Abstract
Background
Extra-corporeal membrane oxygenation (ECMO) is a life-saving intervention for severe respiratory and cardiac diseases. However, 50% of survivors have abnormal neurologic exams. Current ECMO management is guided by systemic metrics, which may poorly predict cerebral perfusion. Continuous optical monitoring of cerebral hemodynamics during ECMO holds potential to detect risk factors of brain injury such as impaired cerebrovascular autoregulation (CA).
Methods
We conducted daily measurements of microvascular cerebral blood flow (CBF), oxygen saturation, and total hemoglobin concentration using diffuse correlation spectroscopy (DCS) and frequency-domain diffuse optical spectroscopy in nine neonates. We characterize CA utilizing the correlation coefficient (DCSx) between CBF and mean arterial blood pressure (MAP) during ECMO pump flow changes.
Results
Average MAP and pump flow levels were weakly correlated with CBF and were not correlated with cerebral oxygen saturation. CA integrity varied between individuals and with time. Systemic measurements of MAP, pulse pressure, and left cardiac dysfunction were not predictive of impaired CA.
Conclusions
Our pilot results suggest that systemic measures alone cannot distinguish impaired CA from intact CA during ECMO. Furthermore, optical neuromonitoring could help determine patient-specific ECMO pump flows for optimal CA integrity, thereby reducing risk of secondary brain injury.
Impact
-
Cerebral blood flow and oxygenation are not well predicted by systemic proxies such as ECMO pump flow or blood pressure.
-
Continuous, quantitative, bedside monitoring of cerebral blood flow and oxygenation with optical tools enables new insight into the adequacy of cerebral perfusion during ECMO.
-
A demonstration of hybrid diffuse optical and correlation spectroscopies to continuously measure cerebral blood oxygen saturation and flow in patients on ECMO, enabling assessment of cerebral autoregulation.
-
An observation of poor correlation of cerebral blood flow and oxygenation with systemic mean arterial pressure and ECMO pump flow, suggesting that clinical decision making guided by target values for these surrogates may not be neuroprotective.
-
~50% of ECMO survivors have long-term neurological deficiencies; continuous monitoring of brain health throughout therapy may reduce these tragically common sequelae through brain-focused adjustment of ECMO parameters.
Similar content being viewed by others
Introduction
Extra-corporeal membrane oxygenation (ECMO) has been utilized for refractory respiratory and/or cardiac failure in children for over 20 years.1 In this study, we focus on veno-arterial (VA) ECMO, which involves cannulation of large vessels to divert a portion of venous flow through a membrane oxygenator and mechanical pump.2 ECMO provides support to both the heart and lungs by returning oxygenated blood to the body. The long-term neurological morbidity rate for pediatric ECMO survivors is more than 50%,1,3 prompting increased attention to improving ECMO management of ECMO.1,4
Current management of ECMO is guided by age-appropriate mean arterial blood pressure (MAP) and blood gas parameters. Accordingly, aberrant changes in MAP typically trigger adjustments in pump flow to maintain MAP targets and thus end-organ perfusion. For the brain, this paradigm assumes MAP variations are directly coupled to cerebral blood flow (CBF) changes, in effect, assuming cerebrovascular autoregulation (CA) is disrupted. Prior work exploring CA during pediatric ECMO, however, did not directly monitor CBF at the bedside in humans.5,6,7,8,9 While CBF monitoring using xenon clearance techniques has been explored,10 this is not practical for continuous bedside monitoring.
To this end, we introduce a noninvasive hybrid optical approach for cerebral monitoring during ECMO. Our instrumentation utilizes diffuse correlation spectroscopy (DCS) to measure CBF and frequency-domain diffuse optical spectroscopy (FD-DOS) to measure hemoglobin concentrations and optical scattering. This DOS + DCS approach has been deployed to study other pediatric diagnoses,11,12 but has not previously been applied to ECMO. DCS provides a quantitative CBF index that enables evaluation of the temporal correlation between MAP and CBF to assess the integrity of CA in individuals and as a function of time. Thus, in this work, we directly measure cerebral hemodynamics to explore the hypothesis that CA is impaired during ECMO.
Specifically, we measured the correlation between CBF and MAP to assess CA, and we examined the variability of CA within and between individuals during ECMO. We found that this variability is not predicted by systemic measures of MAP, pulse pressure, and left cardiac dysfunction. This finding motivates the need for direct, individualized, and continuous assessment of CA.
FD-DOS also quantifies cerebral microvascular oxygen saturation (StO2) and total hemoglobin concentration (Hbt), which we compared with systemic MAP and pump flow levels. Our intersubject results were highly heterogeneous for CA integrity and cerebral hemodynamics, likely in part due to ECMO patient heterogeneity. Ultimately, DOS + DCS metrics have potential to identify temporal periods of high risk for neurological injury, enabling personalized intervention. This pilot study demonstrates the potential of DOS + DCS to provide additional bedside insight into cerebral health.
