Abstract
Study design
Cohort study.
Objectives
The objectives of this study were examination, observation and surgical interventions of pediatric patients with diastematomyelia, a rare congenital deformity of the spinal cord.
Setting
Spine surgery and neurosurgery clinic under ministry of health, the Russian Federation.
Methods
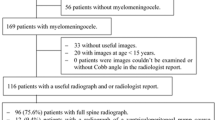
Twenty children (1–18 years of age) with diastematomyelia participated in this study. Diagnosis was based on subjects’ medical history, results of clinical examination, spine radiography in anteroposterior and lateral views, and neurophysiological examinations. Septum resection surgery was done in seventeen subjects.
Results
All the subjects had skin manifestations along the midline of the back. Neurological symptoms were noted in 17 subjects: paraparesis in 11, urinary incontinence in 2, monoparesis in 4, and spasticity in 2 subjects. Three subjects did not show any neurological deficit. Orthopedic examination revealed spinal deformities of various degrees of severity. In 4 subjects, partial restorations of neurological functions were observed; and in 1 subject, bladder incontinence developed after the surgery.
Conclusions
Patients who have limb length discrepancy, congenital scoliosis, skin manifestations should be examined for the presence of diastematomyelia. Patients having neither neurological deficit nor orthopedic deterioration should be monitored, and in case of deterioration, surgical treatment should be reserved. We advocate for performing resection of the septum in patients with diastematomyelia prior to surgical correction of scoliosis or orthopedic correction of lower limb deformities.
Similar content being viewed by others
Introduction
Diastematomyelia is a congenital anomaly of the spine characterized by the splitting of the spinal cord or cauda equina at the extent of one or few vertebra. It has been suggested that the cause of this anomaly is the presence of a connection between the neural tube and amniotic cavity or primitive bowel [1]. Spinal cord splitting occurs due to a bony, cartilaginous, or fibrotic septum which arises from the posterior surface of the anterior wall moving to the vertebral canal dorsally [2]. The term “diastematomyelia” defines the splitting of the cord itself but not the presence of the spur, and should not be mistaken with such conditions as “diplomyelia” and “true doubling of the spinal cord”. Herren and Edwards [3] described 43 cases of this condition, where the diagnosis was confirmed by postmortem in only 2. However, there is still no common classification method for this disease, and existing treatments are debatable [4].
Generally, it is easier to distinguish two types of diastematomyelia: type 1—with a bony spur, and type 2—with a fibrotic septum. This condition can be accompanied by other anomalies such as myelomeningoradiculocele or lipomeningoradiculocele. Kennedy [5] pointed out the variability of the amount and the types of these anomalies, especially in patients of different age groups. Most patients with diastematomyelia show clinical manifestations with severe neurologic and orthopedic pathology [6]. Congenital scoliosis, paralytic clubfoot, and lower limb discrepancy are the most commonly found associated symptoms. Meticulous neurologic examination can reveal deterioration of function, pain, progressive weakness, reflex asymmetry, bladder and bowel disturbances, paresis and spasticity, and sensation disturbances, etc. These symptoms occur due to spinal cord damage during continued growth with presence of fixation which leads to tension of the cord itself and vessels, and further microcirculatory and CSF disturbances [7]. Congenital scoliosis and different skin manifestations such as hemangiomas, local hypertrichosis or skin dimples, alone or in combination, might be evidence of diastematomyelia, which dictates the necessity for further investigation. A widening of the interpedicular space or bony spur might be noticed from the X-ray images, although the latter is rare, especially in cases of fibrotic septum or marked vertebra rotation. A system of evaluation and protocols of treatment for this group of patients are yet to be developed.
The aim of this study was to analyze and compare the neurological status, X-ray, CT, and MRI images, frequency of combination of diastematomyelia with skin signs and other musculoskeletal disorders in 20 pediatric patients. Methods of treatment for these subjects were based on the results of clinical and instrumental examination. Surgical intervention was performed in 17 out of 20 subjects. Partial restorations of neurological function were observed in four subjects, who underwent spur resection surgeries. No neurologic deterioration was observed in 16 subjects. In one subject, temporary bladder incontinence occurred, but gradually resolved within 5 months of surgery. Hence, we suggest surgical resection of the septum/spur in patients with diastematomyelia.
