Abstract
Background
The purpose of this study is to evaluate the association between SARS-CoV-2 viral load in respiratory secretions of infected children and signs/symptoms of COVID-19.
Methods
We reported the clinical characteristics of SARS-CoV-2-infected children during the study period. We compared viral load for several clinical variables, performed a predictive linear regression analysis to identify signs and symptoms significantly associated with viral load, and searched for discriminant viral load thresholds for symptomatic versus asymptomatic infections based on receiver-operating characteristics.
Results
A total of 570 patients were included. The median age was 4.75 years. Comparison of CT values by dichotomous variable showed higher viral loads in children with fever, respiratory symptoms, and previous exposure to SARS-CoV-2. The linear regression analysis confirmed a significant relationship between the CT value with these variables and with age, other symptoms, and asymptomaticity. In particular, infants with fever and SARS-CoV-2 exposure had higher viral loads. No viral load cut-offs were found to distinguish symptomatic from asymptomatic patients.
Conclusion
Our study shows that fever, SARS-CoV-2 exposure, and respiratory symptoms are associated with higher viral load in children, especially infants, while age, presence of nonrespiratory symptoms, or absence of any symptoms are associated with lower viral load.
Impact
-
Key message: the clinical variables that best predict viral load in infected children are history of previous exposure to a SARS-CoV-2-infected person and presence of fever and respiratory symptoms (higher viral load).
-
Added value to the current literature: this is the first article to prove this point.
-
Impact: SARS-CoV-2 viral load should not be used as a measure of clinical severity of COVID-19 in the pediatric population; however, lower viral load appears to be associated with asymptomatic COVID-19 in older children.
Similar content being viewed by others
Introduction
As of August 3, 2022, children accounted for 20.7% (8.7% in the 0–9 cohort and 12% in the 10–19 cohort) of the 21,243,890 confirmed cases of COVID-19 in Italy, according to the latest report from the Italian National Institute of Health.1 The clinical features of SARS-CoV-2 infection in children have been well described. The most recent systematic review and meta-analysis, including 37 studies on pediatric COVID-19, agrees with previous findings on the relatively mild course of the disease in younger children, with fever (48.5%) and cough (40.6%) as the most reported symptoms by 2874 children.2 In the absence of more specific signs and/or symptoms of pediatric COVID-19, previous exposure to a person infected with SARS-CoV-2 becomes a critical discriminator for the diagnosis of the disease in children.3 While we have learned much about the diagnosis and management of pediatric COVID-19, we know little about the relationship between clinical presentation and viral load of SARS-CoV-2 in children. Most studies have focused on the association between viral load and infectivity and/or age4,5 rather than symptom severity. However, it has recently been shown that viral load is significantly higher in adults with severe disease than in those with mild disease6 and that prolonged viral shedding with high viral load has been associated with adverse outcomes in hospitalized patients.7 This finding is interesting because no significant differences in SARS-CoV-2 nasopharyngeal viral loads were found between adults and children.8 Only one recent study evaluated the association between viral load, age, and symptom severity in children, showing no association between the three factors.9 However, this study did not focus on the relationship between SARS-CoV-2 viral load and the specific signs and symptoms of pediatric COVID-19.
Nucleic acid amplification tests, based on real-time reverse transcription polymerase chain reaction (RT-PCR), are the reference method for the diagnosis of acute SARS-CoV-2 infection.10 Cycle threshold (CT) levels obtained at the end of RT-PCR are inversely proportional to the amount of target nucleic acid in the sample and can be used as a proxy marker of viral quantification11 of the viral RNA load of SARS-CoV-2.12 WHO and CDC reports have shown comparable sensitivity among different target genes13,14 and a national study of more than 100 Korean laboratories showed overlapping results for CT values obtained from different RT-PCR assays.15 The determination of SARS-CoV-2 viral load is critical for the interpretation of laboratory tests and the management of isolation and contact tracing protocols.16 Attempts are being made to use the value of CT to understand the association between viral load and disease severity or to predict the evolution of SARS-CoV-2 infection. Indeed, studies based on clinical outcomes have shown that higher SARS-CoV-2 viral load is associated with higher mortality17,18 and increased risk of intubation in COVID-19 patients.19 Recently, it has been shown that low viral load (CT > 35) is not substantially associated with ongoing virus replication.13,20 Despite these findings, the clinical association with high or low viral load is still debated. A study involving 5830 patients with COVID-19 determined that the viral load of symptomatic and asymptomatic patients was not significantly different.21 On the other hand, some studies have shown that CT levels are a robust predictor of mortality rates among patients after the initial diagnosis of SARS-CoV-2 infection.22,23,24 In a retrospective study of 461 adult patients hospitalized with COVID-19, a 4.5-fold increase in the odds of death was reported for patients with a high SARS-CoV-2 viral load.24 However, no study has yet evaluated the clinical association of different SARS-CoV-2 viral loads in the pediatric population.