Cerebrovascular regulation (autoregulation) and ECMO therapy: background
CA mechanisms control cerebrovascular resistance to maintain adequate CBF to meet metabolic demands.13,14 Within the MAP limits of pressure autoregulation, these mechanisms guard against the development of inadequate or excessive cerebral blood flow that can produce ischemic or hyperemic brain injury (Fig. 1b). Although this view of CA has been challenged,13,15 we adopt Lassen’s relatively simple model16 for the quasi-static flow states in this experiment.
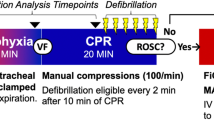
a Timeline of dynamic measurement, showing nominal steps in ECMO pump flow. The actual change, number of steps, and rate of change was limited by the clinical team based on individual patient response. b Schematic of CBF vs. MAP16: at high and low MAP, flow is pressure-controlled. At blood pressures within the pressure limits of autoregulation (dotted lines), flow is regulated; outside this zone, the brain is at risk for hemorrhage or ischemia. The pressure limits of autoregulation are not well understood in neonates and are expected to change with disease state. For example, the lower limit may shift, narrowing the range of regulated flow (maroon curve). Schematics of: c blood circulation; and d FD-DOS/DCS monitoring during ECMO. Optical measurements include the DCS index of CBF (BFI); and FD-DOS measurement of cerebral oxygen saturation (StO2) and total hemoglobin concentration (Hbt).
The ECMO circuit provides a source of steady perfusion in parallel with the heart’s pulsatile perfusion (Fig. 1c); the relative contributions vary between patients and over time. During ECMO, clinicians often adjust MAP using pump flow (PF), based on systemic vital signs.1 As these metrics lack specificity for brain perfusion, such adjustments may produce blood pressures outside an individual’s current autoregulatory range, causing inappropriate cerebral perfusion pressure. This problem is worsened by the disruption of other CA mechanisms during ECMO.5,17,18,19
Difficulties also exist with assessing brain health during ECMO. Neonatal neurological exams are compromised by developmental stage and sedation, leading to the use of EEG and cranial ultrasound, but neither can provide high-quality predictions or evaluations of neuro-injury,1 e.g., ~50% of neonates with “normal” ultrasounds have abnormal MRI post-ECMO.20 Although a few studies have used oxygen saturation to investigate cerebral perfusion,6,7,8 there is limited understanding of adequate cerebral perfusion during ECMO10,21 or the normative blood pressure range of CA.9 DCS and FD-DOS are promising tools to address these needs.
Diffuse optical and correlation spectroscopies
DOS and DCS are related technologies which utilize light ~650−950 nm to probe tissue. While DOS measures chromophore concentrations (primarily oxy- and deoxy-hemoglobin), DCS measures moving scattering bodies (primarily red blood cells).
FD-DOS uses intensity-modulated light to probe the head and brain. A diffusion model of light transport allows separation of the effects of tissue absorption from scattering.22 This separation, combined with multiwavelength measurements, enables quantitative estimates of oxy- and deoxy-hemoglobin concentrations, and thus of StO2 and Hbt. By contrast, devices utilizing constant or slowly varying light sources (e.g., many commercial cerebral oximeters23,24) are unable to separate scattering from absorption and are therefore limited to trend monitoring. Quantitative optical measurements are important during changing physiological conditions, e.g., developing edema during ECMO.
In addition to FD-DOS, DCS employs photon correlation techniques to derive a blood flow index (BFI) proportional to CBF.25,26,27 Combining these devices into a hybrid system allows simultaneous measurement of blood flow, hemoglobin content, and hemoglobin oxygen saturation. A major advantage of DOS + DCS is the ability to make serial or continuous measurements. In part, our study sought to identify temporal changes in cerebral hemodynamics during ECMO.
Methods
All patients from English-speaking families cannulated for VA-ECMO at the Children’s Hospital of Philadelphia were eligible for enrollment. The responsible clinical team was consulted prior to approach for enrollment and each measurement. Clinically unstable subjects were excluded from the study. Under an Institutional Review Board-approved protocol, informed consent was obtained by a physician researcher.
Several metrics of overall and cardiac health were calculated for each study participant. A Functional Status Score28 was calculated at both ICU admission and discharge; Pediatric Risk of Mortality III Scores29 were also calculated. Arterial pulse pressure (PP = systolic − diastolic BP) was examined as a readily available metric of cardiac health. Clinically ordered echocardiograms were assessed for cardiac dysfunction.