Methods
Twenty pediatric patients (12 females and 8 males), aged between 1 and 18 years were include in our study. All the subjects or their representatives signed an informed consent form for participation in the study. Detailed data of the subjects is presented in Table 1. Diagnosis was made based on the data of clinical evaluation, anteroposterior (AP) and lateral X-ray, CT, MRI, and electroneuromyography (ENMG) of the lower extremities. Clinical evaluation included neurological examination for motor function, perception, reflexes, and bladder and bowel functions. Interpedicular distance was measured on AP X-ray. The CT allowed to visualization of the bony spur for size, shape, and extension. MRI provided information about cartilaginous and fibrotic septums which could not be evaluated by X-ray or CT. The level of the conus and CSF flow disturbances were also monitored.
Electromyography (EMG) and ENMG were performed for (1) evaluation of conduction activity of the motor branches of the posterior tibial nerve and M-responses; (2) evaluation of conduction activity of the proximal motor structures (L5-S1 roots) and F-wave responses. CT, MRI, and electrophysiological investigations were performed in the pre- and postoperative periods.
Indications for surgical treatment, progressive neurological deterioration, and necessity for surgical correction of the spine deformity were then established. In these cases, spur removal was performed first, followed by corrective surgery in 1 or 2 months. Surgery was performed through a dorsal approach (Fig. 1). An incision was made in the area of the septum; and laminectomy was performed using a high-speed drill (Midas Rex MR7 Medtronic, USA). Total bony spur resection and spinal cord mobilization were carried out with microscope (OPMI, Vario ZEISS, Germany) and intraoperative neuromonitoring system (NIM-Response, Medtronic, USA). In case of bony spurs, we used a high-speed drill with tips of different sizes. When a fibrotic septum was present, the main goal was to mobilize the spinal cord in its caudal region where it is usually the most vulnerable to corrective forces during surgery. In these subjects, microsurgical septum transection and myeloradiculolysis were performed with IONM. None of the subjects had spinal cord damage during the surgery. After the removal of the septum/spur, the dura was sutured or replaced with a patch (Neuro-Patch, B-Braun, Germany) and the excised lamina was brought back on its place and sutured with ligatures. Microplates were used to secure the bone fragments for children older than 16 years of age. Verticalisation was allowed on 10–12 day post-surgery with additional fixation in a rigid thoracic lumbar sacral orthosis (TLSO). Seventeen subjects were treated surgically; 2 subjects were excluded from the surgery due to somatic diseases and in 1 subject with a fibrotic septum there were no indications for surgery. According to postoperative CTs and MRIs, bony spurs were totally absent in all 17 subjects and adequate mobilization of the spinal cord was achieved.
Results
The skin of all the subjects had signs at the region of the back, similar to local hypertrichosis, hemangiomas, or skin dimpling (a representative image is shown in Fig. 2). Widening of the interpedicular distance at the level of one or a few vertebral segments is a very distinctive feature for patients with diastematomyelia as shown in Fig. 3. In such cases, the presence of spinal cord splitting was clearly visualized on MRI (Fig. 4). CT images provided the necessary information to differentiate between bony and fibrotic septum (Fig. 5). In our population, 18 (90%) subjects had different types of congenital vertebral anomalies, including failure of formation, segmentation and a combination of aforementioned, while 17 (85%) subjects had congenital scoliosis. In 2 (10%) subjects with fibrotic septum, there were no congenital abnormalities. The most commonly seen musculoskeletal deformity in subjects with diastematomyelia was lower limb asymmetry. Atrophy with increasing muscle weakness was thought to be a case of neurological deterioration, thus being an indication for surgery. Partial restorations of neurological function were observed in total four subjects, for whom spur resection surgery was carried out.
Associated morbidities were noted in subjects with diastematomyelia as following: in 7 (35%) cases—paralytic clubfoot, in 3 (15%)—eningomyelocele, in 3 (15%)—lipoma of the vertebral canal, and in 1 (5%)—pyeloectasis. Table 1 shows characteristics of all the subjects. There were no specific EMG patterns related to whether it was a bony or fibrotic form of diastematomyelia or tethered cord. Usually, these subjects had clinical signs of myelopathy or radiculopathy based on the level of the septum.
Postoperatively, when the septum was completely removed (shown in Fig. 6) there was no neurologic deterioration in 16 subjects. In one subject, bladder incontinence developed after the surgery which included concomitant filum terminale transection and spinal cord mobilization with septum removal. Function of the bladder was gradually restored by 5 months post-surgery. Congenital scoliotic deformity correction was carried out in 10 subjects after the initial surgery due to continued curve progression. Subjects were surgically treated with complete removal of the anomalously developed vertebrae and spine instrumentation. The other 7 subjects were observed for a period of 1 to 4 years. No progression of the deformity was noticed during this period.
