Abstract
Purpose
The objective of this study was to test a low-carbohydrate diet (LCD) plus walking to reduce androgen deprivation therapy (ADT)-induced metabolic disturbances.
Materials and methods
This randomized multi-center trial of prostate cancer (PCa) patients initiating ADT was designed to compare an LCD (≤20g carbohydrate/day) plus walking (≥30 min for ≥5 days/week) intervention vs. control advised to maintain usual diet and exercise patterns. Primary outcome was change in insulin resistance by homeostatic model assessment at 6 months. To detect 20% reduction in insulin resistance, 100 men were required. The study was stopped early after randomizing 42 men due to slow accrual. Secondary outcomes included weight, body composition, lipids, and prostate-specific antigen (PSA). Changes from baseline were compared between arms using rank-sum tests.
Results
At 6 months, LCD/walking reduced insulin resistance by 4% vs. 36% increase in control (p = 0.13). At 3 months, vs. control, LCD/walking arm significantly lost weight (7.8kg; p<0.001), improved insulin resistance (↑36%; p = 0.015), hemoglobin A1c (↓3.3%; p = 0.01), high-density lipoprotein (HDL) (↑13%; p = 0.004), and triglyceride (↓37%; p = 0.036). At 6 months, weight loss (10.6kg; p<0.001) and HDL (↑27%; p = 0.003) remained significant. LCD/walking preserved total body bone mineral count (p = 0.025), reduced fat mass (p = 0.002), lean mass (p = 0.036), and percent body fat (p = 0.004). There were no differences in PSA. Limitations include the effect of LCD, weight loss vs. walking instruction are indistinguishable, and small sample size.
Conclusions
In an underpowered study, LCD/walking did not improve insulin sensitivity at 6 months. Given most secondary outcomes were improved at 3 months with some remaining improved at 6 months and a secondary analysis showed that LCD/walking reduced insulin resistance over the study, supporting future larger studies of LCD/walking intervention to reduce ADT-induced disturbances.
Similar content being viewed by others
Introduction
Androgen deprivation therapy (ADT) is a common and effective therapy for advanced and metastatic prostate cancer (PCa) [1, 2], but with metabolic disturbances including impaired glucose tolerance, insulin resistance, and weight gain, putting men at increased risk for diabetes and possibly cardiovascular (CV) death [3]. ADT-induced disturbances are compounded by the fact that men receiving ADT have a high baseline prevalence of CV risk factors [4]. Among non-diabetic men beginning ADT, within 12 weeks, whole-body insulin sensitivity index decreased by 11.0 ± 8% (p = 0.04), insulin resistance by homeostatic model assessment (HOMA, an estimation of insulin resistance based on fasting glucose and insulin concentrations) increased by 12.9 ± 5.8% (p = 0.02), and plasma insulin increased by 26 ± 9% (p = 0.04) [5]. This translates to a 40% increased diabetes risk [6], and worsening glucose control among diabetics on ADT [7]. Even when given for a limited time, such as adjuvant to radiotherapy, diabetes risk increases [8].
Beyond increasing diabetes risk, ADT promotes increased fat mass, elevated triglyceride and low-density lipoprotein (LDL) cholesterol [5], decreased libido, impotence, fatigue, osteoporosis, hot flushes, and loss of muscle mass. New treatments to prevent these sequelae are desperately needed.
The low-carbohydrate diet (LCD), which limits carbohydrate intake, results in dramatic weight loss and reductions in serum insulin, LDL, and triglycerides [9]. Thus, an LCD appears to favorably modulate many pathways that are unfavorably modified by ADT. We hypothesized that an LCD would prevent insulin resistance and other ADT-associated disturbances. In addition, exercise may also benefit PCa management [10]. We conducted a 6-month randomized clinical trial (RCT) among men initiating ADT comparing an LCD plus walking vs. a control arm.
Materials and methods
Study design
After obtaining institutional review board approval at each site (Duke University, Durham Veterans Affairs Medical Center [VAMC], and Greater Los Angeles VAMC), we conducted a multi-center phase II RCT of LCD plus walking advice vs. a control arm. Each participant signed a written consent. After confirming eligibility, participants completed a baseline visit and were randomized 1:1 to receive the intervention or control for 6 months. Randomization was conducted by permutated block design, stratified by center, and whether the participant received concurrent radiation for PCa. Data collection occurred at baseline, 3 months, and 6 months post randomization.
