-0.
Kobayashi T, Miyakoshi N, Abe T, Kikuchi K, Noguchi H, Konno N, et al. Acute neck pain caused by pseudogout attack of calcified cervical yellow ligament: a case report. J Med Case Rep. 2016;10:133.
Baba H, Maezawa Y, Kawahara N, Tomita K, Fukusawa N, Imura S. Calcium crystal deposition in the ligamentum flavum of the cervical spine. Spine. 1993;18:2174–81.
Rosenthal AK, Ryan LM. Calcium pyrophosphate crystal deposition disease, pseudogout, and articular chondrocalcinosis. In: William J. Koopman, Larry W. Moreland editors. Arthritis and allied conditions: a textbook of Rheumatology. Williams & Wilkins, 2001; pp 2348–71.
Yelamarthy PKK, Chhabra HS, Vaccaro A, Vishwakarma G, Kluger P, Nanda A, et al. Management and prognosis of acute traumatic cervical central cord syndrome: systematic review and Spinal Cord Society-Spine Trauma Study Group position statement. Eur Spine J. 2019;28:2390–407.
Statistics Bureau of Japan. Current Population Estimate as of October 1, 2019. https://www.stat.go.jp/english/data/jinsui/2019np/index.html#a15k01-a. Accessed 24 Aug 2020.
Kudo D, Miyakoshi N, Hongo M, Kasukawa Y, Ishikawa Y, Ishikawa N, et al. An epidemiological study of traumatic spinal cord injuries in the fastest aging area in Japan. Spinal Cord. 2019;57:509–15.
Felson DT, Anderson JJ, Naimark A, Kannel W, Meenan RF. The prevalence of chondrocalcinosis in the elderly and its association with knee osteoarthritis: the Framingham study. J Rheumatol.1989;16:1241–5.
Acknowledgements
The authors thank Takeshi Ino for his help in date collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kimura, R., Miyakoshi, N., Kobayashi, T. et al. Acute exacerbation of cervical myelopathy caused by pseudogout of the cervical ligamentum flavum after cervical spinal cord injury: a case report. Spinal Cord Ser Cases 6, 98 (2020). https://doi.org/10.1038/s41394-020-00348-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-020-00348-4