Abstract
Objective
To describe renal regional saturation of oxygen (RrSO2) values during the first week of life for preterm neonates born at <32 weeks gestational age (GA).
Methods
RrSO2 values recorded over the first week of life using near-infrared spectroscopy were retrospectively analyzed in this two-center cohort study of preterm infants without known congenital anomalies of the kidney.
Results
A cohort of 109 neonates with a median GA of 26.9 weeks and a median of 120 (IQR: 87–141) hours of continuous RrSO2 monitoring were included. Separately fitted trends in RrSO2 did not differ (p = 0.52) between sites and demonstrated a consistent decrease in RrSO2 by 20 points (95% CI: 9.6–30.1) during the first 60 h of life, followed by a stabilization of RrSO2 thereafter. RrSO2 baseline trends increased by 2.1 (95% CI: 0.8–3.3) percentage points for each additional week GA between 24 and 32 weeks GA.
Conclusions
Despite differences in adjusted RrSO2 values between sites, profiles over time are consistent, allowing for the determination of RrSO2 trajectories in preterm infants. This expected pattern of RrSO2 changes in the first week may help guide future investigations and interventions to identify and reduce kidney injury in the preterm neonate.
Impact
-
Renal regional saturation of oxygen (RrSO2) slowly decreases during the first 60 h of age in <32-week preterm neonates.
-
While site differences were identified with respect to absolute values, RrSO2 trends from two different centers were not different.
-
Lower gestational age neonates have lower RrSO2 levels during the first week.
Similar content being viewed by others
Introduction
Premature birth continues to be a major public health problem with one in ten babies born <37 weeks. Long-term studies of 40- to 50-year-old adults born prematurely show two to three times increased risk of chronic kidney disease (CKD1). The etiology of this increased risk is multifactorial, but likely begins at birth and in the Neonatal Intensive Care Unit (NICU2). Premature neonates have reduced nephron endowment, increased nephrotoxic medication exposures, and increased acute kidney injury (AKI) compared to term neonates3. Unfortunately, our monitoring of kidney function in the NICU is limited to tracking urine output, which is notoriously difficult, and utilizing frequent serum creatinine checks that requires relatively large blood sampling for premature neonates4. A method to monitor kidney health and function non-invasively that more effectively detects sudden changes and alterations is needed to protect the limited nephrons and reduce the long-term risk of CKD.
Somatic tissue oxygenation monitoring with near-infrared spectroscopy (NIRS) is increasingly being used in neonates to detect changes in physiology that could impact clinical outcomes5, including necrotizing enterocolitis6,7, diagnosis of a hemodynamically significant patent ductus arteriosus8, and neonatal encephalopathy9. Specifically, noninvasive measurement of renal regional saturation of oxygen (RrSO2) has been feasible in preterm neonates and values less than 50 have been associated with the subsequent development of AKI10,11. However, normal changes in RrSO2 in preterm neonates at different gestational ages (GAs) in the first week have not been well described outside of single-center studies12,13,14.
To address this gap, we sought to describe RrSO2 values during the first week of age for preterm neonates born at less than 32 weeks GA at two centers. We hypothesized that given rapidly changing kidney physiology and the wide range of renal development associated with varying preterm GAs4,15,16,17,18, RrSO2 would likely change significantly in the first week.
Methods
This two-center study was conducted using existing cohorts of preterm neonates admitted to the level III NICU at UnityPoint Health-Meriter Hospital (UPHM) (Madison, WI) and the level IV NICU at Lucile Packard Children’s Hospital Stanford (LPCH) (Palo Alto, CA) from 2016 to 2019. The data on subjects from UPHM were obtained from a blinded prospective study where all neonates <32 weeks GA, and with chronologic age <48 h at the time of enrollment were eligible for inclusion in the study. Exclusion criteria were infants with known congenital anomalies of the kidney, investigator unavailability to consent parent or clinician decision that NIRS monitoring was not suitable due to clinical condition. The data on subjects from LPCH were obtained from unblinded standard clinical monitoring in all neonates <29 weeks GA. Each center received approval from their institutional review board to participate in this study. The primary study aim was to assess trends in RrSO2 in the first week of life measured with continuous renal NIRS monitoring.
