Abstract
Background
Obesity is associated with insulin resistance (IR). Identifying high-risk obese children affected with IR is crucial to apply preventive management. We aimed to assess the diagnostic value of urinary C-peptide (UCP) and urinary C-peptide creatinine ratio (UCPCR) to diagnose IR in obese children.
Methods
This prospective cross-sectional study was performed on 60 children with obesity as the study group. Sixty healthy children of matched age and sex with normal body mass index (BMI) served as the control group. Hemostasis model for the assessment of IR (HOMA-IR), glycated hemoglobin (HbA1c), fasting blood glucose and insulin, UCP, and UCPCR were assessed in all included children.
Results
UCP and UCPCR were significantly higher in children with obesity (2.075 ± 0.783) ng/ml, (0.200 ± 0.021) nmol/mmol compared to the control group (1.012 ± 0.465) ng/ml, (0.148 ± 0.016) nmol/mmol, respectively. Both UCP and UCPCR were positively correlated with each other and with HOMA-IR, HbA1c, acanthosis nigricans, waist circumference, and BMI. At cutoff ≥2.45, the sensitivity of UCP to diagnose IR in obese children was 71.4%. At cutoff ≥0.20, the sensitivity of UCPCR to diagnose IR in obese children was 87.6%.
Conclusions
UCP and UCPCR are promising surrogate markers of IR in children and adolescents with obesity. However, UCPCR is a better marker than UCP.
Impact
-
Obesity is associated with IR. Identifying high-risk obese children affected with IR is crucial to apply preventive management.
-
We aimed to assess the diagnostic value of UCP and UCPCR to detect IR in obese children.
-
To the best of our knowledge, we are the first to use UCP and UCPCR to assess IR in obese children. We found that UCP and UCPCR are practical, easy, dependable noninvasive markers to assess IR in children with obesity and could potentially be useful in epidemiological studies and clinical practice.
Similar content being viewed by others
Introduction
Obesity is a serious health problem worldwide, especially in the pediatric population.1 Childhood obesity is associated with increased risk of metabolic syndrome, type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD), adulthood obesity, and insulin resistance (IR).2,3
IR is defined as a subnormal response of the body to insulin function.4 IR is an important link between obesity and metabolic abnormalities especially CVD.5 Obesity can cause IR through several mechanisms such as increased cytokines and hormonal production by adipose tissue.6 Adipocytes also inhibit carbohydrate metabolism through intracellular inhibition of insulin signaling.7 Besides, adiponectin, which has an insulin-sensitizing effect, is found to be decreased in obesity.8
Identification of obese children with IR is of utmost importance to define a high-risk group within the obese pediatric population who needed further management and preventive measures.9 Different methods to assess IR in children with obesity are previously validated such as hyperinsulinemic–euglycemic clamp, frequently sampled intravenous glucose tolerance test, hemostasis model for the assessment of IR (HOMA-IR), and fasting serum insulin, but none of them seem to be ideal as all of them are time-consuming, expensive, invasive, and need blood sampling.1,2,9,10,11,12 Surrogate easy noninvasive dependable biomarker for the assessment of IR is crucial. Urinary C-peptide (UCP) and urinary C-peptide creatinine ratio (UCPCR) are new easy methods used recently to assess IR in adults, but no data are available in pediatrics.13
C-peptide is secreted in equimolar amounts to insulin and is considered a surrogate biomarker for insulin.14 Moreover, 5% of C-peptide is excreted unchanged in the urine unlike insulin making urinary measures possible.15,16 UCP needs 24 h of urine collection to be measured. However, UCPCR is easier and allows the use of a single-spot urine sample.17
We hypothesize that UCP and UCPCR could be ideal biomarkers for the identification of IR in children with obesity. The aim of this study was to assess the correlation between UCP and UCPCR with HOMA-IR and to evaluate the value of UCP and UCPCR to diagnose IR in children and adolescents with obesity.
