Abstract
Background
Osteopontin (OPN) is an important breastmilk protein involved in infant intestinal, immunological, and brain development. However, little is known about how common milk pasteurization and storage techniques affect this important bioactive protein.
Methods
Human milk osteopontin concentration was measured in single-donor fresh (n = 1) or frozen (n = 20) breastmilk, pooled Holder-pasteurized donor breastmilk (n = 11), and a shelf-stable (retort pasteurized) breastmilk product (n = 2) by ELISA. Single-donor breastmilk samples were subjected to pasteurization and/or freezing before measuring osteopontin concentrations.
Results
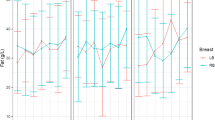
Holder pasteurization of breastmilk resulted in an ∼50% decrease in osteopontin concentration within single-donor samples. Breastmilk from mothers of preterm infants trended toward higher osteopontin concentration than mothers of term infants; however, samples from preterm mothers experienced greater osteopontin degradation upon pasteurization. A commercial breastmilk product that underwent retort pasteurization had lower osteopontin concentration than a Holder-pasteurized pooled breastmilk product. Finally, freezing breastmilk prior to Holder pasteurization resulted in less osteopontin degradation than Holder pasteurization prior to freezing.
Conclusions
Commonly used breastmilk pasteurization and storage techniques, including freezing and Holder pasteurization, decrease the concentration of the bioactive protein osteopontin in human breastmilk. Holder pasteurization reduced osteopontin concentration by an average of 63%, while freezing resulted in an 8–12% decrease.
Impact
-
Pasteurization of human breastmilk significantly decreases the concentration of the bioactive protein osteopontin.
-
Use of both pasteurization and freezing techniques for breastmilk preservation results in greater loss of osteopontin.
-
This study presents for the first time an analysis of osteopontin concentrations in single-donor pasteurized milk samples.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Liu, L. et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 385, 430–440 (2015).
Martin, J., Hamilton, B. & Osterman, M. Births in the United States, 2021. NCHS Data Brief. 1–8 (2022).
Steiner, L., Diesner, S. C. & Voitl, P. Risk of infection in the first year of life in preterm children: an Austrian observational study. PLoS ONE 14, e0224766 (2019).
Manzoni, P. et al. Human milk feeding prevents retinopathy of prematurity (ROP) in preterm VLBW neonates. Early Hum. Dev. 89, S64–S68 (2013).
Furman, L., Taylor, G., Minich, N. & Hack, M. The effect of maternal milk on neonatal morbidity of very low-birth-weight infants. Arch. Pediatr. Adolesc. Med. 157, 66–71 (2003).
Schanler, R. J., Shulman, R. J. & Lau, C. Feeding strategies for premature infants: beneficial outcomes of feeding fortified human milk versus preterm formula. Pediatrics 103, 1150–1157 (1999).
Schanler, R. J. Outcomes of human milk-fed premature infants. Semin. Perinatol. 35, 29–33 (2011).
Quigley, M., Embleton, N. D. & McGuire, W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst. Rev. 7, CD002971 (2019).
Mothers’ Milk Bank Northeast. Comparison of Holder pasteurized (frozen) and retort processed (shelf-stable) human milk. https://milkbankne.org/wp-content/uploads/2017/11/Holder-vs-Shelf-Stable-Human-Milk-MMBNE.pdf (2017).
Ballard, O. & Morrow, A. L. Human milk composition: nutrients and bioactive factors. Pediatr. Clin. North Am. 60, 49 (2013).
Dawod, B. & Marshall, J. S. Cytokines and soluble receptors in breast milk as enhancers of oral tolerance development. Front. Immunol. 10, 16 (2019).
Hegar, B. et al. The role of two human milk oligosaccharides, 2′-fucosyllactose and lacto-N-neotetraose, in infant nutrition. Pediatr. Gastroenterol. Hepatol. Nutr. 22, 330 (2019).
Witkowska-Zimny, M. & Kaminska-El-Hassan, E. Cells of human breast milk. Cell. Mol. Biol. Lett. 22, 11 (2017).
Binte Abu Bakar, S. Y., Salim, M., Clulow, A. J., Nicholas, K. R. & Boyd, B. J. Human milk composition and the effects of pasteurisation on the activity of its components. Trends Food Sci. Technol. 111, 166–174 (2021).
Adhisivam, B. et al. Effect of Holder pasteurization on macronutrients and immunoglobulin profile of pooled donor human milk. J. Matern. Fetal Neonatal Med. 32, 3016–3019 (2019).
Paulaviciene, I. J. et al. The effect of prolonged freezing and Holder pasteurization on the macronutrient and bioactive protein compositions of human milk. Breastfeed. Med. 15, 583–588 (2020).
Peila, C. et al. The effect of Holder pasteurization on nutrients and biologically-active components in donor human milk: a review. Nutrients 8, 477 (2016).
Lima, H. K., Wagner-Gillespie, M., Perrin, M. T. & Fogleman, A. D. Bacteria and bioactivity in Holder pasteurized and shelf-stable human milk products. Curr. Dev. Nutr. 1, e001438 (2017).
Meredith-Dennis, L. et al. Composition and variation of macronutrients, immune proteins, and human milk oligosaccharides in human milk from nonprofit and commercial milk banks. J. Hum. Lact. 34, 120–129 (2018).