Intervention
LCD/walking arm was instructed by a dietitian to limit carbohydrate intake to ≤20g/day [11] and to walk ≥30 min/day for ≥5 days/week. Participants were provided a list of low-carbohydrate foods to choose from (e.g., greens, lean meat, and seafood) and a list of moderate/high carbohydrate foods to limit (e.g., bread, pasta, legumes, and starchy vegetables). Grains and starchy vegetables are high in carbohydrates (e.g., 1 slice of bread contains about 12g carbohydrate); thus, these food items are on the limit list. Sample menus and recipes were also provided. No other limits were given. Participants were coached by the dietitian in person or by phone weekly for months 0–3 and biweekly for months 4–6. During coaching, study dietitian answered questions and problem-solved with participants to help with diet adherence. Diet was assessed by 3-day food records [12] at each visit and analyzed by the Food Processor software (ESHA, version 10.14, Salem OR, USA). Participants were asked to measure urinary ketone weekly using provided ketone strips (Ketostix, Bayer Healthcare, Leverkusen, Germany). Control participants were asked to maintain usual dietary and exercise patterns.
Study participants
Key eligibility included men initiating ADT (LHRH-agonist, LHRH-antagonist, or orchiectomy) for PCa with an anticipated duration of ≥6 months, body mass index (BMI) ≥24kg/m2, and phone access for calls. Key exclusion criteria included symptomatic metastatic disease, medication-controlled diabetes, medications that interfere with insulin, already consuming an LCD, being vegetarian/vegan, or hemoglobin A1c (HbA1c) >7%.
Sample size and recruitment
Assuming the standard deviation of the change in HOMA from baseline to 6 months is 30% [5], with a sample size of 100 participants (50/group) completing the study, there was 91% power to detect a clinically meaningful ≥20% difference between arms for change in HOMA using a two-sided t test (α = 0.05). According to a large RCT of lifestyle intervention vs. control for diabetes prevention, lifestyle intervention decreased HOMA insulin resistance by 28% (from baseline to 12 months), which translated into a 58% reduction in diabetes risk [13]. Therefore, we chose 20% change in HOMA as a clinically meaningful cutoff.
Data collection and analysis
At each visit, weight (without shoes and in light clothing) and height were measured, fasting blood collected, and adverse events assessed. Adverse events were rated as mild, moderate, or severe based on pre-determined study definitions. Body composition including total fat body mass (FBM), fat percent, lean body mass (LBM), bone mineral content (BMC, the amount of bone mineral), and bone mineral density (BMD, the ratio of BMC over measured bone area) was measured using DEXA (Lunar DPX Duo®, GE Healthcare) at baseline and 6 months. Fasting blood was analyzed for insulin, glucose, prostate-specific antigen (PSA), lipids, and high-sensitivity C-reactive protein (hsCRP). PSA, glucose, and lipids were measured by commercial laboratories (LabCorp for Duke and Durham VAMC; Greater LA VAMC clinical lab for Greater LA VAMC). Insulin was measured in an electrochemiluminescent immunoassay using an SI-2400 imager and assay kits from Meso Scale Discovery (Rockville, MD, USA) by Duke Immunoassay Laboratory. HOMA was calculated using the approximation (glucose ×insulin)/22.5. Physical activity was measured by the Godin–Leisure questionnaire [14] and exercise capacity by a 6-min walk test. Quality of life was also assessed with the SF-36 questionnaire, which provided data to be calculated into a Global Health Composite Score [15]. The leading investigator (SJF) was blinded to the randomization and not involved in data collection.
Statistical analysis
Intervention adherence was assessed by comparing dietary intakes with the rank-sum test at each visit. The primary outcome was percent change in HOMA at 6 months between arms, which was tested using the rank-sum test (though power calculations were based upon t test, data were not normally distributed and thus a rank-sum test was used). Secondary outcomes included changes in anthropometric and various health measures from baseline to 3 and 6 months, which were compared using a rank-sum test . In a secondary analysis, change in HOMA over the three study visits among all men randomized was tested using a linear mixed model with an interaction term and main effects for treatment, study visit, and a random effect for participant. With the exception of the secondary analyses using a linear mixed model, which used all randomized men, all other analyses were limited to men who finished the study with available HOMA data at all three study visits.