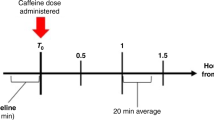
Both centers used the same technique for NIRS monitoring. A neonatal sensor connected to an INVOS 5100C NIRS monitor was placed on the infant’s right or left flank (to measure RrSO2). The sensor was placed directly over Mepitel transparent adhesive dressing to aid with skin protection. Clinicians and staff were blinded to the RrSO2 values at UPHM. At LPCH the values were visible but there were no guidelines for addressing RrSO2 values during the time period of the study. Sensors were kept in place until the infant was 7-days old (168 h of life (HOL)) and RrSO2 values were recorded every 5–30 s.
Patient and maternal demographics and perinatal details were obtained from the electronic medical record. RrSO2 data were subsequently processed to give hourly averages based on hours of life.
Statistical methods
Continuous demographic characteristics were summarized using means and standard deviations or medians and interquartile range; categorical features were described using frequencies and percentages. Distributions of continuous and categorical variables were compared between sites using χ2 tests, t-tests, non-parametric (rank-sum) procedures, or multivariable regression if the characteristic was thought to be jointly influenced by several factors. Hourly readings of RrSO2 over the first 168 HOL were analyzed using generalized estimating equations19,20 for a Gaussian family, probit link function, and with autoregressive correlation structure for repeated measures over time. HOL (2–168) entered the model as a six-knot restricted cubic spline to allow for linear and non-linear behavior. Other demographic features (e.g., sex, GA, birth weight, mode of delivery) were examined to see whether they had any influence on trends. Models utilized a robust “sandwich” estimator of variance for estimation and testing of relevant effects to guard against possible misspecification of the correlation structure. A p value <0.05 was considered significant. Trends were assessed separately across centers and compared.
Results
A total of 109 neonates (UPHM (n = 35, 32%) and LPCH (n = 74, 68%)) were included in the study. Demographic information for the full cohort and individual centers is listed in Table 1 along with comparisons between centers. Average GA for UPHM neonates was almost two weeks greater than those from LPCH (28.5 ± 2.43 vs. 26.5 ± 1.49, 95% CI: 1.07–2.86; p < 0.001), and this was associated with a 25% increase in median birth weight (95% CI: 9–44% increase; p = 0.001). Sex and method of delivery appeared roughly balanced between the two locations, with slightly more than half of neonates being male and just under two-thirds of births by Cesarean section delivery. There was no difference in birth weight once adjusted for GA, sex, and mode of delivery.
Recording of RrSO2 took place over the first 168 HOL with occasional interruptions or delayed starts. The earliest recordings began at 2 and 5 HOL for LPCH and UPHM, respectively, with 75% of neonates from each site starting no later than 14 (LPCH) or 44 (UPHM) HOL. In addition to starting earlier, LPCH monitoring tended to have longer uninterrupted blocks of continuous measurements (median [IQR] 122 [88–145] continuous hours) compared to UPHM (115 [80–124] continuous hours).
Mean percent RrSO2 for neonates at LPCH exhibited a non-linear relationship with time during the 168 HOL (χ24 = 11.7, p = 0.019) but with no strong association with GA (p = 0.065), sex (p = 0.93), or mode of delivery (p = 0.52). At UPHM, the pattern of mean percent RrSO2 over time showed evidence (χ24 = 17.0, p = 0.002) of non-linear behavior and a positive association involving GA (p = 0.034). Sex and mode of delivery were not strongly associated with trends in the mean response (p > 0.40 for each). Figure 1 demonstrates these patterns for LPCH (Fig. 1a) and UPHM (Fig. 1b). Apgar score at 5 min had no association (p = 0.856) with RrSO2 after adjusting for the other elements in the model (HOL, location, GA, mode of delivery and sex).
a, b— The solid lines represent the mean RrSO2 over time with pointwise 95% confidence limits for the mean at each HOL given by dashed lines; gray points are individual measurements from each neonate at the centers (a - Lucile Packard Children’s Hospital Stanford, b - UnityPoint Health-Meriter Hospital). Overall common behavior RrSO2 means (c)—each center represented with red (UnityPoint Health-Meriter Hospital) and black (Lucile Packard Children’s Hospital Stanford) with shaded regions representing the 95% confidence intervals for the mean RrSO2.