Upon enrollment, ~1-h daily optical FD-DOS/DCS monitoring sessions were conducted (Table 1). Monitoring ended due to clinical instability, weaning from or withdrawal of ECMO, parental choice, or at the fifth day of ECMO. The monitoring session consisted of two phases: (1) baseline measurements of BFI, StO2, and Hbt and (2) CA assessment. Subject measurements with low-quality signal (e.g., DCS photon count rate <10 kHz), non-neonates, and recipients of extended (>15 min) CPR were excluded from the current analysis. Additionally, measurements following dramatic swelling in one subject (>30% change in body weight) were excluded due to potential failure of the diffusion approximation. Study personnel continuously observed the subjects during data collection. Motion artifacts were manually recorded and these periods excluded from further analysis. Additionally, artifacts were identified using both the temporal derivative and absolute value of blood pressure and pump flow.
Baseline measurements and CA assessment
Details of the hybrid DOS + DCS instrument have been described elsewhere and are summarized in the online supplement.30 A semi-infinite model was used for analysis of both DOS and DCS data. Baseline measurements were collected each day using a custom-built flexible patient interface with embedded fiber optics manually placed on the subject’s forehead. Measurements were limited to the right side only due to cannula placement. For each baseline period of ~5 min, tissue oxygen saturation (StO2,o), hemoglobin content (Hbt,o), and reduced scattering coefficient (µ′s,o) were quantified.
After the baseline measurements, a lighter and more conformable DOS + DCS probe was utilized for CA measurements. FD-DOS measurements of StO2 and Hbt utilized a single source-detector separation to calculate temporal changes from baseline.31 FD-DOS temporal data were only available for 15 of 22 monitoring sessions. The DOS measurement was sensitive to signal-to-noise issues due to the relatively small source and detector fibers required for the lightweight probe.
For the CA assessment phase, interleaved FD-DOS and DCS measurements were acquired every 7 s on the subject’s right forehead during serial PF variation (Fig. 1a, 30−60 min, depending on toleration of flow variation). In addition to the optical data, time-synchronized clinical vital signs, and ECMO system parameters (Transonic HT-100 flow meter, Spectrum Medical M2) were recorded (CNS, Moberg Research). These data included pulse and mean arterial pressures (PP, MAP), venous oxygen saturation (SvO2), arterial oxygen saturation (SaO2), and PF (normalized by weight). Temporal data sets utilized for CA assessment were normalized to a ~5-min period prior to any manipulation.
PF changes were performed by the bedside perfusionist in steps of approximately ±10% from baseline. Each step was maintained for ~5 min (Fig. 1a) prior to return to baseline PF. In initial measurements (subjects 1, 2), we aimed to undertake four 10% steps (i.e., 80−120% of baseline). However, we found patient-specific flow limitations (e.g. high venous line pressures) often prevented PF adjustments by the full range. In these cases, a subset of the range was used. As ±10% changes were found to sufficiently alter MAP, PF adjustments were subsequently limited to ~90 and ~110% of baseline. The speed and exact timing of the adjustments was left to the perfusionist’s discretion, which was guided by the actual and expected response of the patient to flow changes. Note that reported PF is normalized by body weight (L/min/kg).
Data processing and statistical analysis
Baseline cerebral hemodynamic and baseline circulatory parameters (symbolized by Xo) were compared across individuals and measurement days. Specifically, we computed the Pearson correlation coefficient between: (1) BFIo and MAPo; (2) BFIo and PFo; (3) PFo and MAPo; (4) StO2,o and MAPo; (5) StO2,o and PFo; (6) StO2,o and SvO2,o; and (7) PPo and MAPo (corrcoef, MATLAB R2017a, Mathworks).
For each CA assessment (N = 22, Table 1), relative MAP and BFI data were computed as a function of monitoring time, t, during cyclical PF variation (Fig. 1a), i.e., rMAP(t) ≡ MAP(t)/MAPo, rBFI(t) ≡ BFI(t)/BFIo. CA was characterized by the DCSx index, which is the Pearson’s correlation coefficient between rMAP(t) and rBFI(t). To examine the impact of baseline circulatory parameters on CA, we grouped DCSx measurements by MAPo terciles, low/moderate/high PPo, and severe/moderate/mild left cardiac dysfunction. A Wilcoxon rank sum test was then employed to test for differences in DCSx across the three groups for each circulatory parameter. Low/moderate/high PPo corresponded to PPo < 8 mmHg, 8 < PPo < 15 mmHg, and PPo > 15 mmHg, respectively. Severe/moderate/mild left cardiac dysfunction was assessed by a blinded independent reviewer of clinical echocardiograms. The reviewer’s scores were compared with the clinical assessment scores; the more conservative score was used if there was disagreement. Finally, we present two case examples of concurrent time-series rBFI and StO2 data.