Statistical analyses were completed using Stata 13.1 (Stata Corp., College Station, TX, USA). Two-sided p < 0.05 was considered statistically significant.
Results
Enrollment
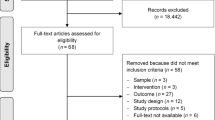
Due to slow accrual and budget constraints, recruitment was discontinued after 45 participants were enrolled. Precise measurements of why accrual was slow were not captured; however, our anecdotal experience is that given the baseline visit needed to occur prior to starting ADT and then collect dietary data over a week prior to ADT, many men were unwilling to delay ADT to enroll on the study. Lack of interest in the diet was lesser of a concern but did occur.
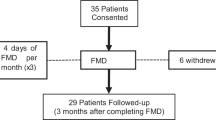
Among 45 men enrolled, 42 were randomized (N = 20 to LCD, N=22 to control) (Fig. 1). Following randomization, 40 participants completed baseline visits (N = 19 LCD, N = 21 control) and 37 completed the 3-month visit (N = 17 LCD, N = 20 control). In total, 14 LCD participants completed the 6-month visit, of which 11 had complete data including blood at baseline and 6 months. Twenty control participants completed the 6-month visit, of which 18 had complete data including blood at baseline and 6 months. Dropout was 6 in the LCD arm (6/20 = 30%) vs. 2 in the control (2/22 = 9%), p = 0.12 (Fisher’s exact)
Participant population
Participants who completed the 6-month visit were similar between arms at baseline (Table 1). When the 11 randomized men who did not complete all study data collection were included in the comparison, baseline characteristics were still balanced between arms (not shown).
Dietary intakes
At baseline, both arms consumed similar amounts of carbohydrate, fat, protein, and calories (Table 2). At both 3 and 6 months, LCD/walking participants consumed less carbohydrates (p<0.01) but greater protein (p<0.05) vs. controls, while fat and caloric intake remained similar between arms. Carbohydrate intake reduced from 227.3 to 74.4 g/day at 3 months and remained constant at 78.9g/day at 6 months in the LCD/walking arm.
Primary outcome
At 6 months, the LCD/walking arm decreased HOMA by 4% vs. 36% increase in the controls (p = 0.13) (Table 3). Thus, there was no difference in the primary outcome. In a secondary analysis, there was a significant interaction between treatment and visit in predicting HOMA among all randomized participants (LCD/walking plus controls, n = 40), indicating that the LCD/walking led to significant changes in HOMA across the three time points of the study (Fig. 2, p = 0.006).
Secondary outcome: glucose metabolism
At 3 months, HOMA decreased in the LCD/walking vs. controls (median change: −19 vs. 7%, p = 0.015). All glycemic markers including fasting glucose, insulin, and HbA1c increased in the controls but decreased in LCD/walking (p < 0.05 for all comparisons between arms except fasting glucose, Table 3). While similar trends were seen at 6 months, no marker was significantly different between arms.
Secondary outcome: anthropometric measures
At 3 months, median weight loss in LCD/walking participants was 7.5 vs. 0.3 kg gain for controls (Table 3). At 6 months, median weight loss in LCD/walking increased to 9.3 kg vs. median 1.3 kg gain in controls. LCD/walking participants reduced BMI by 7.4% at 3 months and 9% at 6 months, whereas controls increased 0.5% and 1.4%, respectively. The weight and BMI changes at both visits were significantly different between arms (all p < 0.001).
Secondary outcome: lipid metabolism and inflammatory measures
At both visits, there was no significant difference in the percent changes between arms in total, LDL, and non-HDL cholesterols. In contrast, HDL increased significantly more in the LCD/walking vs. controls at both 3 months (p = 0.004) and 6 months (p = 0.003). Triglycerides showed an opposite direction of percent change with significant decreases in LCD/walking at 3 months (p = 0.036) and non-significant trends toward lower levels at 6 months (p = 0.086). The percent changes in PSA and HsCRP were not significantly different between arms at both visits.