Trends (linear [one term] and non-linear [four components]) in percent RrSO2 did not statistically differ between locations (χ25 = 4.18, p = 0.524; test of center*trend interaction). Despite a strong difference between centers in absolute values (p = 0.001), the mean trend for LPCH consistently remained higher than UPHM by 6.6–15.5%, with the greatest separation occurring around 50 HOL (Fig. 1). Each center showed elevated initial RrSO2 values followed by a nadir reached at 60 HOL with a subsequent plateau in RrSO2 values for the remaining hours. Given the statistically similar trends in RrSO2 values between centers, the absolute expected change in percent RrSO2 at various time points were determined (Fig. 2). The change in percent RrSO2 is expected to be slightly less than 5 points in the first 2–12 HOL and 5 points from 12 to 24 HOL, with decreased changes in percent RrSO2 in subsequent time intervals until reaching no change around 72 HOL, which corresponds with the plateau period previously described. The cumulative reduction of RrSO2 from 2 to 60 HOL is 20 percentage points (95% CI: 9.6–30.1; p = 0.05).
Stratification of RrSO2 trends by GA after controlling for center, sex and mode of delivery is shown in Fig. 3. We found that the baseline RrSO2 trend curve increases 2.1 percentage points (95% CI: 0.8–3.3; p = 0.001) for each additional week of gestation between 24 and 32 weeks.
Discussion
In this two-center cohort study evaluating RrSO2 trends over the first 7 days in <32-week preterm infants, we found that absolute RrSO2 decreased by 20 points in the first 60 h of age followed by a plateau for the remaining days in the first week. Despite absolute center differences, both center cohorts followed a similar decreasing RrSO2 trend after birth. After controlling for site, sex, and delivery method, we found that the RrSO2 baseline increased by 2.1 percentage points for each additional week of gestation between 24 and 32 weeks.
The overall decrease in RrSO2 seen in the first 60 HOL for these infants may be explained by expected physiologic changes in the kidney after birth. Typically, in utero kidney blood flow accounts for 3–5% of cardiac output and after birth, and increases to 10% in the first week and about 20% of cardiac output as adults21. The increase in tissue oxygenation due to the increased blood flow is likely offset and overcome by the increase in oxygen extraction due to a rapid increase in glomerular filtration rate (GFR) and increase in aerobic metabolism driven by an increase in ATP-dependent pumps21. It is likely that this increase in GFR results in increased oxygen utilization and explains the down-trending RrSO2 seen in the first 60 h and this finding could be confirmed in future studies by also evaluating the fractional tissue oxygen extraction, or FTOE. The difference in oxygenation seen in the most premature neonates may be explained by decreased vascularization of the kidney, subsequently reducing oxygenation compared to less premature neonates with more advanced kidney development and vascularization. An additional factor likely to contribute to changes seen in our study is the effect of cardiac blood flow and specifically hemodynamically significant patent ductus arteriosus’ that have been noted to affect renal tissue oxygenation in other studies8,22. In this study, we could not assess this effect as each center typically does not obtain echocardiograms until after seven days of age. While not assessed with this data, future studies could evaluate the relationship between RrSO2 and the development of AKI in premature infants so that variation from our described trends could aid with AKI treatment and prevention.
In comparison to previous neonatal renal NIRS monitoring studies, our data has the advantage of prolonged continuous monitoring until day seven at two different sites that used similar techniques. A previous preterm study by Richter et al. intermittently evaluated RrSO2 in the first 48 h after birth in 25–29-week GA infants and found a median range of 63–72% but an IQR of 48–87% suggestive of significant variability23. It is difficult to compare our data as many of our neonates started monitoring at 24 h but the range of values is similar between 24 and 48 h. Most recently, in a study of neonates <30 weeks, similar to our findings RrSO2 declined significantly in the first 96 h and absolute values were within the range seen in our two centers14. In another study, McNeill et al. monitored a smaller cohort of older preterm neonates (29–33 weeks GA) from days 3–21 and found a slow decrease in renal tissue oxygenation12. This is different from the stable trend we observed from 60 h to 7 days of age, but our patients were of lower GA. A small cohort of preterm infants limited to a single center has also been described by Marin et al.13 and again demonstrated similar trends over time and with GA as we have reported here. Additional studies evaluating RrSO2 in term infants24,25 describe a comparable trajectory with initial peak values of RrSO2 that then nadir, although the peak RrSO2 is higher in term infants than in preterm cohorts.