Results
We measured a total of 15 children. The present analysis focuses on neonates. One subject was therefore excluded from the present analysis due to age (7 years). Additionally, one subject was excluded due to low DCS signal-to-noise ratio, and four subjects were excluded due to persistent artifacts in vitals signs or PF. Lastly, one subject was only partially included in this analysis due to significant swelling that occurred between measurement days 1 and 2 (with accompanying body weight change of 2.9−3.83 kg); this degree of swelling will very likely cause a breakdown of underlying mathematical assumptions in our analysis. All monitoring sessions for the remaining eight neonates were included. Thus, we analyzed 22 monitoring sessions of the nine included neonates (Table 1, Supplementary Material Fig. S1). At our institution, centrifugal pumps are not used for infants; therefore, all included subjects were perfused with roller pumps.
Baseline hemodynamics and vital signs
Table 2 contains summary statistics of baseline hemodynamic measurements across the nine neonatal subjects (1−5 measurements per subject). Figure 2 shows their correlation with systemic measures. We observed high intrasubject variability in BFIo, compared to PFo, and MAPo, which suggests that these systemic parameters are poor surrogates of CBF (Table 2). Weak correlations between BFIo and PFo (R = − 0.45, p = 0.03) and between BFIo and MAPo (R = 0.49, p = 0.02), were found. Note also that we did not observe a significant correlation between MAPo and PFo (R = −0.24, p = 0.28) in this population. These weak and potentially spurious correlations are perhaps further testament to the complex interactions that can exist between ECMO and cardiac circuits and these circuits and the brain, as well as the significant intersubject and temporal variation in vasopressor therapy, shock state, etc. The intrasubject variability in BFIo could reflect variability within individual patients, e.g., due to changes in superficial tissue thickness. Similarly, StO2,o was not correlated with PFo (R = 0.11, p = 0.64) or with MAPo (R = 0.07, p = 0.77), and it was only marginally correlated with mixed systemic SvO2,o (R = 0.43, p = 0.057). Cerebral StO2,o was generally lower than systemic SvO2,o, which is consistent with the high metabolism of the brain, compared to the resting body, and other work,32 as well as the differences between cerebral and somatic vascular physiology. Finally, the correlations of BFIo and StO2,o with PPo were R = 0.328 (p = 0.136) and R = −0.08 (p = 0.745) respectively (not shown).
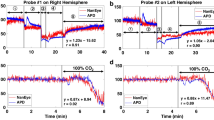
DCS-measured Blood Flow Index (BFI) vs. (a) mean arterial blood pressure (MAP) and (b) pump flow (PF, normalized by patient weight). (c) MAP is not well correlated to pump flow. Cerebral oxygenation (StO2) is poorly correlated to PF (d) and MAP (e); it is trending to a weak correlation with venous oxygen saturation (SvO2) (f). Pulse pressure (PPo) was correlated with MAP (g). Black circles designate subjects who expired on ECMO. Lines represent a linear best fit; R is Spearman’s correlation coefficient.
An important advantage of the FD-DOS technique is its ability to measure absolute optical properties. In the seven neonates with multiple measurement days, we observed an intrasubject temporal coefficient of variation (CV) in the tissue-reduced scattering coefficient of 0.26 (0.18, 0.35) (i.e., CV is the ratio of the standard deviation and the mean of μ′s,o at 785 nm for each patient across multiple monitoring days; intersubject median (IQR); also see Table 2). Since μ′s,o determines the optical path length in tissue, accurate values of μ′s,o are critical for quantification. By contrast, tissue absorption (μa) varied less (0.09 (0.04, 0.22)).
Functional systems scores and pediatric risk of mortality (III) scores, day of life, and day on ECMO were all compared to optical measurements, and no significant relationships were identified.
CA assessment during ECMO pump flow variation
Figure 3 shows exemplar temporal traces of Hbt, StO2, relative BFI, and relative MAP measurements obtained during ±20% PF changes in different neonates (#1, 2) on the first day of ECMO and of life. In these examples, Hbt and StO2 are insensitive to flow manipulations in both cases, while MAP and BFI data show divergent responses. These results suggest that baseline condition for subject 2 was hyperoxygenated, as hemoglobin saturation was consistent despite >10% decrease in blood flow. For subject 1, the DCSx index (95% CI) was −0.42 (−0.52, −0.31); generally, DCSx near zero or slightly negative are considered to reflect intact CA. For subject 2, the DCSx index of 0.71 (0.65, 0.77) suggests impaired CA (Pearson’s correlation coefficients between StO2 and MAP were −0.04 (−0.17, 0.09) and 0.21 (0.1, 0.32), respectively).
Across the subject population, we found that DCSx was not predicted by MAPo, PPo, or left cardiac dysfunction (Fig. 4). While not statistically significant, DCSx was lower in patients with better cardiac function measured by echo-cardiogram, suggesting CA is more robust in patients with healthier hearts.