Secondary outcome: body composition and exercise measures
At 6 months, the LCD/walking arm maintained total body BMC (0.14%) vs. controls who lost BMC (−2.32%) (p = 0.025) (Table 4). Median percent total BMD change at 6 months did not differ between arms, but the controls tended to decrease more (−1.12% vs. −0.13%, p = 0.064). The LCD/walking arm also had greater median percent decrease in FBM (−16.18%; p = 0.002), LBM (−7.31%; p = 0.036), and percent body fat (−8.35%; p = 0.004) vs. controls, which gained both FBM (10.99%) and percent body fat (10.43%). LCD/walking arm increased physical activity significantly only at 3 months. The exercise capacity measured by 6-min walk was not different between arms at any visit.
Secondary outcome: adverse events
Participants in both arms reported adverse events of varying degree of severity. During months 0–3, the LCD/walking arm reported 13 mild and 5 moderate events vs. 1 mild and 1 moderate in controls. Most adverse events in the LCD/walking arm were fatigue, constipation, and headaches. During months 4–6, there were no differences in events reported by arm (4 mild in LCD/walking; 3 mild and 4 moderate in controls). There were no severe adverse events reported.
Discussion
Within the context of an underpowered RCT that closed early, we found that an LCD plus walking intervention did not improve insulin sensitivity after ADT at 6 months. However, there were significant improvements in many secondary outcomes at 3 months (weight loss, insulin sensitivity, HDL, and triglyceride) with some maintained up to 6 months (weight loss, increased HDL, and preserved bone mineral status). In contrast, the control arm showed several common ADT disturbances including weight gain, increased insulin resistance, loss of BMC and LBM, and increased FBM and fat percentage. Our findings support previous research that ADT adversely impacts various CV risk factors and bone status [16,17,18]. Despite the negative primary outcome, given the underpowered nature of the study and the many positive secondary outcomes including the secondary finding that the intervention significantly reduced insulin resistance over the study, our data support further study of an LCD/walking intervention to mitigate the adverse ADT effects.
As the control participants were asked to maintain their usual dietary and exercise patterns and they experienced well-known ADT side effects, they served as a true control group to test whether a lifestyle intervention can mitigate the metabolic disturbances of ADT. Within this context, the LCD/walking intervention was effective in weight loss and the improvement in insulin sensitivity was significant at 3 months. Even though weight loss continued into 6 months in LCD/walking and the carbohydrate restriction stayed consistent, insulin resistance (HOMA) and other glycemic markers (fasting glucose, insulin) all showed a reversed trend such that insulin resistance (the primary outcome) was not significant at 6 months. This finding suggests that the initial improvement in insulin sensitivity (reduction in insulin resistance) at 3 months may have been contributed by separate mechanisms from the impact of weight loss and/or carbohydrate restriction or adaptations of the mechanism reversed the trend in the glycemic markers after the first 3 months. We are not aware of any lifestyle intervention in PCa patients that led to similar temporary changes that later returned to baseline. However, similar reversal pattern was recently reported in adiponectin and triglyceride levels of a weight loss trial of women without cancer [19]. These data support further study to test whether an LCD/walking intervention can effectively reverse the ADT disturbances on glycemic markers and diabetes risk long term [19, 20]. Previous research also suggested that ADT may worsen glycemic metabolism through the increase in subcutaneous vs. visceral fat [21], which differs from the common characteristics of metabolic syndrome [22]. Future studies are needed to understand the mechanisms of how ADT affects glycemic markers and the degree to which an LCD/walking can prevent these effects long term.
The impact of ADT on lipids has been mixed in previous studies. Some studies showed ADT increased total, LDL, and HDL cholesterol [21, 23,24,25], while others found ADT had no impact on HDL [26, 27] or decreased it [28] and the impact may depend on ADT duration [29]. In our small study, ADT did not impact total, LDL, or non-HDL cholesterol. However, the LCD/walking intervention increased HDL significantly more at both visits and reduced triglyceride significantly more at 3 months vs. controls. Previous studies also showed that ADT increased triglyceride significantly [21, 30, 31]. The benefit of the LCD/walking on triglyceride may be contributed by the weight loss in conjunction with carbohydrate restriction. Thus, our intervention was effective in improving two separate risk factors for metabolic syndrome (HDL and triglyceride), which is common among PCa patients.