Although trends in RrSO2 were not statistically different between the two centers, there were absolute differences that persisted, despite controlling for differences in GA and birth weight. This could be due to differences in blinding between centers that could have influenced clinicians’ decisions to make clinical changes such as giving fluid boluses or blood transfusions despite neither center having a management guideline based on RrSO2 values. Similarly, each center has different protocols for blood transfusions, fluid management, and other clinical needs, which without being standardized across the two centers, could influence RrSO2 and is not possible to control for. Each center also has different thresholds for SpO2 alarms (LPCH alarms at 88 and 100%; UPHM alarms at 88 and 95%). It is known that SpO2 correlates with RrSO226; thus, the use of additional FiO2 to potentially maintain a higher SpO2 for infants at one center could have influenced the RrSO2 trend. Finally, LPCH uses renal NIRS monitoring as the standard of care while the other center required obtaining consent prior to use—this difference led to fewer early time points for neonates at UPHM and may have fundamentally altered the UPHM cohort as parents who consented to the study may have had fewer sick neonates.
This study is limited by the retrospective nature and reliance on chart review for data and outcome documentation. All variables could not be controlled for and likely influenced the persistent center differences. Changes in hemoglobin levels, timing of red blood cell transfusions, blood pressure, and SpO2 were also not acquired, limiting the ability to evaluate the effects of anemia, hypotension, and hypoxemia on RrSO2 absolute values and trends. Renal fractional oxygen extraction was also not obtained. This information may confirm if changes over time and with GA are related to a relative redistribution of renal perfusion or to alterations in oxygen utilization by a maturing kidney.
Conclusions
In conclusion, this study contributes the largest number of preterm neonates with continuously monitored RrSO2 over the first week of age. Although absolute differences in values existed between sites, the overall RrSO2 trend was similar and initially decreased after birth, before plateauing at about 60 h of age. Future large, multicenter studies should be conducted to better evaluate center differences and confirm true normative values. Multicenter studies would also be appropriate to assess the relationship between trends in RrSO2 and the development of AKI. Future critical studies are needed to evaluate whether RrSO2 changes can predict AKI prior to changes in serum creatinine and urine output, and to evaluate protocols for interventions. The normative data from this study can be used to inform current clinical care as well as future studies to assess variation from the normal values, as well as clinical outcomes, with a goal to shape clinical management guidelines for AKI detection and treatment based on renal tissue oxygenation.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Crump, C., Sundquist, J., Winkleby, M. A. & Sundquist, K. Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: national cohort study. BMJ 365, l1346 (2019).
Low Birth Weight and Nephron Number Working Group. The impact of kidney development on the life course: a consensus document for action. Nephron 136, 3–49 (2017).
Harer, M. W., Charlton, J. R., Tipple, T. E. & Reidy, K. J. Preterm birth and neonatal acute kidney injury: implications on adolescent and adult outcomes. J. Perinatol. 40, 1286–1295 (2020).
Selewski, D. T. et al. Neonatal acute kidney injury. Pediatrics 136, e463–e473 (2015).
Hyttel-Sorensen, S. et al. Cerebral near infrared spectroscopy oximetry in extremely preterm infants: phase II randomised clinical trial. BMJ 350, g7635 (2015).
Martini, S. & Corvaglia, L. Splanchnic NIRS monitoring in neonatal care: rationale, current applications and future perspectives. J. Perinatol. 38, 431–443 (2018).
Baserga, M., Reich, B. & Braski, K. Abnormal splanchnic regional saturations in a preterm infant that developed necrotizing enterocolitis following a red blood cell transfusion. Adv. Neonatal Care 20, 401–405 (2020).
Chock, V. Y., Rose, L. A., Mante, J. V. & Punn, R. Near-infrared spectroscopy for detection of a significant patent ductus arteriosus. Pediatr. Res. 80, 675–680 (2016).
Chock, V. Y., Frymoyer, A., Yeh, C. G. & Van Meurs, K. P. Renal saturation and acute kidney injury in neonates with hypoxic ischemic encephalopathy undergoing therapeutic hypothermia. J. Pediatr. 200, 232–239.e231 (2018).
Bonsante, F. et al. Low renal oxygen saturation at near-infrared spectroscopy on the first day of life is associated with developing acute kidney injury in very preterm infants. Neonatology 115, 198–204 (2019).
Harer, M. W., Adegboro, C. O., Richard, L. J. & McAdams, R. M. Non-invasive continuous renal tissue oxygenation monitoring to identify preterm neonates at risk for acute kidney injury. Pediatr. Nephrol. 36, 1617–1625 (2021).
McNeill, S., Gatenby, J. C., McElroy, S. & Engelhardt, B. Normal cerebral, renal and abdominal regional oxygen saturations using near-infrared spectroscopy in preterm infants. J. Perinatol. 31, 51–57 (2011).