The purpose of this study is to evaluate the association between SARS-CoV-2 viral load in respiratory secretions of infected children and the specific signs and symptoms of pediatric COVID-19.
Materials and methods
Study design and setting
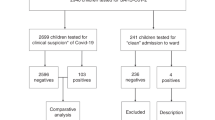
We retrospectively reviewed the cases of all children with a positive nasopharyngeal swab (NPS) for SARS-CoV-2 who were admitted to the emergency department (ED) of the Bambino Gesù Children’s Hospital, Research and Healthcare Institute, Rome, Italy, between May 2020 and April 2021. The ED provides free 24/7 urgent medical care. During the study period, there were 40,431 visits to the ER, 7487 of which resulted in admission to a ward. Patients were tested for SARS-CoV-2 whenever they presented with fever or any respiratory symptoms, including cough, shortness of breath, and rhinorrhea. All patients tested by procedure before scheduled admission to the ward were also included. These patients, although not triaged, were still admitted to the ED and tested for SARS-CoV-2 before admission to any ward. For each patient included, the clinical characteristics at the time of admission to the ED and the SARS-CoV-2 viral load detected by one of the molecular tests in use at our laboratory were reported.
Patients were grouped and compared by age (<1 year, ≥1 and <6 years, ≥6 and <10 years, ≥10 years). For each patient, the following variables were collected: age; sex; coexisting conditions; history of previous exposure to SARS-CoV-2; fever (defined as the temperature above 37.8 °C); respiratory symptoms, i.e., cough, shortness of breath, and rhinorrhea; other symptoms, i.e., vomiting, diarrhea, abdominal pain, rushing, asthenia and inappetence, conjunctivitis and, in patients aged 6 years and older, headache, chest pain, anosmia and ageusia; and admission to the ward. Fever and other signs and symptoms were recorded if the child presented them at the time of admission or if the parents reported them up to 48 h before admission to the ED. History of exposure to SARS-CoV-2-infected individuals was recorded only in case of direct contact. More specifically, all patients and/or their parents were asked whether they had had contact with someone in the household or someone with whom they spent a lot of time in close contact who was later found to be infected with SARS-CoV-2. Both comorbidities and other pathological conditions (such as a history of wheezing or recurrent infections) were included in the term “coexisting conditions.” Vaccination status was not recovered because the children were not yet vaccinated at the time of the study period. All variables in the four age groups were compared with the χ2 test.
Median CT values of patients divided dichotomously according to clinically relevant variables were reported and compared. Adopting the CT value as a continuous dependent variable, a linear regression analysis of significant variables was performed to identify the signs and symptoms most associated with SARS-CoV-2 viral load, at all ages and by age group. Finally, we looked for the threshold value of CT for each of the following criteria: fever; respiratory symptoms; fever and respiratory symptoms; and absence of fever and respiratory symptoms, considering patients as a set of groups and grouped into age groups.