Patients and methods
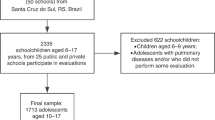
This prospective cross-sectional study was carried out at the pediatric department, Tanta University hospital during the period from January 2019 to January 2021 on 60 children and adolescents with obesity as the study group. Sixty healthy children with normal body mass index (BMI) of matched age and sex served as the control group. The study was approved by the local ethics committee of our faculty of medicine. Written informed consent was signed by the parents of all included children.
Inclusion criteria
Children and adolescents with obesity whose BMI was more than 95th percentile on Egyptian growth curves.
Exclusion criteria
Patients with secondary obesity due to medical conditions such as Cushing’s syndrome, growth hormone deficiency, hypothyroidism, and syndromic obesity, children with chronic diseases such as renal or hepatic diseases, children with abnormal oral glucose tolerance tests, and children taking drugs interfere with glucose metabolism such as corticosteroids.
All subjects included in the study were subjected to complete history taking such as age, sex of patients, gestational age, and birth weight, developmental history, medications, chronic diseases, dietetic history, and family history of obesity or any other diseases.
Anthropometric measurements
Anthropometric measurements were performed for all included children. Height was measured using a Harpenden stadiometer in the standing position. The readings of height were obtained in centimeters to the nearest 0.1 cm. Weight was measured using Seca Scale after removing the heavy outer garments and shoes. The weight was obtained in kilogram unit to the nearest 0.1 kg. BMI was calculated by dividing the weight in kilograms by the square of the height in meters, calculated as kg/m2. Height, weight, and BMI were plotted on the Egyptian growth charts suitable for age and sex to obtain a percentile ranking. Waist circumference (WC) was measured at the midpoint between the iliac crests and lower rib margin. Measurements are recorded to the nearest 0.5 cm. WC was considered to be increased when its value was at or above the 90th percentile for sex and age.18 Hip circumference was measured at the level of the greatest protrusion of the buttocks at the level of the greater trochanter to the nearest 0.5 cm.19 Waist-to-hip ratio was calculated by dividing WC by hip circumference.
Clinical examination, blood pressure, and pubertal status estimation
Clinical examination was performed to search for acanthosis nigricans and reported as present or not.20 Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured for each participant three times by the auscultation method with appropriate cuff size after 20 min of rest and the average was recorded. The average of the BP measurements was defined as hypertension if it was >95th percentile according to their age and height percentile.21 Pubertal staging was assessed and classified according to Tanner staging. Therefore, individuals were considered prepubertal when they were at stage 1 and pubertal when they were at stages 2, 3, 4, or 5.
Biochemical laboratory investigations
Laboratory investigation was performed in the form of a lipid profile that included total cholesterol (TC), triglycerides (TGs), low-density lipoprotein (LDL), and high-density lipoprotein (HDL). Fasting blood glucose (FBG) level was measured using an automatic biochemical analyzer. Fasting serum insulin level was also measured using the enzyme-linked immunosorbent assay (ELISA) method. IR was estimated using HOMA-IR, which was calculated as: HOMA-IR = fasting plasma insulin (μU/ml) × FBG (mmol/l)/22.522 and IR was defined as HOMA-IR ≥ 3.4.23 Blood samples were collected after 10–12 overnight fasting. Glycated hemoglobin (HbA1c) levels were measured by the turbidimetric inhibition immunoassay (Hitachi 911, Roche Diagnostics).
Participants were instructed to fast for 8 h overnight and to empty their bladder on awaking. A mid-stream urine sample for UCP and UCPCR was collected 2 h after eating a mixed meal at breakfast (containing carbohydrates, proteins, and fat). Urine containers with boric acid preservatives were used. The sample was sent to the laboratory on the same day. UCPCR was measured using Human C-peptide ELISA kit (DRG Instruments GmbH, Germany). Urinary creatinine was assayed using the kinetic alkaline picrate method (Abbott Architect ci16200 System). Intraassay coefficient of variation was <4%; interassay coefficient of variation was <6%.