Temporal variation in CA during ECMO
Temporal variation in CA during ECMO for individual subjects was substantial (i.e., a coefficient of variation of 0.86 (−0.32, 1.14); see Table 2), and larger than the temporal variation in systemic parameters (Table 2). We further present one longitudinal case example (Fig. 5) for the patient with the largest number of monitoring days (subject 7). The robustly positive DCSx measurements on days 1−3 suggest impaired CA. In addition, MAPo, PPo, PFo, and StO2,o all significantly increased during days 1−3. It is plausible that the increase in StO2,o reflects increased oxygen delivery to the brain arising from excessive blood flow due to the increase in MAPo. Conversely, on days 4 and 5, DCSx is noticeably closer to zero, signaling improved CA. Further, systemic arterial and venous saturations (SaO2,o and SvO2,o), between days 1−3 and 4−5 are not significantly different. Finally, the improved CA on days 4 and 5 was associated with higher PPo, a surrogate metric of improved cardiac function. The notion of improved cardiac function is also supported by the divergence between PPo and PFo on day 4, which suggests that the healing heart is taking over the work of providing perfusion. This patient was successfully weaned from ECMO. Examining all the measurements in the entire population, we do not see a significant trend in DCSx with time (not shown). The longitudinal results shown in Fig. 5 should be interpreted with caution, in part because the optical measurements were temporally sparse (1 per day) and limited number of total measurements.
Longitudinal baseline measurements of MAPo (a); PPo and PFo (b); StO2,o, SvO2,o, and SaO2,o (c); and the optical DCSx CA index (d) for patient #7, who survived ECMO. Error bars denote standard deviation (a, b, c) and the 95% CI (d). On days 1, 2, and 4, the MAPo, SaO2,o, and SvO2,o changed little; however, DCSx changed significantly.
Discussion
In this observational pilot study we introduced and demonstrated a scheme that utilizes diffuse optical technology to noninvasively assess CA (i.e., DCSx index), microvascular cerebral perfusion (i.e., BFI), and microvascular cerebral oxygenation (i.e., StO2) in neonates receiving ECMO. The optical measurements, which were performed at the bedside with minimal disruption to clinical care of the patient, varied substantially between individuals and with time (Table 2). These preliminary results, as well as previous work by our group11,30 and others,33 suggest these optical measurements may be well-suited for longitudinal monitoring in children. Future work is clearly needed to demonstrate the clinical utility of this scheme and the practicality of continuous monitoring in critically ill children.
For CA assessment, optical measurements of BFI changes were compared to corresponding MAP changes induced by PF manipulations (Fig. 3). Pilot data from the case examples demonstrate the scheme’s ability to track longitudinal improvement (Fig. 5) in an individual neonate during ECMO. By contrast, cardiac and circulatory parameters do not predict CA, i.e., intact or impaired as defined by DCSx measurements (Figs. 4, 5). Note, previous work has shown good agreement between DCS and Laser Doppler (LD) CBF measures25 and that LDx (a LD CA metric similar to DCSx) could accurately distinguish intact from impaired CA.34 This in turn suggests that the DCSx is comparable to LDx, measured invasively by LD, for determination of CA.
At clinically prescribed PFo, the BFIo, MAPo, and StO2,o levels were heterogeneous (Fig. 2); intrasubject variability in BFIo and CA were large compared to the variability of PFo and MAPo (Table 2). The impact of PFo on MAPo and ultimately, on cerebral blood flow, appears to be complex; among other factors, it depends on cardiac output and the fraction of necessary flow provided by the ECMO pump, and may also reflect brain injury acquired prior to ECMO initiation. In total, these results suggest that the easily measured systemic parameters, such as pump flow and mean arterial pressure, that are often used to characterize patient response are not always good surrogates for healthy cerebral physiology (i.e., adequate CBF or StO2). Future work is needed to confirm the prognostic value of longitudinal monitoring with this scheme.