SARS-CoV-2 assays
NPSs were collected in 3 mL of the universal transport medium (Copan Italia, Brescia, Italy) and analyzed for molecular detection of SARS-CoV-2. Samples from patients with acute conditions whose results were needed in less than 1 h were considered “urgent” (U) and analyzed with Cepheid GeneXpert Xpress SARS-CoV-2 (Cepheid, Sunnyvale, CA); samples from patients who needed a result within 2–5 h were considered “priority” (P) and analyzed with the Simplexa Covid-19 direct assay on LIAISON® MDX (DiaSorin Molecular, CA); samples from patients whose result was expected within 12 h were considered “standard” (S) and analyzed with the AllplexTM SARS-CoV2 assay (Seegene, Seoul, South Korea).
For the Cepheid GeneXpert Xpress SARS-CoV-2 assay, 300 µL of the sample was transferred into the cartridge and loaded into the GeneXpert Instrument System platform. The target genes are E and N. For Simplexa Covid-19 direct assay, 50 µL of the sample and 50 µL of the reaction mixture were transferred to the Direct Amplification Disc and loaded into the LIAISON® MDX. The target genes are S and ORF1ab. For the Seegene Starlet-Tanbead platform, a total of 300 µL per sample was extracted and eluted with 80 µL of elution buffer. RT-PCR was performed on CFX96 (Bio-Rad Laboratories) with AllplexTM SARS-CoV-2 Assay. For detection, 5 µL of extracted RNA was used in a final volume of 20 µL. Results were analyzed automatically using Seegene software (Seegene SARS-CoV-2 Viewer). The target genes are E, RdRp/S, and N.
An internal control was included in each reaction to check for PCR inhibition. Samples were considered positive when one or more genes were detected. For each sample, the average CT was calculated based on the genes detected.
Statistical analysis
All continuous variables were compared by the Kruskal–Wallis test, since they were mostly non-normally distributed. All categorical variables were compared by the χ2 test or Fisher’s exact test. A p value less than 0.05 was considered statistically significant. When multiple comparisons were performed, a Bonferroni-corrected p value was provided. A linear regression of the relevant variables of the univariate analysis was performed to identify the signs and symptoms most associated with molecular detection of SARS-CoV-2, adopting the CT value as a continuous dependent variable. CT value cut-offs for different combinations of signs and symptoms were derived by receiver-operating characteristic (ROC) curve analysis. All analyses were conducted using IBM SPSS statistical software, version 23.0.
Ethical approval
The study was approved by the local Ethics Committee. Informed consent from the participants’ legal guardian or next of kin was obtained at the time of admission to the pediatric emergency room.
Results
The study included 570 patients admitted to the ED of our hospital and tested positive for SARS-CoV-2 RNA detection. According to clinical conditions, three different molecular workflows were appropriately set up: 262 were tested as “U”, 90 as “P” and 218 as “S”.
Their clinical characteristics are shown in Table 1.
The median age of the subjects was 4.75 years (IQR 1.06–11.32), with most patients aged ≥1 and <6 years. Overall, 308 (54%) were males and 262 (46%) were females, with a female-to-male ratio of 1:1.2. Among pediatric patients admitted to the emergency room, 246/570 (43.2%) had a proven history of previous exposure to a SARS-CoV-2-infected person. A total of 244/570 (42.8%) patients were febrile on admission, 187/570 (32.8%) patients had respiratory symptoms, including cough, shortness of breath, or rhinorrhea. In our population, 238/570 (41.8%) had no fever or respiratory symptoms) and 178/570 (31.2%) patients had mostly other symptoms, among which vomiting and diarrhea were the most frequent. Among the 570 patients, 144 (25.3%) were completely asymptomatic. Of all patients, 153/570 (26.8%) required admission to the ward.
The clinical characteristics of the patients, grouped by age and compared with the χ2 test, are shown in Table 2.
Children younger than 1 year old (136/570) were significantly more febrile (80/136, 58.8%; p < 0.001) and had more respiratory symptoms (61/136, 44.9%; p < 0.001), especially cough (41/136, 30.1%; p < 0.001) and rhinorrhea (32/136, 23.5%; p < 0.001) than the other subgroups. Children aged ≥1 and <6 years (190/570) had no significant clinical features. Children aged 6–10 years (75/570) were mostly free of fever and respiratory symptoms compared with the other age groups (48/75, 64.0%; p < 0.001), and among other symptoms, abdominal pain was most frequently reported (12/75, 16.0%; p < 0.001). Finally, children aged ≥10 years (169/570) presented more often with headache (19/169, 11.2%; p < 0.001) and coexisting conditions (39/169, 23.1%; p < 0.001).