As expected, the control arm in our study showed a reduction in BMC and LBM, and increased FBM. The LCD/walking was effective in preserving bone status and reducing FBM. Even though LCD/walking lost more LBM than the controls, this is likely a reflection of the greater weight loss in the LCD/walking arm, a common finding with weight loss [32]. However, a systematic review showed that diet-induced weight loss reduces muscle mass without adversely affecting muscle strength [33]. Further, weight loss improves global physical function likely due to reduced fat mass. Future studies of LCD should include measurement of muscle strength. Very few studies included both dietary and exercise intervention among PCa patients undergoing ADT. A supervised 3-month exercise program preserved appendicular lean mass and reduced fat mass, but had no impact on BMD [34]. Another 6 months intervention combining metformin, a low glycemic dietary advice, and aerobic exercise improved abdominal girth and weight, but did not improve insulin sensitivity and lipid metabolism [35]. Bone density was not measured in this study. A recent meta-analysis of 14 studies (N = 1135) concluded that exercise improved muscle strength, FBM, and BMI, but had no impact on BMD and cardiometabolic markers [36]. Thus, it is promising that our intervention negated adverse effects of ADT from multiple areas including glycemic markers, insulin resistance, HDL, triglycerides, body composition, and bone density despite the improvement in insulin resistance and glycemic markers was only for 3 months. In particular, as noted most physical activity trials have shown no effect on bone content. Thus, it is unlikely that our walking advice prevented bone loss but most likely due to the weight loss from the LCD, though the underlying mechanisms are unknown.
Overall, our study confirmed the adverse metabolic effects of ADT and supports a careful screening for risk for diabetes and CVD prior to initiating ADT. Our study had limitations. First, the study was discontinued early due to slow accrual and budget constraint so that 45 of 100 targeted was enrolled. As noted, the exact reasons for low accrual are unknown. Some patients refused to participate in the study because they consider dietary intervention as an additional burden despite the potential benefit. On the other hand, some refused to participate because of the possibility of being randomized to the control group. Transportation to clinical site due to distance was also a barrier for some. Future studies incorporating strategies such as delayed intervention and home visit for data collection may mitigate the barriers and improve recruitment. The underpowered sample size likely contributed to our overall negative findings. Indeed, the intervention resulted in greater improvements (40%) in insulin resistance than initially estimated (20%), though results were not statistically significant. As such, we cannot conclude that a larger study would have been positive—this remains to be tested. Nonetheless, despite the decreased power, many secondary outcomes were positive. Further, we cannot distinguish the effect of LCD from the walking advice or from weight loss. Nevertheless, prior studies of exercise alone (not just walking advice) have shown no improvements in bone content or insulin [34,35,36], and thus we speculate that most of the benefits are due to the diet, weight loss, or combination. The carbohydrate intake of the LCD/walking participants was not as compliant as the study intended of ≤20 g/day. The level of carbohydrate intake was feasible and not restricted, yet with promising benefits. Whether a greater compliance would result in even greater benefits remains to be tested. Though dropout was numerically higher in the LCD/walking arm, this was not significant. Moreover, adverse events, while mainly mild to moderate and predominantly limited to the first 3 months, were greater in the intervention arm. Collectively, this suggests that the LCD may not fit for all participants and personalization of the intervention may lead to greater adherence and efficacy.
Conclusions
In an underpowered study, an LCD plus walking intervention did not improve insulin sensitivity at 6 months for men starting ADT. However, the intervention improved many secondary outcomes—especially at 3 months—and a secondary analysis indicated that the intervention reduced insulin resistance significantly over the study supporting future studies to explore new feasibility strategies, mechanistic pathways of the changes in markers, and with larger sample sizes to test whether LCD can mitigate the metabolic disturbances of ADT.
References
Liede A, Hallett DC, Hope K, Graham A, Arellano J, Shahinian VB. International survey of androgen deprivation therapy (ADT) for non-metastatic prostate cancer in 19 countries. ESMO Open. 2016;1:e000040.
Gilbert SM, Kuo YF, Shahinian VB. Prevalent and incident use of androgen deprivation therapy among men with prostate cancer in the United States. Urol Oncol. 2011;29:647–53.
Ahmadi H, Daneshmand S. Androgen deprivation therapy for prostate cancer: long-term safety and patient outcomes. Patient Relat Outcome Meas. 2014;5:63–70.
