Abstract
Background
Seizures are underrecognized in preterm infants, and little is known about their impact on brain growth. We aimed to define the association between early seizures and subsequent brain growth.
Methods
Infants <30 weeks gestation underwent 72 h of prospective amplitude-integrated electroencephalography (aEEG) monitoring, term-equivalent age (TEA) magnetic resonance imaging (MRI), and 2-year neurodevelopmental testing. Seizures were defined as trains of sharp waves >10 s, evolving in frequency/amplitude/morphology, and identified using automated algorithms with manual review. Using T2-weighted images, cortical surface area (CSA) and gyrification index (GI) were calculated and volumes were segmented into five tissue classes: cerebrospinal fluid, gray matter, white matter (WM), deep nuclear gray matter, and cerebellum. Correlations between total seizure burden and tissue-specific volumes were evaluated, controlling for clinical variables of interest.
Results
Ninety-nine infants underwent aEEG/MRI assessments (mean GA = 26.3 weeks, birthweight = 899 g). Seizure incidence was 55% with a median of two events; median length = 66 s and mean burden = 285 s. Greater seizure burden was associated with smaller CSA and volumes across all tissue types, most prominently in WM (R2 = −0.603, p < 0.01), even after controlling for confounders. There was no association with GI.
Conclusions
Seizures in preterm infants are common and associated with smaller TEA brain volumes. This relationship was strongest for WM and independent of clinical factors.
Impact
-
Seizures in preterm infants are common.
-
Little is known about the association between early seizures and later brain growth.
-
Greater seizure burden is linked with smaller volumes of all brain tissue types, most prominently the WM.
-
This relationship is true even controlling for other factors.
-
Additional study is needed to identify the optimal EEG monitoring and seizure treatment strategy for improved brain growth and neurodevelopmental outcomes.
Similar content being viewed by others
Introduction
Previous investigations of seizures in preterm infants are heterogeneous in cohort composition and study design, and estimates of seizure incidence vary. Nevertheless, preterm infants are known to have more seizures than term infants,1,2,3 and a significant proportion is subclinical.4 Importantly, there is growing evidence that seizures may be associated with adverse neurologic sequelae in this population, including brain injury, intellectual impairment, and cerebral palsy.5,6,7,8 Although there is a significant overlap between seizures and preterm brain injury, most notably intraventricular hemorrhage (IVH),6,9,10,11 a pathophysiological link has not been established. It is possible that the adverse outcomes associated with seizures in infants with IVH are a direct result of the seizures, but they may also be a consequence of associated brain injury unrelated to seizures and occurring during a critical developmental window12 when the brain is undergoing rapid changes in physical size,13,14,15 gyrification,16,17 and synaptic density.18 While the relative contributions of these two mechanisms remain unclear, seizures and/or IVH may permanently alter the trajectory of brain growth.
Evaluating potential mechanistic connections between preterm seizures and subsequent adverse neurologic consequences is a high priority, as it carries important implications for electroencephalography (EEG) monitoring and seizure treatment in the neonatal intensive care unit (NICU). If seizures are indeed an independent risk factor for adverse brain growth, approaches for targeted evaluation and effective management must be developed and implemented. In this manuscript, we describe the results from an investigation that aimed to define the association between seizure burden during the first 72 h of life and brain volume, cortical surface area (CSA), and cortical folding at term-equivalent age (TEA) in a cohort of very preterm infants (born prior to 30 weeks gestation). We also examined the additional discriminatory value EEG and volumetric measures bring to the prediction of adverse neurodevelopmental outcomes. We hypothesized that early seizures would be associated with smaller brain volumes, CSA, and folding at TEA, with varying effects according to tissue type.
Methods
Cohort
Very preterm infants born before 30 completed weeks gestation were prospectively recruited for a longitudinal cerebral monitoring study between 2008 and 2016. All infants were hospitalized in the NICU at St. Louis Children’s Hospital, a level IV NICU serving urban, suburban, and rural populations. Infants were excluded if there was a known congenital or genetic anomaly or if the infant did not survive to TEA magnetic resonance imaging (MRI). Detailed clinical and demographic characteristics were collected from the medical record, including gestational age, sex, birth weight, Apgar scores at 1 and 5 min, CRIB-II (Clinical Risk Index for Babies II) score,19 antenatal steroid exposure, bronchopulmonary dysplasia (BPD, defined as supplemental oxygen beyond 36 weeks), postnatal steroid exposure, sepsis (defined as culture-positive sepsis), and necrotizing enterocolitis (NEC, defined as Bell stage IIA or greater).
aEEG monitoring and seizure classification
All infants underwent continuous two-channel amplitude-integrated EEG (aEEG) recording from the time of recruitment through 72 h of age. All monitoring was performed with the BRM3 aEEG monitor (Natus Medical, San Carlos, CA) using hydrogel electrodes arranged in the typical C3-P3, C4-P4 montage. As routine EEG/aEEG monitoring is not standard of care in this population, and the risk/benefit of seizure treatment has not yet been established, the clinical team was blinded to the monitor, and all recordings were archived and analyzed after the infant was discharged.