Lima, H. K. et al. Effect of Holder pasteurization and retort processing on bioactive components and nutritional content of human milk. FASEB J. 31, 958.19 (2017).
Wu, T. et al. Availability of donor milk improves enteral feeding but has limited effect on body growth of infants with very-low birthweight: data from a historic cohort study. Matern. Child Nutr. 18, e13319 (2022).
Li, Y. et al. Pasteurization procedures for donor human milk affect body growth, intestinal structure, and resistance against bacterial infections in preterm pigs. J. Nutr. 147, 1121–1130 (2017).
Donovan, S. M. et al. Bovine osteopontin modifies the intestinal transcriptome of formula-fed infant rhesus monkeys to be more similar to those that were breastfed. J. Nutr. https://doi.org/10.3945/jn.114.197558 (2014).
West, C. E. et al. Effects of osteopontin-enriched formula on lymphocyte subsets in the first 6 months of life: a randomized controlled trial. Pediatr. Res. https://doi.org/10.1038/pr.2017.77 (2017).
Lonnerdal, B., Kvistgaard, A. S., Peerson, J. M., Donovan, S. M. & Peng, Y. M. Growth, nutrition, and cytokine response of breast-fed infants and infants fed formula with added bovine osteopontin. J. Pediatr. Gastroenterol. Nutr. 62, 650–657 (2016).
Standal, T., Børset, M. & Sundan, A. Role of osteopontin in adhesion, migration, cell survival and bone remodeling. Exp. Oncol. 26, 179–184 (2004).
Lund, S. A., Giachelli, C. M. & Scatena, M. The role of osteopontin in inflammatory processes. J. Cell Commun. Signal. 3, 311–322 (2009).
Hunter, G. K., Kyle, C. L. & Goldberg, H. A. Modulation of crystal formation by bone phosphoproteins: structural specificity of the osteopontin-mediated inhibition of hydroxyapatite formation. Biochem. J. 300, 723–728 (1994).
Jiang, R. & Lönnerdal, B. Osteopontin in human milk and infant formula affects infant plasma osteopontin concentrations. Pediatr. Res. 85, 502–505 (2019).
Bruun, S. et al. Osteopontin levels in human milk vary across countries and within lactation period: data from a multicenter study. J. Pediatr. Gastroenterol. Nutr. 67, 250–256 (2018).
Jiang, R., Prell, C. & Lönnerdal, B. Milk osteopontin promotes brain development by up-regulating osteopontin in the brain in early life. FASEB J. 33, 1681–1694 (2019).
Jiang, R., Prell, C. & Lönnerdal, B. Milk osteopontin promotes brain development by up-regulating osteopontin in the brain in early life. FASEB J. https://doi.org/10.1096/fj.201701290RR (2019).
Liang, N. et al. Structural and functional changes of bioactive proteins in donor human milk treated by vat-pasteurization, retort sterilization, ultra-high-temperature sterilization, freeze-thawing and homogenization. Front. Nutr. 9, 926814 (2022).
Zhu, J. et al. Longitudinal changes of lactopontin (milk osteopontin) in term and preterm human milk. Front. Nutr. 9, 1738 (2022).
Liu, L., Jiang, R. & Lönnerdal, B. Assessment of bioactivities of the human milk lactoferrin–osteopontin complex in vitro. J. Nutr. Biochem. 69, 10–18 (2019).
Nazmi, A. et al. Osteopontin and iCD8α cells promote intestinal intraepithelial lymphocyte homeostasis. J. Immunol. 204, 1968–1981 (2020).
Kristensen, M. F. et al. Osteopontin adsorption to Gram-positive cells reduces adhesion forces and attachment to surfaces under flow. J. Oral Microbiol. https://doi.org/10.1080/20002297.2017.1379826 (2017).
Schlafer, S., Meyer, R. L., Sutherland, D. S. & Städler, B. Effect of osteopontin on the initial adhesion of dental bacteria. J. Nat. Prod. https://doi.org/10.1021/np300514z (2012).
Kristensen, M. F., Sørensen, E. S., Del Rey, Y. C. & Schlafer, S. Prevention of initial bacterial attachment by osteopontin and other bioactive milk proteins. Biomedicines 10, 1922 (2022).
Funding
This material is based upon work supported by the National Science Foundation Graduate Research Fellowship under Grant No. 1937963 (to K.G.M.), as well as NIH grant R01DK111671 (to D.O-V.); Vanderbilt Training in Cellular, Biochemical and Molecular Sciences Training Program, T32GM008554-25 (to K.G.M.); and the Vanderbilt Institute for Clinical and Translational Research (VICTR) grant VR62082.
Author information
Authors and Affiliations
Contributions
K.G.M., J.R., and J.-H.W., conceived the project idea; J.-H.W. provided samples; K.G.M. performed data acquisition and analysis; K.G.M. and D.O.-V. wrote the manuscript; J.R., J.-H.W., K.G.M., and D.O.-V. revised and approved the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All samples were acquired from patients who had given informed consent for their samples to be used for research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McClanahan, K.G., Reese, J., Weitkamp, JH. et al. Effects of pasteurization on osteopontin concentrations in human breastmilk. Pediatr Res 95, 641–646 (2024). https://doi.org/10.1038/s41390-023-02838-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02838-1