Direct cerebral monitoring versus systemic surrogates
Current clinical protocols frequently rely on systemic variables such as MAP targets, urine output and skin temperature as surrogates of end-organ perfusion, including cerebral perfusion. This study demonstrates that these non-neurologic indicators of adequate oxygen delivery are not reliable surrogates of brain perfusion.35,36 We observed longitudinal changes in perfusion and CA that were not apparent from the systemic measurements (e.g., Fig. 5). These pilot results, in combination with the observed variability between absolute MAP, SaO2,o, and SvO2,o and optical measurements of the brain (Fig. 5), highlight the potential of diffuse optics for improving patient-specific CBF management during ECMO. Defining such CBF targets will clearly be a challenge, as has been reviewed in the context of neurosurgery,37 and will ultimately need to include both blood pressure and metabolic regulation. Note, quantitative cerebral StO2 measurements were generally lower than systemic SvO2 measurements (Fig. 2), which is indicative of higher cerebral oxygen extraction levels,32 as well as differences in vascular physiology. Indeed, our average measured StO2 across patients was 57%, which is lower than previously reported StO2 of 67% in 1-week-old healthy infants.33
Intriguingly, in this population BFIo was a factor ~2 lower, while StO2 was 8% higher, than previously reported presurgical values in ventilated neonates with congenital heart defects.27
Use of StO2 data to assess CA
Our preliminary findings indicate that using StO2 measurements alone to assess CA may be difficult to generalize. For example, the StO2 data do not distinguish between the two case examples presented in Fig. 3, while the BFI data suggest different states of CA. The origin of the differing trends between BFI and StO2 data in Fig. 3 is not known. From Fick’s model, a constant StO2 in the face of changing BFI suggests that cerebral oxygen metabolism changes with pump/heart-driven cerebral blood flow, which seems unlikely. Potentially, the high absolute StO2 levels in these two examples (i.e., 60−70%) reflect hyperperfusion, and the accumulation of a sizeable reservoir of dissolved oxygen in the tissue. Previous modeling work has shown that such conditions can substantially blunt the changes in oxygen extraction arising from changes in cerebral blood flow.38 Excessive CBF, however, may expose the brain to risk of bleeding. More work is needed to investigate the use of StO2 data for CA assessment in this population.
Intrasubject variability in optical tissue scattering
Intrasubject temporal variability in the tissue-reduced scattering coefficient measurements was ~30%. Similar variability in scattering was also recently reported in two neonates on ECMO.39 The variability in scattering could reflect variability in tissue water content caused by swelling/inflammation. Indeed, given one subject’s >30% increase in body weight relative to the prior day, the very low tissue scattering coefficient measurement (~1.5 cm−1 at 785 nm) on the second day likely indicated a large amount of brain/superficial tissue swelling. Subsequent monitoring sessions were excluded from our analysis, due to potential failure of the diffusion model of photon transport. Additionally, the swelling observed in the ECMO population pushes the skin and optical probe further from the brain. Independent measurements of tissue water content and swelling in future studies is needed to better understand the relationship between scattering and swelling.
Clinical NIRS monitors assume a value for tissue scattering to derive estimates of oxygen saturation22; errors in this estimation affect the accuracy of computed StO2. The large temporal variability in scattering observed here raises concern about conflation between scattering and oxygenation changes in NIRS monitoring during ECMO. Future investigation of the magnitude and distribution of this error is needed. In addition, since accurate calculation of the DCS BFI relies on accurate knowledge of tissue absorption and scattering,22 a hybrid frequency or time domain DOS + DCS approach is preferable to DCS alone for perfusion monitoring.
Limitations
This pilot study has many limitations. The patient population is heterogeneous, even within diagnosis. Post-ECMO neuroimaging showed a wide range of injury; our sample size and the limitations discussed below preclude drawing conclusions on the relationship between CA and the injury observed weeks after ECMO by MRI. In addition, the study had variation in the timing of ECMO initiation, severity of illness, total blood volume (volume status), and other clinical variables in these critically ill children. Moreover, since the present study is observational, we did not control for medications nor clinical interventions; additionally, our recruitment protocol may have excluded the most ill, least stable, children. Given limited resources, continuous 24-h monitoring was not practical. Instead, our measurements were acquired over ~1 h per day, scheduled as convenient for the family and clinical team, and thus each measurement had a large variation in measurement time with respect to the start of ECMO, etc. Therefore, the longitudinal data from a single subject presented in Fig. 5 should be interpreted with caution, e.g., since the ~1-h monitoring intervals may not be indicative of average hemodynamics across the day. Further, the precise reasons for the observed improvement in CA in Fig. 5 are not known. Our data were also collected at a relatively slow rate (~7 s per measurement), limiting our sensitivity to higher frequency autoregulatory mechanisms. Due to the small data set, we made a linear comparison of MAP to BFIo, rather than a more realistic piece-wise linear or sigmoidal curve.
Furthermore, in these experiments, data were collected only on the right side of the head. Children were cannulated via the great vessels in the right side of the neck; the left side of the head was therefore positioned towards the bed. Anchoring our probe to the left side of the head in this position was impractical and repositioning was not feasible due to danger of dislodging the cannulas. However, cannulation via the vessels on the right side of the neck may restrict blood flow more to the right than left side of the brain, as the right side is then perfused by collateral circulation through the circle of Willis, leaving the right side of the brain more vulnerable to ischemic injury. Future studies to identify potential hemispherical differences in Hbt, StO2, and CA are needed.