Detection of seizures on a limited-channel montage was enhanced by the use of a multimodal approach: utilizing an automated seizure detection algorithm, identifying changes in the aEEG baseline, and confirmation with the raw EEG. Each recording was initially screened by assessing for characteristic changes in the aEEG baseline (sudden change in the upper and lower margin of the time-compressed tracing or a “saw tooth” pattern20) or for marks placed by an automatic seizure detection algorithm. Seizures were confirmed or excluded by inspection of the raw EEG at the identified time points. Seizure-like artifactual events, such as those induced by high-frequency oscillatory ventilation,21 EKG artifact, or muscle artifact, were excluded.22 As brief seizures are not well detected by automated algorithms or aEEG baseline changes,23,24 the entire raw trace was also manually inspected for seizure activity. All EEG studies were scored by a single reviewer (Z.A.V.) with extensive experience in reading aEEG recordings of preterm infants.
Seizures were defined in the manner described by Scher et al.,25,26 namely, a series of sharp waves at least 10 s in length, which evolve in frequency, amplitude, and morphology, and are clearly distinguishable from the background and artifact. PEDs5 were not classified as seizures. Cumulative seizure burden and average seizure length were recorded.
Neuroimaging
All surviving infants underwent non-contrast brain MRI at TEA. All scans were performed using a 3 T TIM Trio system (Siemens, Erlangen, Germany) without sedating medications using an infant-specific head coil. T2-weighted turbo-spin echo sequence parameters included TR 8600 ms, TE 160 ms, and voxel size 1 mm × 1 mm × 1 mm.
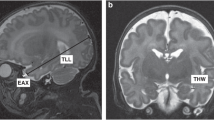
Brain volumes were delineated on native space T2-weighted images. Total and regional brain volumes were estimated using the Advanced Normalization Tools pipeline, which utilizes registration, bias correction, and tissue segmentation tools to develop probabilistic maps of tissue-specific regional volumes, followed by manual editing by a single highly experienced rater (D.A.) using ITK-Snap software tools.27,28 Calculated volumes consisted of cerebrospinal fluid (CSF), cortical gray matter, white matter (WM), deep nuclear gray matter, and cerebellum. Examples of segmented and labeled images are shown in Fig. 1. Regional brain volumes were evaluated both uncorrected and corrected for total intracranial volume (ICV).
CSF is shown in pink, cortical gray matter in green, white matter in blue, deep nuclear gray matter in yellow, and cerebellum in cyan. Infant A had 14 electrographic seizures, each lasting ~100 s each. The total white matter volume was 114.6 mL. In comparison, infant B had no detected seizures and had a total white matter volume of 160.2 mL.
CSA and gyrification index (GI), a measure of cortical folding, were generated. The cortex was reconstructed to provide mid-thickness, inflated, flat, spherical, and cerebral hull surfaces.29 The GI was calculated as the ratio of the area of the mid-thickness cortical surface to the area of the cerebral hull.30 Both measures were generated for each hemisphere using the surfaces in the individual’s native space after alignment along the anterior commissure–posterior commissure axis. For both CSA and GI, the average of the left and right hemispheres was used for analysis.
Qualitative assessment of brain injury was performed, including assessment of IVH, WMI injury (WMI), and cerebellar hemorrhage (CH). IVH was assessed using screening cranial ultrasounds performed in the first month of life as part of routine clinical care and classified based on the highest grade of injury on either side using the four-grade Papile scale.31 WMI was assessed on TEA MRI and qualitatively graded as none, punctate, or cystic. CH was also identified as present or absent on TEA MRI. As MRI has a superior sensitivity for WMI and CH, ultrasound data were not used for identification of either form of injury.32,33,34
Neurodevelopmental outcome
All surviving infants underwent comprehensive neurodevelopmental testing between 18 and 24 months corrected age using the Bayley Scales of Infant Development, Third Edition.35 Composite scores in the cognitive, language, and motor domains were obtained, and infants were classified as having moderate impairment if the score in any one of the three domains was <85 (−1 SD) or severe impairment if the score in any one domain was <70 (−2 SD).