Comparison of CT values of 10 validation samples on the three platforms showed a slight statistically significant difference (p = 0.023), with a maximum variation between mean CT values of 1.2 (Supplementary Table 1). Considering this variation was not clinically significant, the results of the three assays were analyzed together.
The median CT values of patients according to clinically relevant dichotomous variables in the whole sample and by age group are shown and compared with the Kruskal–Wallis test in Tables 3 and 4.
When analyzing the entire population, all signs and symptoms considered were found to be significantly associated with the change in CT value. Fever, respiratory symptoms, and previous exposure to an individual infected with SARS-CoV-2 were all associated with a lower CT value (with a median CT of about 20). Specifically, children with fever and/or respiratory symptoms showed a median CT of about 20 (fever 20.6, IQR 15.6–33.3; respiratory symptoms 20.2, IQR 16.1–28.4) compared with 34.2 (IQR 23.3–40.3) for asymptomatic patients. This difference in CT values was not evident in all age groups. In more detail: fever was significantly associated with a lower CT value at all ages except in children aged 1–6 years (15.9, 20.2, and 24.2 compared with 20.7, 34.9, and 33.9, in the <1 year, 6–10 years, and >10 years groups, p = 0.005, 0.005, and <0.001, respectively); respiratory symptoms and previous exposure to an individual infected with SARS-CoV-2 were significantly associated with a lower CT value in patients aged 1–6 years and >10 years (respiratory symptoms 25.6 and 21.8 compared with 33.1 and 33.9, p = 0.001 and <0.001, respectively; exposure to SARS-CoV-2 25.4 and 23.3 compared with 34.4 and 32.3, p < 0.001 and <0.001, respectively).
A linear regression analysis was conducted, adopting the CT value as the dependent variable and the clinically or statistically significant variables from the univariate analysis as the independent variables. Ward admission, although found to be slightly significant in previous analyses, was excluded from the regression model because it would be considered a clinical outcome, rather than a clinical predictor, of higher viral load. In addition, in many cases, patients were admitted on the basis of significant comorbidity rather than on the basis of COVID-19 infection alone. The results of linear regression analysis in the whole study sample and for each age group are shown in Tables 5 and 6, respectively.
This analysis confirms that previous exposure to SARS-CoV-2-infected individuals, fever and respiratory symptoms, predicted a lower CT value (corresponding to a higher viral load), while older age, absence of fever and respiratory symptoms, and presence of other symptoms, predicted a higher CT value (corresponding to a lower viral load).
When stratified by age, only exposure history remained a parameter significantly associated with a lower CT value in all age groups except the 1- to 6-year-old group.
Using ROC curve analysis, we explored the cut-offs of the CT value for each of the following criteria: fever; respiratory symptoms; fever and respiratory symptoms; and absence of fever and respiratory symptoms. However, the ROC curves did not produce a reliable shape and area under the curve to define valid cut-offs (data not shown). Therefore, clinically meaningful cut-offs for the CT value could not be produced.