Marin, T. et al. Renal oxygenation (RsO2) population parameter estimates in premature infants routinely monitored with near-infrared spectroscopy. Adv. Neonatal. Care (2021). Online ahead of print.
Hoffman, S. B., Magder, L. S. & Viscardi, R. M. Renal versus cerebral saturation trajectories: the perinatal transition in preterm neonates. Pediatr. Res. (2022). Online ahead of print.
Bueva, A. & Guignard, J. P. Renal function in preterm neonates. Pediatr. Res. 36, 572–577 (1994).
Charlton, J. R., Baldelomar, E. J., Hyatt, D. M. & Bennett, K. M. Nephron number and its determinants: a 2020 update. Pediatr. Nephrol. 36, 797–807 (2021).
Chikkannaiah, P., Roy, M., Kangle, R. & Patil, P. V. Glomerulogenesis: can it predict the gestational age? A study of 176 fetuses. Indian J. Pathol. Microbiol. 55, 303–307 (2012).
Hinchliffe, S. A., Sargent, P. H., Howard, C. V., Chan, Y. F. & van Velzen, D. Human intrauterine renal growth expressed in absolute number of glomeruli assessed by the disector method and cavalieri principle. Lab. Invest. 64, 777–784 (1991).
Hardin, J. W. & Hilbe, J. M. Generalized Estimating Equations (Chapman & Hall/CRC, 2003).
Zeger, S. L., Liang, K. Y. & Albert, P. S. Models for longitudinal data: a generalized estimating equation approach. Biometrics 44, 1049–1060 (1988).
Nada, A., Bonachea, E. M. & Askenazi, D. J. Acute kidney injury in the fetus and neonate. Semin. Fetal Neonatal. Med. 22, 90–97 (2017).
van der Laan, M. E. et al. A hemodynamically significant patent ductus arteriosus does not affect cerebral or renal tissue oxygenation in preterm infants. Neonatology 110, 141–147 (2016).
Richter, A. E. et al. The effect of maternal antihypertensive drugs on the cerebral, renal and splanchnic tissue oxygen extraction of preterm neonates. Neonatology 110, 163–171 (2016).
Bailey, S. M., Hendricks-Munoz, K. D. & Mally, P. Cerebral, renal, and splanchnic tissue oxygen saturation values in healthy term newborns. Am. J. Perinatol. 31, 339–344 (2014).
Montaldo, P., De Leonibus, C., Giordano, L., De Vivo, M. & Giliberti, P. Cerebral, renal and mesenteric regional oxygen saturation of term infants during transition. J. Pediatr. Surg. 50, 1273–1277 (2015).
Petrova, A. & Mehta, R. Regional tissue oxygenation in association with duration of hypoxaemia and haemodynamic variability in preterm neonates. Arch. Dis. Child Fetal Neonatal. Ed. 95, F213–F219 (2010).
Acknowledgements
We would like to thank the Meriter Foundation for funding the initial trial at UPHM. We would like to thank the families for agreeing to participate in the study.
Author information
Authors and Affiliations
Contributions
M.W.H.: significant contributions to the design and conception, data analysis and interpretation, drafting the manuscript, critical revision of the manuscript and final approval. P.E.C.: analysis and interpretation of data; drafting the article and revising it critically for important intellectual content; and final approval of the version to be published. J.E.C.: collection and interpretation of data; and final approval of the version to be published. M.R.L.: analysis of data and drafting methods/parts of results and review/approval of manuscript. V.Y.C.: significant contributions to the design and conception, data analysis and interpretation, drafting the manuscript, critical revision of the manuscript and final approval.
Corresponding author
Ethics declarations
Competing interests
The authors have no financial disclosures. V.Y.C. is supported by the Stanford Maternal and Child Health Research Institute. M.W.H. is supported by the Wisconsin Partnership Program New Investigator Award and an institutional KL2 award (KL2TR002374).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Harer, M.W., Condit, P.E., Chuck, J.E. et al. Renal oxygenation measured by near-infrared spectroscopy in preterm neonates in the first week. Pediatr Res 92, 1744–1748 (2022). https://doi.org/10.1038/s41390-022-02036-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02036-5
This article is cited by
-
Renal tissue oxygenation and development of AKI in preterm neonates born < 32 weeks’ gestational age in the first week of age
Journal of Perinatology (2024)
-
The relationship between trajectories of renal oxygen saturation and acute kidney injury: a prospective cohort study with a secondary analysis
Aging Clinical and Experimental Research (2024)