Statistical approach
Univariate analysis of relevant demographic and clinical variables was performed using Fisher’s exact test for categorical variables and the Mann–Whitney U test for continuous variables. The univariate correlation was assessed with Pearson’s correlation coefficient, and multivariate linear regression was used to assess the strength of the relationship between cumulative seizure burden, CSA, GI, and tissue-specific regional brain volume (corrected and uncorrected for ICV), controlling for key clinical factors that may independently alter brain volumes and/or seizure incidence (gestational age, antenatal steroids, grade of IVH, grade of WMI, CH, culture-positive sepsis, NEC, BPD, and postnatal steroids). Given the potential for nonindependence imparted by the inclusion of infants of multiple gestations, linear mixed-effects modeling was used with family as a random variable, an approach previously used in neonatal studies.36,37
Our group and others have previously examined the relationship between neurodevelopmental outcome and preterm seizure burden3,6 or tissue volumes.15,38,39 However, it is likely that each of these measures (seizure burden, volumetric data, and clinical data) provide nonoverlapping information about the neurodevelopmental outcome. The additive value of regional volumetric data, CSA, and cumulative seizure burden to predict adverse neurodevelopmental outcome was assessed using binary logistic regression and area under the curve (AUC) analysis.
Statistical tests were considered significant at p < 0.05. All statistical testing was performed using R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria). The “nlme” package was used for mixed-effects modeling.
Results
Cohort description
A total of 207 infants were initially recruited for the study, and a total of 99 infants met all the inclusion criteria, survived to TEA, and had MRI scans of sufficient quality for volumetric analysis. For the 108 excluded infants, 32/108 (30%) died prior to MRI, 7/108 (6%) withdrew from the study, 24/108 (22%) were not available for a scan during the term-equivalent time window (discharged prior to TEA or were not clinically stable to travel to the scanner), and 42/108 (39%) had MRI of insufficient quality for volumetric and surface-based analysis. Excluded infants were more immature (mean GA 25.8 vs. 26.3 weeks, p < 0.01), more often male (64 vs. 47%, p < 0.01), and died more often (30 vs. 2%, p < 0.01). Birthweight and IVH incidence was not statistically different between included and excluded infants.
For the 99 included infants, the mean gestational age was 26.3 ± 1.8 weeks, the mean birthweight was 899 ± 234 g, and 54% of infants were female. The median 1- and 5-minute Apgar scores were 4 and 7, respectively. Most infants received antenatal betamethasone (90/99), and approximately half (48/99) received a complete two-dose course prior to delivery. As survival to TEA was an inclusion criterion, death was a rare event, occurring only twice in the cohort. A complete summary of clinical and demographic factors can be found in Table 1.
Brain injury outcomes
All infants included in the study cohort had high-quality (i.e., low motion) MRI scans, with a median postmenstrual age at a scan of 38 weeks (range 35–42 weeks). The first screening head ultrasound was performed at a median age of 1 day (range 0–12 days) and IVH was first diagnosed at a median age of 3 days (range 0–10 days). The incidence of IVH was comparable to other published studies of VLBW infants, with IVH of any grade in 29% of infants and grade III/IV IVH in 9% of infants. WMI was identified in 24% (24/99) of infants, one-third (7/24) of which was cystic. CH was noted in a similar proportion, with identification in 23% (23/99) of infants.
Seizure outcomes
The median duration of aEEG recording was 70 h. At least one seizure was detected in 55% of infants and infants had a median of two seizure events. The median length of individual seizures was 66 s (range 10–318 s) and the mean cumulative seizure burden was 285 s (range 0–4425 s). Of note, no infants were identified clinically as having seizures; they were all identified only by electrographic means. As the recordings were not evaluated until after discharge, no infants received antiepileptic medications for early seizures. Although none of the infants in this study had additional prospective EEG monitoring, three infants were suspected to have clinical seizures later in their hospital course. None of these events were confirmed to be electrographic seizures on subsequent EEG monitoring.
Brain injury of any type or severity was associated with an increased mean cumulative seizure burden (408 vs. 173 s, p = 0.04). There was no association between cumulative seizure burden and culture-positive sepsis, NEC, or BPD.
Volumetric analysis
The mean total cerebral volume was 280 ± 37 mL and the mean CSF volume was 111 ± 22 mL. Tissue-specific mean volumes can be found in Table 2.