Davis MK, Rajala JL, Tyldesley S, Pickles T, Virani SA. The prevalence of cardiac risk factors in men with localized prostate cancer undergoing androgen deprivation therapy in British Columbia, Canada. J Oncol. 2015;2015:820403.
Smith MR, Lee H, Nathan DM. Insulin sensitivity during combined androgen blockade for prostate cancer. J Clin Endocrinol Metab. 2006;91:1305–8.
Keating NL, O'Malley AJ, Smith MR. Diabetes and cardiovascular disease during androgen deprivation therapy for prostate cancer. J Clin Oncol. 2006;24:4448–56.
Keating NL, Liu PH, O'Malley AJ, Freedland SJ, Smith MR. Androgen-deprivation therapy and diabetes control among diabetic men with prostate cancer. Eur Urol. 2014;65:816–24.
Crawley D, Garmo H, Rudman S, Stattin P, Haggstrom C, Zethelius B, et al. Association between duration and type of androgen deprivation therapy and risk of diabetes in men with prostate cancer. Int J Cancer. 2016;139:2698–704.
Gardner CD, Kiazand A, Alhassan S, Kim S, Stafford RS, Balise RR, et al. Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial. JAMA. 2007;297:969–77.
Finlay A, Wittert G, Short CE. A systematic review of physical activity-based behaviour change interventions reaching men with prostate cancer. J Cancer Surviv. 2018;12:571–91.
ATKINS 20®: An effective diet for weight loss: Atkins Foundation. https://www.atkins.com/how-it-works/atkins-20.
Thompson FE, Kirkpatrick SI, Subar AF, Reedy J, Schap TE, Wilson MM, et al. The National Cancer Institute's Dietary Assessment Primer: a resource for diet research. J Acad Nutr Diet. 2015;115:1986–95.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Amireault S, Godin G, Lacombe J, Sabiston CM. Validation of the Godin–Shephard Leisure-Time Physical Activity Questionnaire classification coding system using accelerometer assessment among breast cancer survivors. J Cancer Surviv. 2015;9:532–40.
Hagell P, Westergren A, Arestedt K. Beware of the origin of numbers: standard scoring of the SF-12 and SF-36 summary measures distorts measurement and score interpretations. Res Nurs Health. 2017;40:378–86.
Morote J, Gomez-Caamano A, Alvarez-Ossorio JL, Pesqueira D, Tabernero A, Gomez Veiga F, et al. The metabolic syndrome and its components in patients with prostate cancer on androgen deprivation therapy. J Urol. 2015;193:1963–9.
Gandaglia G, Sun M, Popa I, Schiffmann J, Trudeau V, Shariat SF, et al. Cardiovascular mortality in patients with metastatic prostate cancer exposed to androgen deprivation therapy: a population-based study. Clin Genitourin Cancer. 2015;13:e123–30.
Wang A, Karunasinghe N, Plank L, Zhu S, Osborne S, Bishop K, et al. Effect of androgen deprivation therapy on bone mineral density in a Prostate Cancer Cohort in New Zealand: A Pilot Study. Clin Med Insights Oncol. 2017;11:1179554917733449.
Teoh JY, Chiu PK, Chan SY, Poon DM, Cheung HY, Hou SS, et al. Risk of new-onset diabetes after androgen deprivation therapy for prostate cancer in the Asian population. J Diabetes. 2015;7:672–80.
Derweesh IH, Diblasio CJ, Kincade MC, Malcolm JB, Lamar KD, Patterson AL, et al. Risk of new-onset diabetes mellitus and worsening glycaemic variables for established diabetes in men undergoing androgen-deprivation therapy for prostate cancer. BJU Int. 2007;100:1060–5.
Mitsuzuka K, Kyan A, Sato T, Orikasa K, Miyazato M, Aoki H, et al. Influence of 1 year of androgen deprivation therapy on lipid and glucose metabolism and fat accumulation in Japanese patients with prostate cancer. Prostate Cancer Prostatic Dis. 2016;19:57–62.
Smith MR, Lee H, McGovern F, Fallon MA, Goode M, Zietman AL, et al. Metabolic changes during gonadotropin-releasing hormone agonist therapy for prostate cancer: differences from the classic metabolic syndrome. Cancer . 2008;112:2188–94.