For the baseline measurements, we caution that the variability in BFIo also likely reflects variability in factors such as differences in the superficial tissue thickness and probe pressure against the head. Swelling, for example, may change the distance between the optical probe and the brain, which will affect the absolute BFI measurement. Note, however, the relative changes used for the CA measurements are more robust to many of these effects.
Conclusion
We carried out a pilot study that employed diffuse optical tools to continuously monitor cerebral hemodynamics and assess cerebrovascular autoregulation integrity in the intensive care unit during VA-ECMO. Given a lack of correlation between DCS-measured CBF and both PF and MAP, the data here present a strong argument for cerebral monitoring with individualization of end-organ targeted care. This argument is further reinforced by the substantial variability in measurements of cerebral hemodynamics and CA integrity across patients and with time. This variability was not predicted by systemic measurements. Cerebral monitoring with diffuse optics could, in principal, be used to drive ECMO care and improve the quality of survival in these critically ill neonates. The hybrid FD-DOS + DCS approach utilized in this study provided additional value compared to FD-DOS alone for assessment of CA, oxygen delivery, and metabolism. Looking forward, by determining these critical metrics of cerebral health, quantitative optical tools could permit goal-directed clinical interventions, e.g., setting of ECMO pump flow based on DCSx values.
References
Lin, N., Flibotte, J. & Licht, D. J. Neuromonitoring in the neonatal ECMO patient. Semin. Perinatol. 42, 111–121 (2018).
Lequier, L. Extracorporeal life support in pediatric and neonatal critical care: a review. J. Intensive Care Med. 19, 243–258 (2004).
Ijsselstijn, H. & van Heijst, A. F. Long-term outcome of children treated with neonatal extracorporeal membrane oxygenation: increasing problems with increasing age. Semin. Perinatol. 38, 114–121 (2014).
Bembea, M. M. et al. Neuromonitoring during extracorporeal membrane oxygenation: a systematic review of the literature. Pediatr. Crit. Care Med. 16, 558–564 (2015).
Lee, J. K. et al. A pilot study of cerebrovascular reactivity autoregulation after pediatric cardiac arrest. Resuscitation 85, 1387–1393 (2014).
Papademetriou, M. et al. Wavelet cross-correlation to investigate regional variations in cerebral oxygenation in infants supported on extracorporeal membrane oxygenation. Oxyg. Transp. Tissue XXXIV 765, 203–209 (2013).
Van Heijst, A. et al. Oxygenation and hemodynamics in left and right cerebral hemispheres during induction of veno-arterial extracorporeal membrane oxygenation. J. Pediatrics 144, 223 (2004).
Tian, F. et al. Impairment of cerebral autoregulation in pediatric extracorporeal membrane oxygenation associated with neuroimaging abnormalities. Neurophotonics 4, 041410 (2017).
Zweifel, C., Dias, C., Smielewski, P. & Czosnyka, M. Continuous time-domain monitoring of cerebral autoregulation in neurocritical care. Med. Eng. Phys. 36, 638–645 (2014).
Stockwell, J. A. et al. Cerebral blood flow and carbon dioxide reactivity in neonates during venoarterial extracorporeal life support. Crit. Care Med. 24, 155–162 (1996).
Lynch, J. M. et al. Preoperative cerebral hemodynamics from birth to surgery in neonates with critical congenital heart disease. J. Thorac. Cardiovasc. Surg. 156, 1657–1664 (2018).
Diop, M. et al. Development of a combined broadband near-infrared and diffusion correlation system for monitoring cerebral blood flow and oxidative metabolism in preterm infants. Biomed. Opt. Express 6, 3907–3918 (2015).
Willie, C. K., Tzeng, Y. C., Fisher, J. A. & Ainslie, P. N. Integrative regulation of human brain blood flow. J. Physiol. 592, 841–859 (2014).
Czosnyka, M. et al. Monitoring of cerebrovascular autoregulation: facts, myths, and missing links. Neurocrit. Care 10, 373–386 (2009).
Tzeng, Y. C. & Ainslie, P. N. Blood pressure regulation IX: cerebral autoregulation under blood pressure challenges. Eur. J. Appl. Physiol. 114, 545–559 (2014).
Lassen, N. A. Cerebral blood flow and oxygen consumption in man. Physiol. Rev. 39, 183–238 (1959).
Short, B. L., Walker, L. K., Bender, K. S. & Traystman, R. J. Impairment of cerebral autoregulation during extracorporeal membrane oxygenation in newborn lambs. Pediatr. Res. 33, 289–294 (1993).
Papademetriou, M. D. et al. Optical topography to measure variations in regional cerebral oxygenation in an infant supported on veno-arterial extra-corporeal membrane oxygenation. Adv Exp Med Biol 737, 71–76 (2012).
Short, B. L. The effect of extracorporeal life support on the brain: a focus on ECMO. Semin. Perinatol. 29, 45–50 (2005).