Increasing seizure burden was associated with smaller volumes across all tissue types, most prominently in the WM (R2 = −0.603, p < 0.01; Fig. 2 and Table 2). In linear mixed-effects modeling, the association between cumulative seizure burden and each tissue type volume remained significant even when controlling for gestational age, antenatal steroids, brain injury, NEC, culture-positive sepsis, BPD, postnatal steroid exposure, and multiple gestations (p < 0.01). The strength of association was strongest for WM (t = −6.34), but was significant for all tissue classes (gray matter t = −2.89, deep nuclear gray matter t = −3.91, and cerebellum t = −3.41). Substituting the CRIB score for gestational age (to account for the severity of illness) did not change the outcomes, likely because of the high degree of collinearity between the two values (R2 = −0.91).
In addition to smaller volumes across tissue types, there was a notable association between greater seizure burden, smaller total intracranial volume, and greater CSF volume. When correcting for total intracranial volume, WM and CSF volumes remained significantly associated with cumulative seizure burden (Table 3).
Cortical surface measures
CSA and GI measures were generated for all 99 infants. The mean CSA was 257 ± 38 cm2 and the mean GI was 1.79 ± 0.12, consistent with previously published reports. Smaller mean CSA was associated with increasing cumulative seizure burden, even after correcting for gestational age, antenatal steroids, brain injury, NEC, BPD, culture-positive sepsis, postnatal steroid exposure, and multiple gestations (t = −3.71, p < 0.01). There was no association between mean GI and cumulative seizure burden (t = −1.46, p = 0.14). There were no notable differences in the association between left and right measures of CSA or GI. A summary of all models is shown in Supplemental Table 1.
Neurodevelopmental outcomes
As two infants died after TEA but before neurodevelopmental testing, 97 infants were eligible for follow-up at age 18–24 months. Eighty-two of these infants returned for neurodevelopmental testing, for a follow-up rate of 85%. The median cognitive, language, and motor composite scores were 85, 89, and 85, respectively. Most infants were identified as having a moderate impairment (52/82, 63%), while a smaller number had severe impairment (12/82, 15%; Supplemental Table 2). A baseline model consisting of standard clinical variables (gestational age, antenatal steroids, presence of brain injury, NEC, BPD, sepsis, and postnatal steroids) was moderately predictive of severe outcome with an AUC of 0.787. Incorporation of regional MRI volumes and cumulative seizure burden in the model increased the strength of the prediction, reflected as higher AUC values of 0.865 and 0.878, respectively.
Discussion
These results demonstrate an association between TEA brain volumes, average CSA, and cumulative seizure burden as measured by two-channel EEG in the first 72 h following birth in preterm infants. This association remains significant even when controlling for other clinical factors, which might alter seizure incidence or brain development, including gestational age, antenatal steroid exposure, and all three common forms of preterm brain injury (i.e., IVH, WMI, CH). There was no significant association between seizure burden and GI. While cumulative seizure burden was associated with smaller volumes across all tissue types at TEA, it was most strongly linked with smaller WM volumes.
Consistent with other limited-channel EEG studies, we noted a high incidence (55%) of seizures that were exclusively without clinical correlate. Other prospective studies have reported similar frequencies of electrographic seizures identified using aEEG in this population, with rates between 22 and 63% (5,6,9). This high incidence of subclinical seizures across cohorts highlights the necessity of prospective monitoring to measure seizure incidence in this population, and it is clear that reliance on clinical detection alone will lead to significant underreporting.2,40 As is common in investigations of low birthweight infants, rates of brain injury across these studies were also high, with neuroimaging abnormalities detected in ~40% of infants. While this injury might independently drive risk for seizures or alter trajectories of brain growth, in this study, relationships between seizure burden and brain volumes remain significant across tissue types even when controlling for these factors.
Brain injury in preterm infants is complex and appears to be caused by a variety of dysmaturational disturbances that affect both white and gray matter, a condition sometimes referred to as encephalopathy of prematurity.4 It is interesting that WM volumes were most strongly associated with seizure burden, as the WM is particularly vulnerable at this developmental stage.41,42,43 It should also be noted that the distinction between WM and gray matter is somewhat arbitrary, as virtually all axons have their origin and termination in gray matter. Thus, injury to one tissue type would be expected to affect the other. This destruction-development link in gray and WM is further supported by an autopsy series in which WMI was associated with thalamic and cortical gray matter atrophy.44,45
The role of seizures in this process is not clear, although seizures have been implicated as a possible cause of brain injury in human and animal models.46 Miller et al. demonstrated abnormal cerebral metabolism and evidence of neuronal injury in proportion to seizure burden in a cohort of infants with perinatal asphyxia.47 Similarly, epilepsy has previously been implicated in microstructural WM changes.48 Further, preclinical studies support a significant deleterious impact of seizures on synaptogenesis,49,50 dendritic proliferation,51 and myelination,52 all processes that are active during the third trimester of gestation, a period when very preterm infants are confined to the NICU. Thus, although we have shown an association between seizures and brain volumes and not cause and effect, it is plausible that seizures play an active role in causing injury that independently reduces brain volumes.