Discussion
According to many researchers [7,8,9], patients with diastematomyelia often have neurological impairment. Shaw [9] has shown that, in a series of 8 patients, 7 patients developed a progressive neurological deficit during growth which was initially absent. This served as an indication for surgical intervention. However, there was only a modest clinical improvement after surgery. Based on this result, the author recommended operative treatment as a prophylactic measure.
Our observations indicate that the patients with diastematomyelia that continue with neurologic deterioration have an unremoved septum or spur. Septum resection in the presence of neurological deficit might lead to partial neurological restoration in a small amount of patients, thus surgery should be recommended as a prophylactic measure as soon as any signs appear. In most cases the spine deformity is congenital. The most common types of anomaly in our patients were a failure of formation (hemivertebra) and failure of segmentation (unsegmented bar). Deformity of the spine was localized at the level of the spur in 11 patients; few patients had marked spine deformities above or below one, even in the absence of the vertebral anomalies. According to our observations, management of these deformities is necessary, and should be performed after the spur resection. Although this procedure alone does not completely resolve the pathology, in a few patients we observed no further progression of the deformity.
Winter et al. [10]. reported that about 5% of pediatric patients with congenital scoliosis had diastematomyelia. For this reason evaluation is recommended to exclude diastematomyelia in all patients with congenital deformities and widening of the vertebral canal on X-ray images. However, it is unknown whether there is a connection between the presence of the diastematomyelia and progression of the deformity. Based on the observational results of 27 patients with this condition, Winter et al [10]. concluded that abnormal vertebrae are the main reason for the progression of this condition. In contrast, Keim and Greene [11] could not reveal a connection between the diastematomyelia and progression of congenital scoliosis. Therefore, we believe that treatment of these patients should be based on the degree of the deformity and the rate of progression.
We conclude that in congenital scoliosis patients with LLD, skin manifestations should be examined for the presence of diastematomyelia. Progressive neurologic deterioration in these patients are due to the presence of the spur thus dictating the necessity for resection. Spur or septum removal should be performed prior to surgical correction of the spine or lower limb deformities. During the surgical procedure, laminoplasty rather than laminectomy is the preferred option as it helps to avoid the development of iatrogenic kyphosis and secures the dura during further deformity correction and metal implant installation. Patients, who have no neurological disturbances should be monitored closely and treated surgically in case of any deterioration.
References
Pang D, Dias MS, Ahab-Barmada M. Split cord malformation: Part I: A unified theory of embryogenesis for double spinal cord malformations. Neurosurgery. 1992;31:451–80.
Dias MS, Pang D. Split cord malformations. Neurosurg Clin N Am. 1995;6:339–58.
Herren RY, Edwards JE. Diplomyelia (duplication of the spinal cord). Arch Path. 1940;30:1203–14.
Bekki H, Morishita Y, Kawano O, Shiba K, Iwamoto Y. Diastematomyelia: A Surgical Case with Long-Term Follow-Up. Asian. Spine J. 2015;9:99–102.
Kennedy PR. New data on diastematomyelia. J Neurosurg. 1979;51:355–61.
Gan YC, Sgouros S, Walsh AR, Hockley AD. Diastematomyelia in children: treatment outcome and natural history of associated syringomyelia. Child’s Nerv Syst. 2007;23:515–9.
Miller A, Guille JT, Bowen JR. Evaluation and treatment of diastematomyelia. JBJS. 1993;75:1308–17.
Andersson H, Sullivan L. Diastematomyelia: report of two cases submitted to laminectomy. Acta Orthop Scand. 1965;36:257–64.
Shaw JF. Diastematomyelia. Dev Med Child Neurol. 1975;17:361–4.
Winter RB, Haven JJ, Moe JH, Lagaard SM. Diastematomyelia and congenital spine deformities. JBJS. 1974;56:27–39.
Keim HA, Greene AF. Diastematomyelia and Scoliosis. JBJS. 1973;55:1425–35.
Acknowledgements
The authors thank all the participants of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Vissarionov, S.V., Krutelev, N.A., Snischuk, V.P. et al. Diagnosis and treatment of diastematomyelia in children: a perspective cohort study. Spinal Cord Ser Cases 4, 109 (2018). https://doi.org/10.1038/s41394-018-0141-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-018-0141-0