Statistical analysis
Data were analyzed using the Statistical Package for Social Science (IBM SPSS), version 21. The data were presented as numbers and percentages for the qualitative data. Data were presented in the form of mean and standard deviations (SDs) for quantitative data with the parametric distribution. χ2 was used for the comparison of qualitative data between the two groups, while an independent t test was used for the comparison of quantitative data with parametric distribution between the two groups. Spearman’s correlation coefficient was used to assess the significant relation between quantitative parameters in the same group. Receiver-operating characteristic (ROC) curve was drawn to assess the diagnostic value of UCP and UCPCR to identify IR in children and adolescents with obesity at different cutoff points. Multivariate logistic regression was performed to assess the best predictors of IR in obese children. Significance was adopted at P < 0.05.
Results
Table 1 presented the demographic, anthropometric, and clinical characteristics of the studied groups. Weight, weight z-score, BMI, BMI z-score, WC, HC, W/H ratio, diastolic BP (DBP), systolic blood pressure (SBP), and acanthosis nigricans were significantly increased in children with obesity compared to the control group (P < 0.05).
There was no significant difference between children with obesity and the control group as regards Hb level, total leukocytic count, platelet level, HDL, urea, and creatinine levels. However, ALT, AST, TC, LDL, TG, FBG, fasting blood insulin level, HOMA-IR, and HbA1c were significantly higher in children with obesity compared to the healthy controls. UCP was significantly higher in children with obesity (2.1 ± 0.8) ng/ml compared to the control group (1 ± 0.5) ng/ml, P < 0.001. Similarly, UCPCR was significantly elevated in children with obesity (0.20 ± 0.02) nmol/mmol compared to the control group (0.15 ± 0.02) nmol/mmol, P < 0.001 (Table 2).
UCP was significantly positively correlated with UCPCR (r = 0.665, P < 0.001), HOMA-IR (r = 0.585, P = 0.001), HbA1c (r = 0.548, P = 0.002), DBP (r = 0.328, P = 0.02), WC (r = 0.518, P = 0.01), acanthosis nigricans (r = 0.510, P = 0.04), and BMI z-score (r = 0.425, P = 0.019). While UCPCR had a significant positive correlation with UCP (r = 0.665, P < 0.001), HOMA-IR (r = 0.631, P < 0.001), HbA1c (r = 0.823, P = 0.001), WC (r = 498, P = 0.0), DBP (r = 0.559, P = 0.01), acanthosis nigricans (r = 0.601, P = 0.02), and BMI z-score (r = 0.603, P = 0.001) (Table 3).
The multivariate logistic regression model showed that BMI, WC, acanthosis nigricans, HbA1c, UCP, and UCPCR were good predictors for the development of IR in obese children. Furthermore, UCPCR was the best predictor with an odds ratio (OR) of 4.74 (P = 0.001) (Table 4).
The sensitivity of UCP to diagnose IR in children with obesity at cutoff ≥2.45 was 71.4% and the specificity was 70% with an area under the curve (AUC) of 0.792 (Fig. 1). While the sensitivity of UCPCR to diagnose IR in children with obesity at cutoff ≥0.20 was 87.6%, the specificity was 84% with an AUC of 0.866 (Fig. 2)
Discussion
The main goal of our study was to assess the correlation between UCP and UCPCR with HOMA-IR and to assess their abilities to diagnose IR in children and adolescents with obesity in comparison with HOMA-IR. Our study reported that UCP and UCPCR have a strong positive correlation with HOMA-IR with a good diagnostic value to predict IR and could be used as easy rapid dependable surrogate markers of IR in non-diabetic children and adolescents with obesity. However, UCPCR was a better marker than UCP. The fact that these tests can be performed at home without the help of healthcare staff gives them great advantages to be used as a simple assessment of IR in the large-scale high-risk population.