Importantly, defining seizures in neonates has been a consistent challenge across investigations, even more so in preterm infants who also display electrographic events termed “periodic epileptiform discharges” or PEDs on aEEG. PEDs are characterized by alternating sharp-slow waves with a periodicity of 0.5–4 s but, unlike classic ictal discharges, do not evolve with respect to time or location.5 PEDs were initially described in adults and older infants and are strongly associated with later epilepsy and poor outcome.53,54 For preterm infants, however, PEDs have not been associated with brain injury or poor cognitive outcome.5 Consistent with previous studies, PEDs were not classified as seizures in this investigation.
As shown in this analysis, models that incorporate information from a variety of modalities provide a more complete and accurate picture of future neurodevelopmental outcomes than factors from a single domain. The stressors found in the NICU affect the brain on many scales, from micro- to macrostructural levels. Capturing each element of risk is essential for the most comprehensive view. While clinical variables alone provide a moderate level of accuracy, the incremental improvement in AUC after the addition of regional MRI volumes and cumulative seizure burden indicates that there is an additional predictive value added by these variables.
As the association between preterm seizure burden, brain injury, and morbidity becomes increasingly clear,2 there is a developing urgency to understand the role of medications in treating seizures and improving outcomes. Limited existing data suggest that a reduction in seizure burden by treatment with phenobarbital may modify brain injury risk in preterm infants.55 However, caution should be urged at this juncture as the data on antiepileptic medications in the preterm population are limited and primarily retrospective in nature. This concern is further highlighted by the neurodevelopmental risks associated with the use of antiepileptic drugs in neonates,56 specifically phenobarbital,57,58 the conventional first-line seizure treatment. While phenobarbital remains the most commonly used treatment,2,59 treatment failure rates as high as 63% have been reported.2 Further, in a retrospective study with limited follow-up and in which seizure burden was not accounted for, phenobarbital was associated with decreased cognitive scores at 2 years.60 Levetiracetam has also been explored as an alternative agent with fewer neurodevelopmental side effects,61,62 but there is concerning data about lack of efficacy.63 To reach a consensus regarding seizure treatment in preterm infants, randomized controlled trials of the effect of treatment on neurodevelopmental outcomes are clearly needed.
There are several limitations of this study. First, although seizures were identified using a robust approach (aEEG baseline evaluation, algorithmic detection, confirmation on raw EEG, manual second-by-second review), seizure detection may have been further enhanced by the use of conventional EEG, which provides more complete coverage of the cortex. Second, EEG recordings were made only during the first 72 h of life in this study. Although a consensus is beginning to emerge that seizures are more common than previously thought and vastly underrecognized in preterm infants, the true burden of seizures, which can occur over weeks, remains unknown. Third, although each included infant has robust clinical and imaging data, the study design necessarily requires survival to term-corrected age, resulting in the unavoidable exclusion of roughly half of the originally enrolled infants. Fourth, rates of injury in this cohort are significant, although not entirely surprising given the significant degree of prematurity. Finally, each infant underwent a single MRI at TEA. While this provides valuable insight into the final volume of each tissue type, longitudinal data would provide a better understanding of the altered trajectories of brain growth in this cohort.
Conclusions
This study provides indirect evidence of the deleterious impact of seizures on brain development, with a strong association noted between cumulative seizure burden and brain tissue volumes. While IVH, CH, and WMI remain important causes of subsequent neurodevelopmental impairment, seizures may drive deleterious neuropathological effects independent of macro-scale anatomic injury. Improving the quality and accuracy of outcome prediction is a high-priority goal in clinical care. The iterative improvement in model accuracy, as demonstrated by the increase in AUC from 0.783 to 0.878 after the inclusion of volumetric and seizure burden data, suggests that each of these measures provides additive, non-overlapping information about risk for subsequent neurodevelopmental impairment.