Oka R, Utsumi T, Endo T, Yano M, Kamijima S, Kamiya N, et al. Effect of androgen deprivation therapy on arterial stiffness and serum lipid profile changes in patients with prostate cancer: a prospective study of initial 6-month follow-up. Int J Clin Oncol. 2016;21:389–96.
Nguyen PL, Jarolim P, Basaria S, Zuflacht JP, Milian J, Kadivar S, et al. Androgen deprivation therapy reversibly increases endothelium-dependent vasodilation in men with prostate cancer. J Am Heart Assoc. 2015;4:e001914.
Dockery F, Bulpitt CJ, Agarwal S, Donaldson M, Rajkumar C. Testosterone suppression in men with prostate cancer leads to an increase in arterial stiffness and hyperinsulinaemia. Clin Sci (Lond). 2003;104:195–201.
Ziaran S, Goncalves FM, Breza J Sr. Patients with prostate cancer treated by ADT have significantly higher fibrinogenemia than healthy control. World J Urol. 2013;31:289–92.
Torimoto K, Samma S, Kagebayashi Y, Chihara Y, Tanaka N, Hirayama A, et al. The effects of androgen deprivation therapy on lipid metabolism and body composition in Japanese patients with prostate cancer. Jpn J Clin Oncol. 2011;41:577–81.
Saglam HS, Kose O, Kumsar S, Budak S, Adsan O. Fasting blood glucose and lipid profile alterations following twelve-month androgen deprivation therapy in men with prostate cancer. Scientific World J. 2012;2012:696329.
Salvador C, Planas J, Agreda F, Placer J, Trilla E, Lopez MA, et al. Analysis of the lipid profile and atherogenic risk during androgen deprivation therapy in prostate cancer patients. Urol Int. 2013;90:41–4.
Eri LM, Haug E, Tveter KJ. Effects on the endocrine system of long-term treatment with the non-steroidal anti-androgen Casodex in patients with benign prostatic hyperplasia. Br J Urol. 1995;75:335–40.
Smith MR, Finkelstein JS, McGovern FJ, Zietman AL, Fallon MA, Schoenfeld DA, et al. Changes in body composition during androgen deprivation therapy for prostate cancer. J Clin Endocrinol Metab. 2002;87:599–603.
Weinheimer EM, Sands LP, Campbell WW. A systematic review of the separate and combined effects of energy restriction and exercise on fat-free mass in middle-aged and older adults: implications for sarcopenic obesity. Nutr Rev. 2010;68:375–88.
Cava E, Yeat NC, Mittendorfer B. Preserving healthy muscle during weight loss. Adv Nutr. 2017;8:511–9.
Cormie P, Galvao DA, Spry N, Joseph D, Chee R, Taaffe DR, et al. Can supervised exercise prevent treatment toxicity in patients with prostate cancer initiating androgen-deprivation therapy: a randomised controlled trial. BJU Int. 2015;115:256–66.
Nobes JP, Langley SE, Klopper T, Russell-Jones D, Laing RW. A prospective, randomized pilot study evaluating the effects of metformin and lifestyle intervention on patients with prostate cancer receiving androgen deprivation therapy. BJU Int. 2012;109:1495–502.
Yunfeng G, Weiyang H, Xueyang H, Yilong H, Xin G. Exercise overcome adverse effects among prostate cancer patients receiving androgen deprivation therapy: an update meta-analysis. Medicine (Baltimore). 2017;96:e7368.
Acknowledgements
This study was funded by the Atkins Foundation, AUA, NIH K24 CA160653.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Freedland, S.J., Howard, L., Allen, J. et al. A lifestyle intervention of weight loss via a low-carbohydrate diet plus walking to reduce metabolic disturbances caused by androgen deprivation therapy among prostate cancer patients: carbohydrate and prostate study 1 (CAPS1) randomized controlled trial. Prostate Cancer Prostatic Dis 22, 428–437 (2019). https://doi.org/10.1038/s41391-019-0126-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-019-0126-5
This article is cited by
-
Plant-based diets to reduce prostate cancer risk and improve prostate cancer outcomes—ready for prime time?
Prostate Cancer and Prostatic Diseases (2023)
-
Dietary interventions to improve body composition in men treated with androgen deprivation therapy for prostate cancer: a solution for the growing problem?
Prostate Cancer and Prostatic Diseases (2022)