In our study, HOMA-IR was significantly higher in children with obesity compared to the control group. This was in accordance with the results of other investigators.24,25,26,27 Numerous population-based studies have used HOMA-IR to estimate IR.9,24,25,26,27 Moreover, other researchers concluded that HOMA-IR is a reliable surrogate measure of IR and a strong predictor of type 2 diabetes in children and adolescents with obesity.12,28
HbA1c was significantly higher in children with obesity compared to the control group and was found to be a good predictor of IR in obese non-diabetic children using multivariate logistic regression. Some investigators reported that HbA1c was better than fasting glucose in predicting impaired glucose tolerance in children and adolescents with obesity.29
UCP and UCPCR were significantly higher in children with obesity than in the healthy control group. Moreover, UCP and UCPCR were significantly positively correlated with HOMA-IR. These results were in line with a study conducted by Oram et al.13 who investigated whether UCPCR could be a surrogate marker of IR by examining the correlation of UCPCR with fasting serum insulin, C-peptide, and HOMA-IR in non-diabetic adults affected with obesity and they found that UCPCR was strongly correlated with fasting serum insulin, C-peptide, and HOMA-IR and concluded that UCPCR may be a simple practical method for the assessment of IR in adult epidemiological studies.
Interestingly, both markers were positively correlated with other clinical indicators of IR such as acanthosis nigricans, BMI, and WC. Acanthosis nigricans was reported to be a good clinical indicator of underlying IR in children with obesity by many researchers.30,31,32 Similarly, WC is the most sensitive measurement for central obesity, which is one of the strongest indicators of underlying IR.33,34 Increased BMI was also known to be associated with IR in children with obesity.35 Considering the significant correlation of UCP and UCPCR with these known clinical indicators of IR suggested that both markers could be useful to predict IR.
The sensitivity of UCP to diagnose IR in children with obesity at cutoff ≥2.45 was 71.4% and the specificity was 70%. While the sensitivity of UCPCR to diagnose IR in children with obesity at cutoff ≥0.20 was 87.6% and the specificity was 84%. Moreover, multivariate logistic regression showed that UCPCR was a better predictor of IR than UCP in obese children. This indicated that UCPCR is a better reliable marker to predict IR in children with obesity than UCP; however, both showed good sensitivity to predict IR.
Obesity has dramatically increased among children in the past few decades, especially in developing countries.36 Therefore, finding an easy low-cost surrogate biomarker to predict IR in children with obesity is crucial in these countries, which cannot afford the cost of other expensive IR-related biomarkers. UCPCR is a noninvasive test and does not need proximity to a laboratory for immediate sample analysis. To the best of our knowledge, our study is the first to report UCP and UCPCR as good biomarkers for the assessment of IR in children with obesity. Our study is important because of the simplicity and practicality of using UCP and UCPCR as screening tests for IR.
Limitation of the study
First, a relatively small number of included children. Second, our interpretation of IR is based on the HOMA-IR and not on euglycemic clamp studies; however, HOMA-IR was found to be a good marker to predict IR in several studies. Third, urine collection at home is difficult in a young infant using diapers; however, obesity at this young age represents small percentages in the pediatric population. Further studies on a larger scale are needed to validate our findings and to confirm whether UCP and UCPCR could be used as screening markers to detect IR in children and adolescents with obesity.
Conclusion
UCP and UCPCR are promising easy rapid reliable markers of IR in non-diabetic obese children and adolescents. However, UCPCR was a better marker than UCP.
References
Chiarelli, F. & Marcovecchio, M. L. Insulin resistance and obesity in childhood. Eur. J. Endocrinol. 159, S67–S74 (2008).
Viner, R. M., Segal, T. Y., Lichtarowicz-Krynska, E. & Hindmarsh, P. Prevalence of insulin resistance syndrome in obesity. Arch. Dis. Child. 90, 10–14 (2005).