This finding has important potential implications for the evaluation and treatment of preterm seizures. Currently, there is a paucity of evidence to support routine prospective EEG monitoring for subclinical seizures in asymptomatic preterm patients or treatment of seizures if detected, particularly given the potential for harmful side effects64 and unclear efficacy65 of antiepileptic medication use. Based upon these results, future studies remain necessary which include longitudinal EEG monitoring to evaluate the seizure burden outside of the first 72 h of life, comparison of the utility of conventional versus amplitude-integrated EEG (specifically if the tradeoff of decreased seizure detection is offset by better tolerance of electrodes), further solidification of seizure definitions (including PEDs) tailored to the preterm population, and, ultimately, a randomized controlled trial of treatment versus no treatment to determine if seizure treatment in very preterm infants improves brain development and long-term neurodevelopmental outcomes.
References
Scher, M. S. Neonatal seizure classification: a fetal perspective concerning childhood epilepsy. Epilepsy Res. 70, 41–57 (2006).
Glass, H. C. et al. Seizures in preterm neonates: a multicenter observational cohort study. Pediatr. Neurol. 72, 19–24 (2017).
Spagnoli, C. et al. Symptomatic seizures in preterm newborns: a review on clinical features and prognosis. Ital. J. Pediatr. 44, 115 (2018).
Volpe, J. J. & Volpe, J. J. (eds). Volpe’s Neurology of the Newborn 6th edn (Elsevier, 2018).
Weeke, L. C. et al. Rhythmic EEG patterns in extremely preterm infants: classification and association with brain injury and outcome. Clin. Neurophysiol. 128, 2428–2435 (2017).
Vesoulis, Z. A. et al. Early electrographic seizures, brain injury, and neurodevelopmental risk in the very preterm infant. Pediatr. Res. 75, 564–569 (2014).
Davis, A. S. et al. Seizures in extremely low birth weight infants are associated with adverse outcome. J. Pediatr. 157, 720–725.e1-2 (2010).
Pinchefsky, E. F. & Hahn, C. D. Outcomes following electrographic seizures and electrographic status epilepticus in the pediatric and neonatal ICUs. Curr. Opin. Neurol. 30, 156–164 (2017).
Shah, D. K. et al. Electrographic seizures in preterm infants during the first week of life are associated with cerebral injury. Pediatr. Res. 67, 102–106 (2010).
Lloyd, R. O. et al. Electrographic seizures during the early postnatal period in preterm infants. J. Pediatr. 187, 18–25.e2 (2017).
Strober, J. B., Bienkowski, R. S. & Maytal, J. The incidence of acute and remote seizures in children with intraventricular hemorrhage. Clin. Pediatr. 36, 643–647 (1997).
Matthews, L. G. et al. Brain growth in the NICU: critical periods of tissue-specific expansion. Pediatr. Res. 83, 976–981 (2018).
Boardman, J. P. et al. Early growth in brain volume is preserved in the majority of preterm infants. Ann. Neurol. 62, 185–192 (2007).
Padilla, N. et al. Brain growth gains and losses in extremely preterm infants at term. Cereb. Cortex 25, 1897–1905 (2015).
Kidokoro, H. et al. Brain injury and altered brain growth in preterm infants: predictors and prognosis. Pediatrics 134, e444–e453 (2014).
Armstrong, E. et al. The ontogeny of human gyrification. Cereb. Cortex 5, 56–63 (1995).
Ajayi-Obe, M. et al. Reduced development of cerebral cortex in extremely preterm infants. Lancet 356, 1162–1163 (2000).
Huttenlocher, P. R. & Dabholkar, A. S. Regional differences in synaptogenesis in human cerebral cortex. J. Comp. Neurol. 387, 167–178 (1997).
Parry, G., Tucker, J. & Tarnow-Mordi, W. UK Neonatal Staffing Study Collaborative Group. CRIB II: an update of the clinical risk index for babies score. Lancet 361, 1789–1791 (2003).
Hellström-Westas, L., De Vries, L. S. & Rosén, I. Atlas of Amplitude-Integrated EEGs in the Newborn (Informa Healthcare; Distributed in North and South America by Taylor & Francis, 2008).
Tao, J. D. & Mathur, A. M. Using amplitude-integrated EEG in neonatal intensive care. J. Perinatol. 30, S73–S81 (2010).
Sazgar, M. & Young, M. G. in Absolute Epilepsy and EEG Rotation Review 149–162 (Springer International Publishing, 2019).
Sun, J., Ma, D. & Lv, Y. Detection of seizure patterns with multichannel amplitude-integrated EEG and the color density spectral array in the adult neurology intensive care unit. Medicine 97, e12514 (2018).
