Abstract
Introduction
Although multimodal intraoperative neuromonitoring (IONM), which has high sensitivity and specificity, is typically performed during spinal deformity surgery, neurological status may deteriorate with delay after surgical maneuvers. Here, we report a rare case of delayed postoperative neurological deficit (DPND) that was not detected by IONM during posterior spinal fusion (PSF) for congenital scoliosis.
Case presentation
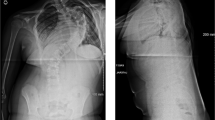
A 14-year-old male presented with congenital scoliosis associated with T3 and T10 hemivertebrae. Preoperative Cobb angle of proximal thoracic (PT) and main thoracic (MT) curves were 50° and 41°, respectively. PSF (T1-L1) without hemivertebrectomy was performed, and the curves were corrected to 31° and 21° in the PT and MT curves, respectively, without any abnormal findings in IONM, blood pressure, or hemoglobin level. However, postoperative neurological examination revealed complete loss of motor function. A revision surgery, release of the curve correction by removing the rods, was immediately performed and muscle strength completely recovered on the first postoperative day. Five days postoperatively, PSF was achieved with less curve correction (36° in the PT curve and 26° in the MT curve), without postoperative neurological deficits.
Discussion
Possible mechanisms of DPND in our patient are spinal cord ischemia due to spinal cord traction caused by scoliosis correction and spinal cord kinking by the pedicle at the concave side. Understanding the possible mechanisms of intra- and postoperative neural injury is essential for appropriate intervention in each situation. Additionally, IONM should be continued to at least skin closure to detect DPND observed in our patient.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 1 print issues and online access
We are sorry, but there is no personal subscription option available for your country.
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
All the data analyzed in this study are available from the corresponding author upon reasonable request.
References
Diab M, Smith AR, Kuklo TR. Neural complications in the surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2007;32:2759–63.
Cervellati S, Bettini N, Bianco T, Parisini P. Neurological complications in segmental spinal instrumentation: analysis of 750 patients. Eur Spine J. 1996;5:161–6.
Lall RR, Lall RR, Hauptman JS, Munoz C, Cybulski GR, Koski T, et al. Intraoperative neurophysiological monitoring in spine surgery: indications, efficacy, and role of the preoperative checklist. Neurosurg Focus. 2012;33:E10.
Biscevic M, Sehic A, Krupic F. Intraoperative neuromonitoring in spine deformity surgery: modalities, advantages, limitations, medicolegal issues - surgeons’ views. EFORT Open Rev. 2020;5:9–16.
Yoshida G, Ando M, Imagama S, Kawabata S, Yamada K, Kanchiku T, et al. Alert timing and corresponding intervention with intraoperative spinal cord monitoring for high-risk spinal surgery. Spine (Phila Pa 1976). 2019;44:E470–e9.
Chang JH, Hoernschemeyer DG, Sponseller PD. Delayed postoperative paralysis in adolescent idiopathic scoliosis: management with partial removal of hardware and staged correction. J Spinal Disord Tech. 2006;19:222–5.
Dapunt UA, Mok JM, Sharkey MS, Davis AA, Foster-Barber A, Diab M. Delayed presentation of tetraparesis following posterior thoracolumbar spinal fusion and instrumentation for adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2009;34:E936–41.
Keyoung HM, Kanter AS, Mummaneni PV. Delayed-onset neurological deficit following correction of severe thoracic kyphotic deformity. J Neurosurg Spine. 2008;8:74–9.
Early SD, Kay RM, Maguire MF, Skaggs DL. Delayed neurologic injury due to bone graft migration into the spinal canal following scoliosis surgery. Orthopedics. 2003;26:515–6.
Mineiro J, Weinstein SL. Delayed postoperative paraparesis in scoliosis surgery. A case report. Spine (Phila Pa 1976). 1997;22:1668–72.
Yoshida G, Hasegawa T, Yamato Y, Matsuyama Y. Delayed neuromonitoring alarm after scoliosis correction in Lenke type 4 adolescent idiopathic scoliosis. BMJ Case Rep. 2021;14:e242289.
Halsey MF, Myung KS, Ghag A, Vitale MG, Newton PO, de Kleuver M. Neurophysiological monitoring of spinal cord function during spinal deformity surgery: 2020 SRS neuromonitoring information statement. Spine Deform. 2020;8:591–6.