Chen, F. et al. Association between childhood obesity and metabolic syndrome: evidence from a large sample of Chinese children and adolescents. PLoS ONE 7, e47380 (2012).
Lee, S. H. et al. Comparison of different criteria for the definition of insulin resistance and its relationship to metabolic risk in children and adolescents. Ann. Pediatr. Endocrinol. Metab. 25, 227–233 (2020).
Nogueira-de-Almeida, C. A. & de Mello, E. D. Different criteria for the definition of insulin resistance and its relation with dyslipidemia in overweight and obese children and adolescents. Pediatr. Gastroenterol. Hepatol. Nutr. 21, 59–67 (2018).
Tagl, V. M., Giannini, G. & Chiarelli, F. Insulin resistance in children. Front. Endocrinol. 10, Article 342 (2019).
Després, J. P. & Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 444, 881–887 (2006).
Rupérez, F. J., Martos-Moreno, G. A., Chamoso-Sánchez, D., Barbas, C. & Argente, J. Insulin resistance in obese children: What can metabolomics and adipokine modelling contribute? Nutrients 12, 3310 (2020).
Conwell, L. S., Trost, S. G., Brown, W. J. & Batch, J. A. Indexes of insulin resistance and secretion in obese children and adolescents: a validation study. Diabetes Care 27, 314–319 (2004).
Chang-Rueda, C. et al. Correlation of HOMA-IR with BMI-for-age percentile in children and adolescents from the Soconusco region of Chiapas. Mex. Rev. Fa. Med. 67, 447–750 (2019).
Rossner, S. M., Neovius, M., Montgomery, S. M., Marcus, C. & Norgren, S. Alternative methods of insulin sensitivity assessment in obese children and adolescents. Diabetes Care 31, 802–804 (2008).
Keskin, M., Kurtoglu, S., Kendirci, M., Atabek, M. E. & Yazici, C. Homeostasis model assessment is more reliable than the fasting glucose/insulin ratio and quantitative insulin sensitivity check index for assessing insulin resistance among obese children and adolescents. Pediatrics 115, e500–e503 (2005).
Oram, R. A. et al. Urine C-peptide creatinine ratio can be used to assess insulin resistance and insulin production in people without diabetes: an observational study. BMJ Open 3, e003193 (2013).
Elzahar, W., Arafa, A., Youssef, A., Erfan, A. & El Amrousy, D. Urinary C-peptide creatinine ratio to differentiate type 2 diabetes mellitus from type 1 in pediatric patients. Eur. J. Pediatr. 179, 1115–1120 (2020).
Besser, R. E. Determination of C-peptide in children: when is it useful? Pediatr. Endocrinol. Rev. 10, 494–502 (2013).
Leighton, E., Sainsbury, A. R. & Jones, G. C. A practical review of c-peptide testing in diabetes. Diabetes Ther. 8, 475–487 (2017).
Jones, A. G. et al. Urine C-peptide creatinine ratio is an alternative to stimulated serum C-peptide measurement in late-onset, insulin-treated diabetes. Diabet. Med. 28, 1034–1038 (2011).
Romualdo, M. C., Nóbrega, F. J. & Escrivão, M. A. Insulin resistance in obese children and adolescents. J. Pediatr. 90, 600–607 (2014).
Cameron, N. & Bogin, B. Human Growth and Development 2nd edn, Vol. 19, 487–513 (Academic Press, 2012).
Higgins, S. T., Fremark, M. & Prose, N. S. Acanthosis nigricans: a practical approach to evaluation and management. Dermatol. Online J. 14, 2 (2008).
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114, 555–576 (2004).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
van der Aa, M. P. et al. How to screen obese children at risk for type 2 diabetes mellitus? Clin. Pediatr. 53, 337–342 (2014).