Discussion
Our study sought to associate the signs and symptoms of pediatric COVID-19 with the viral load of SARS-CoV-2 in the respiratory secretions of positive children accessing our ED. Samples were obtained using a NPS and measured by RT-PCR, the gold standard diagnostic test for the detection of SARS-CoV-2. In addition to its high sensitivity, the molecular test generates the CT, a proxy for viral load, which is particularly useful in defining the infectivity of positive patients.13 Although no clinical study has validated the use of CT values to define patient management,25 many efforts are aimed at defining a putative association between CT values and clinical setting.26
The clinical and demographic features of our study are comparable to those reported in the literature,27 with fever and respiratory symptoms dominating the presentation of symptomatic COVID-19 in children and with other nonrespiratory symptoms, such as vomiting, diarrhea, abdominal pain, and headache, accounting for less than 10% of all cases. Slightly less than half of the pediatric COVID-19 cases remain asymptomatic, consistent with the hypothesis of a milder course of the disease in children. Most studies on pediatric COVID-19 have focused on the pediatric population as a whole, without distinguishing between age groups.28,29 In this study, we divided patients according to age to see if age groups could be related to specific manifestations of COVID-19. Indeed, we found significant differences between the age groups in terms of clinical presentation (as shown in Table 2). More specifically, younger children (<6 years) appeared to be more febrile and presented with more cough than older children (>6 years), who in turn presented with more comorbidities and “atypical” nonrespiratory symptoms. The reason for this may be twofold: either the symptoms were more likely to be described by older and more “self-conscious” patients than by younger patients, or the reported symptoms were related to another illness, so the finding of SARS-CoV-2 was only occasional, as the later evidence of low viral load observed in this group seems to suggest.
Comparing the median CT value of the patients according to the single dichotomous variable considered (as shown in Tables 3 and 4), we found significant differences at all ages, suggesting that the presence or absence of specific signs and symptoms, as well as previous exposure to a SARS-CoV-2-infected person, may drive viral load. In more detail, patients with fever and/or respiratory symptoms showed a lower CT value than both patients negative for these parameters (CT ~20 vs. CT ~32; p < 0.001) and asymptomatic patients (CT ~34 vs. CT ~23, p < 0.001). Children younger than 1 year were more febrile than the other age subgroups, and their CT value (CT ~16) was also the lowest among all subgroups. A history of previous exposure to an individual infected with SARS-CoV-2 was also associated with a lower CT value (CT ~22 vs. CT ~34, p < 0.001). The reasons explaining this phenomenon may be related to Italian health policy, which allows easier and free access to treatment, or to an increased awareness of parents, who bring their children to the emergency room in the first phase of the disease, when the viral load is highest. In fact, Yonker et al. showed that children have a higher viral load in the first 5 days of illness.8 Of note, fever, respiratory symptoms, and previous exposure to SARS-CoV-2 were all associated with a lower CT value in children older than 10 years. Overall, patients with coexisting conditions were associated with a higher CT value (CT ~35 vs. CT ~24; p value < 0.001). This could be due to the occasional finding of SARS-CoV-2 positivity in patients who accessed the ED for other reasons or required hospitalization for which SARS-CoV-2 testing is performed as part of the admission protocol.
In the linear regression model (as shown in Tables 5 and 6), advanced age, absence of fever and respiratory symptoms, and presence of other symptoms were negatively associated with viral load; while temperature, respiratory symptoms, and exposure to SARS-CoV-2 were positively associated with it. All these results were significant. In age-specific linear regression analysis, exposure to SARS-CoV-2 was significantly associated with elevated viral load at all ages except in the 1- to 6-year-old group. In children younger than 1 year, fever was the best predictor of higher viral load.
These results strongly suggest that the lack of overt symptomatology in children may be associated with a lower SARS-CoV-2 viral load; in fact, completely asymptomatic patients, especially older ones, show lower CT values. Unfortunately, our analysis did not allow us to define stringent cut-offs for CT values associated with specific signs and symptoms.
The single-center retrospective design of our study prevents us from generalizing our hypotheses to the entire pediatric population. In addition, we did not include a comparison of clinical variables according to the type of test used to determine the CT value. However, validation of CT values among the platforms demonstrated a very low difference between the three, with a maximum mean difference of 1.2, despite a significant p value (p = 0.023), which we considered not clinically significant. The concordance between molecular tests for SARS-CoV-2 is further supported by a recent study by Raju et al. in which strong linearity in CT values is reported between different platforms, including the GeneXpert and Simplexa tests, two of the three tests used in this study.30 Another limitation of this study is that we could not consider the new SARS-CoV-2 variants of interest (VOC), which are currently emerging and could change the pediatric scenario of VOCID-19. During the study period, SARS-CoV-2 wild-type, followed by the UK variant (VOC 202012/01) since approximately February 2021, has been the most prevalent viral strain, while the omicron variant currently accounts for 99.8% of all new cases of COVID-19 in Italy.31
Conclusion
Our study is the first to address the association between SARS-CoV-2 viral load and clinical manifestations of COVID-19 in different pediatric ages. We found that a higher viral load was often associated with fever, SARS-CoV-2 exposure, and respiratory symptoms in children, especially infants, while age, the presence of nonrespiratory symptoms, or the absence of any symptoms were associated with a lower viral load. On the other hand, a lower viral load may be associated with the complete absence of fever and respiratory symptoms in older children. Thus, while a higher viral load may be associated with fever, respiratory symptoms, and recent infection, the lack of the latter is usually indicative of a lower viral load. Further studies are needed to demonstrate the association between SARS-CoV-2 viral load, infectivity, and clinical severity of pediatric COVID-19.