Rakshasbhuvankar, A. et al. Amplitude-integrated EEG for detection of neonatal seizures: a systematic review. Seizure 33, 90–98 (2015).
Shellhaas, R. A. et al. The American Clinical Neurophysiology Society’s Guideline on Continuous Electroencephalography Monitoring in Neonates. J. Clin. Neurophysiol. 28, 611–617 (2011).
Scher, M. S. et al. Ictal and interictal electrographic seizure durations in preterm and term neonates. Epilepsia 34, 284–288 (1993).
Tustison, N. J. et al. The ANTs cortical thickness processing pipeline. In Proc. SPIE 8672, Medical Imaging 2013: Biomedical Applications in Molecular, Structural, and Functional Imaging (eds Weaver, J. B. & Molthen R. C.) 86720K (SPIE—International Society for Optics and Photonics, 2013).
Tustison, N. J. et al. The ANTs longitudinal cortical thickness pipeline. Neuroscience http://biorxiv.org/lookup/doi/10.1101/170209 (2017).
Hill, J. et al. A surface-based analysis of hemispheric asymmetries and folding of cerebral cortex in term-born human infants. J. Neurosci. 30, 2268–2276 (2010).
Engelhardt, E. et al. Regional impairments of cortical folding in premature infants. Ann. Neurol. 77, 154–162 (2015).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Parodi, A. et al. Accuracy of ultrasound in assessing cerebellar haemorrhages in very low birthweight babies. Arch. Dis. Child Fetal Neonatal Ed. 100, F289–F292 (2015).
Benders, M. J. N. L., Kersbergen, K. J. & de Vries, L. S. Neuroimaging of white matter injury, intraventricular and cerebellar hemorrhage. Clin. Perinatol. 41, 69–82 (2014).
de Vries et al. The premature brain: ultrasound or MRI? Neuroradiology 55, 13–22 (2013).
Bayley, N. Bayley Scales of Infant and Toddler Development: Motor Scale (Psychological Corp., 2006).
Burkett, K. M. et al. A comparison of statistical methods for the discovery of genetic risk factors using longitudinal family study designs. Front. Immunol. 6, 589 (2015).
Shaffer, M. L., Kunselman, A. R. & Watterberg, K. L. Analysis of neonatal clinical trials with twin births. BMC Med. Res. Methodol. 9, 12 (2009).
Cheong, J. L. Y. et al. Brain volumes at term-equivalent age are associated with 2-year neurodevelopment in moderate and late preterm children. J. Pediatr. 174, 91–97.e1 (2016).
Strahle, J. M. et al. Impaired hippocampal development and outcomes in very preterm infants with perinatal brain injury. Neuroimage Clin. 22, 101787 (2019).
Scher, M. S. et al. Electrographic seizures in preterm and full-term neonates: clinical correlates, associated brain lesions, and risk for neurologic sequelae. Pediatrics 91, 128–134 (1993).
Khwaja, O. & Volpe, J. J. Pathogenesis of cerebral white matter injury of prematurity. Arch. Dis. Child Fetal Neonatal Ed. 93, F153–F161 (2007).
The PIPARI Study Group et al. Preterm infants’ early growth and brain white matter maturation at term age. Pediatr. Radiol. 43, 1357–1364 (2013).
Jensen, F. E. Developmental factors regulating susceptibility to perinatal brain injury and seizures. Curr. Opin. Pediatr. 18, 628–633 (2006).
Pierson, C. R. et al. Gray matter injury associated with periventricular leukomalacia in the premature infant. Acta Neuropathol. 114, 619–631 (2007).
Nagasunder, A. C. et al. Abnormal microstructure of the atrophic thalamus in preterm survivors with periventricular leukomalacia. Am. J. Neuroradiol. 32, 185–191 (2011).
Schmid, R., Tandon, P., Stafstrom, C. E. & Holmes, G. L. Effects of neonatal seizures on subsequent seizure-induced brain injury. Neurology 53, 1754–1754 (1999).
Miller, S. P. et al. Seizure-associated brain injury in term newborns with perinatal asphyxia. Neurology 58, 542–548 (2002).
Buksakowska, I. et al. Distinctive patterns of seizure-related white matter alterations in right and left temporal lobe epilepsy. Front. Neurol. 10, 986 (2019).
Zhou, C., Lippman, J. J. B., Sun, H. & Jensen, F. E. Hypoxia-induced neonatal seizures diminish silent synapses and long-term potentiation in hippocampal CA1 neurons. J. Neurosci. 31, 18211–18222 (2011).