Madeira, I. R. et al. Cut-off point for homeostatic model assessment for insulin resistance (HOMA-IR) index established from receiver operating characteristic (ROC) curve in the detection of metabolic syndrome in overweight pre-pubertal children. Arq. Bras. Endocrinol. Metabol. 52, 1466–1473 (2008).
Mieldazis, S. F. et al. Hyperinsulinism assessment in a sample of prepubescent children. J. Pediatr. 86, 245–249 (2010).
Guzzaloni, G., Grugni, G., Mazzilli, G., Moro, D. & Morabito, F. Comparison between beta-cell function and insulin resistance indexes in prepubertal and pubertal obese children. Metabolism 51, 1011–1016 (2002).
Uwaifo, G. I. et al. Indices of insulin action, disposal, and secretion derived from fasting samples and clamps in normal glucose-tolerant black and white children. Diabetes Care 25, 2081–2087 (2002).
Barseem, N. F. & Helwa, M. A. Homeostatic model assessment of insulin resistance as a predictor of metabolic syndrome: consequences of obesity in children and adolescents. Egypt. Pediatr. Assoc. Gaz. 63, 19–24 (2015).
Lee, H. S., Park, H. K. & Hwang, J. S. HbA1c and glucose intolerance in obese children and adolescents. Diabet. Med. 29, e102–e105 (2012).
Chueh, H. W., Cho, G. R. & Yoo, J. H. Clinical significance of acanthosis nigricans in children and adolescents with obesity induced metabolic complications. Korean J. Pediatr. 50, 987–994 (2007).
Caceres, M., Teran, C. G., Rodriguez, S. & Medina, M. Prevalence of insulin resistance and its association with metabolic syndrome criteria among Bolivian children and adolescents with obesity. BMC Pediatr. 8, 31 (2008).
Yamazaki, H., Ito, S. & Yoshida, H. Acanthosis nigricans is a reliable cutaneous marker of insulin resistance in obese Japanese children. Pediatr. Int. 45, 701–705 (2003).
Lee, S., Bacha, F., Gungor, N. & Arslanian, S. A. Waist circumference is an independent predictor of insulin resistance in black and white youths. J. Pediatr. 148, 188–194 (2006).
Hirschler, V., Aranda, C., Calcagno, M. D. L., Maccalini, G. & Jadzinsky, M. Can waist circumference identify children with the metabolic syndrome? Arch. Pediatr. Adolesc. Med. 159, 740–744 (2005).
Lim, S. M., Choi, D. P., Rhee, Y. & Kim, H. C. Association between obesity indices and insulin resistance among healthy Korean adolescents: the JS high school study. PLoS ONE 10, e0125238 (2015).
Gupta, N., Goel, K., Shah, P. & Misra, A. Childhood obesity in developing countries: epidemiology, determinants, and prevention. Endocr. Rev. 33, 48–70 (2012).
Author information
Authors and Affiliations
Contributions
D.E.A.: acquisition of data, recruitment of patients, drafting, and final approval of the manuscript. A.A.H.: idea of the research, performing the statistical analysis, drafting, and final approval of the manuscript. W.S.: acquisition of data, performing laboratory analysis, drafting, and final approval of the manuscript. S.Elshall: acquisition of data, recruitment of patients, drafting, and final approval of the manuscript. S.Elrifaey: statistical analysis, drafting, and final approval of the manuscript. A.E.: acquisition of data, supervising the research, drafting, and final approval of the manuscript. M.H.: acquisition of data, supervising the research, drafting, and final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
IRB approval
The study was approved by the local ethics committee of the Faculty of Medicine, Tanta University, Egypt.
Patient consent
The patients were enrolled after obtaining written informed consent from their parents.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hassan, A.A., Elshall, S., Erfan, A. et al. Urinary C-peptide and urinary C-peptide creatinine ratio as markers for insulin resistance in obese children and adolescents. Pediatr Res 92, 805–809 (2022). https://doi.org/10.1038/s41390-021-01847-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01847-2