Data availability
The datasets generated and/or analyzed during this study are available from the corresponding author upon reasonable request.
References
Italian National Health Institute (Istituto Superiore di Sanità). Coronavirus epidemic: situation report. https://www.epicentro.iss.it/coronavirus/bollettino/Bolletino-sorveglianza-integrata-COVID-19_3-agosto-2022.pdf.
Qi, K. et al. Clinical, laboratory, and imaging features of pediatric COVID-19: a systematic review and meta-analysis. Medicine (Baltimore) 100, e25230 (2021).
Roversi, M. et al. Diagnosis of COVID-19 in children guided by lack of fever and exposure to SARS-CoV-2. Pediatr. Res. 11, 1–7 (2021).
Yu, F. et al. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin. Infect. Dis. 71, 793–798 (2020).
Baggio, S. et al. Severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) viral load in the upper respiratory tract of children and adults with early acute coronavirus disease 2019 (COVID-19). Clin. Infect. Dis. 73, 148–150 (2021).
Amy, E. et al. SARS-CoV-2 viral load peaks prior to symptom onset: a systematic review and individual-pooled analysis of coronavirus viral load from 66 studies. Preprint at https://www.medrxiv.org/content/10.1101/2020.09.28.20202028v1 (2020).
Néant, N. et al. Modeling SARS-CoV-2 viral kinetics and association with mortality in hospitalized patients from the French COVID cohort. Proc. Natl Acad. Sci. USA. 118, e2017962118 (2021).
Yonker, L. M. et al. Virologic features of severe acute respiratory syndrome coronavirus 2 infection in children. J. Infect. Dis. 224, 1821–1829 (2021).
Madera, S. et al. Nasopharyngeal SARS-CoV-2 viral loads in young children do not differ significantly from those in older children and adults. Sci. Rep. 11, 3044 (2021).
Recommendations for national SARS-CoV-2 testing strategies and diagnostic capacities. Interim guidance. WHO. 25 June 2021. https://apps.who.int/iris/bitstream/handle/10665/342002/WHO-2019-nCoV-lab-testing-2021.1-eng.pdf?sequence=1&isAllowed=y.
Tom, M. R. & Mina, M. J. To interpret the SARS-CoV-2 test, consider the cycle threshold value. Clin. Infect. Dis. 71, 2252–2254 (2020).
Bullard, J. et al. Infectivity of severe acute respiratory syndrome coronavirus 2 in children compared with adults. CMAJ 193, E601–E606 (2021).
Piralla, A. et al. Residual SARS-CoV-2 RNA in nasal swabs of convalescent COVID-19 patients: is prolonged quarantine always justified? Int. J. Infect. Dis. 102, 299–302 (2021).
Corman, V. M. et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eur. Surveill. 25, 2000045 (2020).
Sung, H. et al. Nationwide external quality assessment of SARS-CoV-2 molecular testing, South Korea. Emerg. Infect. Dis. 26, 2353–2360 (2020).
Dahdouh, E., Lázaro-Perona, F., Romero-Gómez, M. P., Mingorance, J. & García-Rodriguez, J. Ct values from SARS-CoV-2 diagnostic PCR assays should not be used as direct estimates of viral load. J. Infect. 82, 414–451 (2021).