Katsarou, A.-M., Moshé, S. L. & Galanopoulou, A. S. Interneuronopathies and their role in early life epilepsies and neurodevelopmental disorders. Epilepsia Open 2, 284–306 (2017).
Casanova, J. R., Nishimura, M. & Swann, J. W. The effects of early-life seizures on hippocampal dendrite development and later-life learning and memory. Brain Res. Bull. 103, 39–48 (2014).
Dwyer, B. E. & Wasterlain, C. G. Electroconvulsive seizures in the immature rat adversely affect myelin accumulation. Exp. Neurol. 78, 616–628 (1982).
Hamano, K., Iwasaki, N., Takeya, T. & Takita, H. Clinical significance of periodic lateralized epileptiform discharges in children with relation to level of consciousness. Pediatr. Neurol. 11, 28–32 (1994).
Chong, D. J., Hirsch, L. J. & Which, E. E. G. Patterns warrant treatment in the critically ill? Reviewing the evidence for treatment of periodic epileptiform discharges and related patterns. J. Clin. Neurophysiol. 22, 79–91 (2005).
Mikati, M. A. et al. Phenobarbital modifies seizure-related brain injury in the developing brain. Ann. Neurol. 36, 425–433 (1994).
Noguchi, K. K. et al. Brain pathology caused in the neonatal macaque by short and prolonged exposures to anticonvulsant drugs. Neurobiol Dis 149, 105245 (2020).
Farwell, J. R. et al. Phenobarbital for febrile seizures-effects on intelligence and on seizure recurrence. N. Engl. J. Med. 322, 364–369 (1990).
Kwan, P. & Brodie, M. J. Phenobarbital for the treatment of epilepsy in the 21st century: a critical review. Epilepsia 45, 1141–1149 (2004).
Glass, H. C., Kan, J., Bonifacio, S. L. & Ferriero, D. M. Neonatal seizures: treatment practices among term and preterm infants. Pediatr. Neurol. 46, 111–115 (2012).
Maitre, N. L., Smolinsky, C., Slaughter, J. C. & Stark, A. R. Adverse neurodevelopmental outcomes after exposure to phenobarbital and levetiracetam for the treatment of neonatal seizures. J. Perinatol. 33, 841–846 (2013).
Han, J. Y. et al. Efficacy of levetiracetam for neonatal seizures in preterm infants. BMC Pediatr. 18, 131 (2018).
Khan, O. et al. Role of Intravenous Levetiracetam for Acute Seizure Management in Preterm Neonates. Pediatr. Neurol. 49, 340–343 (2013).
Kurtom, W. et al. Lack of response to treatment with levetiracetam in extreme preterm infants with seizures. J. Perinatol. 39, 1480–1484 (2019).
Volpe, J. J. Neurology of the Newborn 5th edn (Saunders/Elsevier, 2008).
Weeke, L. C. et al. Lidocaine response rate in aEEG-confirmed neonatal seizures: retrospective study of 413 full-term and preterm infants. Epilepsia 57, 233–242 (2016).
Acknowledgements
This work was supported by NIH Career Development Awards: K23 NS111086 (to Z.A.V.), K02 NS089852 (to C.S.), and K23 MH105179 (to C.R.). NIH Grants: P30 NS098577, R01 HD061619, R01 HD057098, R01 MH113570, and P50 HD103525. Washington University Institute of Clinical and Translational Sciences KL2 Training Program (NIH/NCATS KL2 TR000450) (to Z.A.V.). The Barnes-Jewish Hospital Foundation and the Washington University ICTS Clinical and Translational Funding Program (NIH/NCATS UL1 TR000448). Doris Duke Charitable Foundation (to C.R.), Dana Foundation (to C.S.), Child Neurology Foundation (to C.S.), and Cerebral Palsy International Research Foundation (to C.S.).
Author information
Authors and Affiliations
Contributions
Z.A.V. developed the study idea, interpreted, and collected aEEG data, performed the statistical analysis, generated figures, and wrote the initial manuscript draft. D.A. collected and analyzed MRI data, generated figures, and critically reviewed the manuscript. C.R., J.N., and C.S. participated in study development, and critically reviewed the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Statement of consent
Informed written consent was obtained for all participants prior to any study procedures.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Vesoulis, Z.A., Alexopoulos, D., Rogers, C. et al. Seizure burden in preterm infants and smaller brain volume at term-equivalent age. Pediatr Res 91, 955–961 (2022). https://doi.org/10.1038/s41390-021-01542-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01542-2