Bivona LJ, France J, Daly-Seiler CS, Burton DC, Dolan LA, Seale JJ, et al. Spinal deformity surgery is accompanied by serious complications: report from the Morbidity and Mortality Database of the Scoliosis Research Society from 2013 to 2020. Spine Deform. 2022;10:1307–13.
Auerbach JD, Kean K, Milby AH, Paonessa KJ, Dormans JP, Newton PO, et al. Delayed postoperative neurologic deficits in spinal deformity surgery. Spine (Phila Pa 1976). 2016;41:E131–8.
Qiao J, Xiao L, Zhu Z, Xu L, Qian B, Liu Z, et al. Delayed postoperative neurologic deficit after spine deformity surgery: analysis of 5377 cases at 1 institution. World Neurosurg. 2018;111:e160–e4.
Welling SE, Bauer JM. Delayed postoperative spinal cord ischemia after posterior spinal fusion in a pediatric patient with syrinx and decompressed chiari: a case report. JBJS Case Connect. 2020;10:e1900610.
Quinonez A, Pahys JM, Samdani AF, Hwang SW, Cahill PJ, Betz RR. Complete paraplegia 36 h after attempted posterior spinal fusion for severe adolescent idiopathic scoliosis: a case report. Spinal Cord Ser Cases. 2021;7:33.
Letts RM, Hollenberg C. Delayed paresis following spinal fusion with Harrington instrumentation. Clin Orthop Relat Res. 1977;125:45–8.
Taylor BA, Webb PJ, Hetreed M, Mulukutla RD, Farrell J. Delayed postoperative paraplegia with hypotension in adult revision scoliosis surgery. Spine (Phila Pa 1976). 1994;19:470–4.
Dolan EJ, Transfeldt EE, Tator CH, Simmons EH, Hughes KF. The effect of spinal distraction on regional spinal cord blood flow in cats. J Neurosurg. 1980;53:756–64.
Yahara Y, Seki S, Makino H, Watanabe K, Uehara M, Takahashi J, et al. Three-dimensional computed tomography analysis of spinal canal length increase after surgery for adolescent idiopathic scoliosis: a multicenter study. J Bone Joint Surg Am. 2019;101:48–55.
Watanabe K, Hosogane N, Kawakami N, Tsuji T, Toyama Y, Chiba K, et al. Increase in spinal longitudinal length by correction surgery for adolescent idiopathic scoliosis. Eur Spine J. 2012;21:1920–5.
Qiu Y, Wang S, Wang B, Yu Y, Zhu F, Zhu Z. Incidence and risk factors of neurological deficits of surgical correction for scoliosis: analysis of 1373 cases at one Chinese institution. Spine (Phila Pa 1976). 2008;33:519–26.
Ando K, Kobayashi K, Ito K, Tsushima M, Morozumi M, Tanaka S, et al. Wave change of intraoperative transcranial motor-evoked potentials during corrective fusion for syndromic and neuromuscular scoliosis. Oper Neurosurg (Hagerstown). 2019;16:53–8.
Sielatycki JA, Cerpa M, Baum G, Pham M, Thuet E, Lehman RA, et al. A novel MRI-based classification of spinal cord shape and CSF presence at the curve apex to assess risk of intraoperative neuromonitoring data loss with thoracic spinal deformity correction. Spine Deform. 2020;8:655–61.
Bridwell KH, Kuklo TR, Lewis SJ, Sweet FA, Lenke LG, Baldus C. String test measurement to assess the effect of spinal deformity correction on spinal canal length. Spine (Phila Pa 1976). 2001;26:2013–9.
Kobayashi K, Imagama S, Ito Z, Ando K, Hida T, Ito K, et al. Transcranial motor evoked potential waveform changes in corrective fusion for adolescent idiopathic scoliosis. J Neurosurg Pediatr. 2017;19:108–15.
Funding
No funds were received in support of this work.
Author information
Authors and Affiliations
Contributions
SO, MO, TH, HT, TM, KM, YM, and HD contributed to the conception of the study, data collection, and interpretation of the results. SO and MO contributed to drafting the manuscript. SO, MO, TH, HT, TM, KM, YM, HD, RH, NO, KF, HK, and KW contributed to the critical revisions and final approval of the version to be published.
Corresponding author
Ethics declarations
Ethical approval
The patient consented to the submission of this case report to the journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ohtsubo, S., Ohashi, M., Hirano, T. et al. Delayed paraparesis after posterior spinal fusion for congenital scoliosis: a case report. Spinal Cord Ser Cases 10, 24 (2024). https://doi.org/10.1038/s41394-024-00639-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-024-00639-0