Faíco-Filho, K. S., Passarelli, V. C. & Bellei, N. Is higher viral load in SARS-CoV-2 associated with death? Am. J. Trop. Med. Hyg. 103, 2019–2021 (2020).
Huang, J. T. et al. Chronological changes of viral shedding in adult inpatients with COVID-19 in Wuhan, China. Clin. Infect. Dis. 71, 2158–2166 (2020).
Magleby, R. et al. Impact of SARS-CoV-2 viral load on risk of intubation and mortality among hospitalized patients with coronavirus disease 2019. Clin. Infect. Dis. 73, e4197–e4205 (2020).
Rhee, C., Kanjilal, S., Baker, M. & Klompas, M. Duration of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infectivity: when is it safe to discontinue isolation? Clin. Infect. Dis. 72, 1467–1474 (2021).
Miller, E. H. et al. Pretest symptom duration and cycle threshold values for severe acute respiratory syndrome Coronavirus 2 reverse-transcription polymerase chain reaction predict coronavirus disease 2019 mortality. Open Forum Infect. Dis. 8, ofab003 (2021).
Silva Júnior, J. V. J. et al. End-point RT-PCR: a potential alternative for diagnosing coronavirus disease 2019 (COVID-19). J. Virol. Methods 288, 114007 (2021).
Rabaan, A. A. et al. Viral dynamics and real-time RT-PCR Ct values correlation with disease severity in COVID-19. Diagnostics (Basel) 11, 1091 (2021).
El Zein, S. et al. SARS-CoV-2 infection: initial viral load (iVL) predicts severity of illness/outcome, and declining trend of iVL in hospitalized patients corresponds with slowing of the pandemic. PLoS One 16, e0255981 (2021).
Quiroga, S. A. et al. Contrasting SARS-CoV-2 RNA copies and clinical symptoms in a large cohort of Colombian patients during the first wave of the COVID-19 pandemic. Ann. Clin. Microbiol. Antimicrob. 20, 39 (2021).
Lennon, N. J. et al. LB-11. Comparison of viral loads in individuals with or without symptoms at time of COVID-19 testing among 32,480 residents and staff of nursing homes and assisted living facilities in Massachusetts. Open. Forum Infect. Dis. 7, S848–S849, https://clinicaltrialsgov/show/NCT02750826 (2020).
Borrelli, M., Corcione, A., Castellano, F., Fiori Nastro, F. & Santamaria, F. Coronavirus disease 2019 in children. Front. Pediatr. 9, 668484 (2021).
Christakis, D. A. Pediatrics and COVID-19. JAMA 324, 1147–1148 (2020).
Ludvigsson, J. F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 109, 1088–1095 (2020).
Raju, S. et al. Comparison of 6 SARS-CoV-2 molecular methods and correlation with the cycle threshold distribution in clinical specimens. J. Appl. Lab. Med. 6, 1452–1462 (2021).
Italian National Health Institute (Istituto Superiore di Sanità). Monitoraggio delle varianti del virus SARS-CoV-2 di interesse in sanità pubblica in Italia. https://www.epicentro.iss.it/coronavirus/pdf/sars-cov-2-monitoraggio-varianti-rapporti-periodici-25-giugno-2021.pdf.
Author information
Authors and Affiliations
Contributions
Conceptualized and designed the article: M.R., L.C., L.Pi., U.R. Collected data: L.C., L.Pi., A.T., L.Pa., C.O. Analyzed the data: M.R. Verified the underlying data and statistical analysis: M.R., U.R. Drafted and wrote the first manuscript and tables: M.R., L.C., L.Pi. Provided laboratory expertise and contributed to acquisition, analysis, and interpretation of data: L.C., L.Pi. Revised the manuscript for important intellectual content: U.R., A.R., C.F.P., A.V., C.R. Reviewed and accepted the final manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The work was approved by our Ethics Committee. Patient consent was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Roversi, M., Coltella, L., Piccioni, L. et al. Relationship between viral load and symptoms in children infected with SARS-CoV-2. Pediatr Res 93, 897–904 (2023). https://doi.org/10.1038/s41390-022-02293-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02293-4