Rollins, M. D. et al. Utility of neuroradiographic imaging in predicting outcomes after neonatal extracorporeal membrane oxygenation. J. Pediatr. Surg. 47, 76–80 (2012).
Taccone, F. S. et al. Cerebral oximetry during extracorporeal cardiopulmonary resuscitation. Crit. Care 17, 409 (2013).
Durduran, T., Choe, R., Baker, W. B. & Yodh, A. G. Diffuse Optics for Tissue Monitoring and Tomography. Rep. Prog. Phys. 73, 076701 (2010).
Jenny, C. et al. Reproducibility of cerebral tissue oxygen saturation measurements by near-infrared spectroscopy in newborn infants. J. Biomed. Opt. 16, 097004–097004 (2011).
Schneider, A. et al. Comparison of 4 near-infrared spectroscopy devices show that they are only suitable for monitoring cerebral oxygenation trends in preterm infants. Acta Paediatr. 103, 934–938 (2014).
Mesquita, R. C. et al. Direct measurement of tissue blood flow and metabolism with diffuse optics. Philos. Trans. R. Soc. A-Math. Phys. Eng. Sci. 369, 4390–4406 (2011).
Boas, D. A. & Yodh, A. G. Spatially varying dynamical properties of turbid media probed with diffusing temporal light correlation. J. Optical Soc. Am. A-Opt. Image Sci. Vis. 14, 192–215 (1997).
Jain, V. et al. Cerebral oxygen metabolism in neonates with congenital heart disease quantified by MRI and Optics. JCBFM 34, 380–388 (2014).
Pollack, M. M. et al. Functional Status Scale: new pediatric outcome measure. Pediatrics 124, e18–e28 (2009).
Wang, J. N., Wu, J. M. & Chen, Y. J. Validity of the updated pediatric risk of mortality score (PRISM III) in predicting the probability of mortality in a pediatric intensive care unit. Acta Paediatr. Taiwan 42, 333–337 (2001).
Buckley, E. M. et al. Early postoperative changes in cerebral oxygen metabolism following neonatal cardiac surgery: effects of surgical duration. J. Thorac. Cardiovasc. Surg. 145, 196–205 (2013).
Fantini, S. et al. Non-invasive optical monitoring of the newborn piglet brain using continuous-wave and frequency-domain spectroscopy. Phys. Med. Biol. 44, 1543 (1999).
Lynch, J. M. et al. Validation of optically measured cerebral venous oxygenation saturation in humans. Acad. Radio. 21, 162–167 (2014).
Franceschini, M. A. et al. Assessment of infant brain development with frequency-domain near-infrared spectroscopy. Pediatr. Res. 61, 546–551 (2007).
Brady, K. M. et al. Continuous time-domain analysis of cerebrovascular autoregulation using near-infrared spectroscopy. Stroke 38, 2818–2825 (2007).
Kato, R. & Pinsky, M. R. Personalizing blood pressure management in septic shock. Ann. Intensive Care 5, 41 (2015).
Rhee, C. J. et al. Elevated diastolic closing margin is associated with intraventricular hemorrhage in premature infants. J. Pediatr. 174, 52–56 (2016).
Steiner, L. A. & Czosnyka, M. Should we measure cerebral blood flow in head-injured patients? Br. J. Neurosurg. 16, 429–439 (2002).
Valabregue, R. et al. Relation between cerebral blood flow and metabolism explained by a model of oxygen exchange. J. Cereb. Blood Flow Metab. 23, 536–545 (2003).
Tian, F. et al. Regional cerebral abnormalities measured by frequency-domain near-infrared spectroscopy in pediatric patients during extracorporeal membrane oxygenation. J. ASAIO 63, e52–e59 (2017).
Acknowledgements
The authors thank the study participants and their families. We also thank Dr. Ashwin Parthasarathy, Dr. Turgut Durduran, Dr. Robert Sutton, Dr. Robert Levy, and Dr. Jeffery Cochran, for helpful discussions; Dr. Brian White for clinical insights; Kenneth Abramson for technical assistance; and the CHOP ECMO team, Madeline Winters, John Newland, and Kaitlin Griffith, for assistance in making measurements. This study was supported by the National Institutes of Health (NIH R01-NS072338, T32-HL007915, R01-NS060653, F31-HD085731, R01-HL141386, & P41-EB015893), DoD CDMRP W81XWH1810607, the Thrasher Foundation, Institute of International Education, and philanthropic support from the June and Steve Wolfson Family Foundation and the Raymond Family ECMO Fund.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: D.R.B., W.B.B., C.D.M., T.S.K., J.M.L., A.L.M., G.D.P.-T., E.M.B., M.J., T.B., K.M.-B., A.G.Y., D.J.L. Drafting the article or revising it critically for important intellectual content: D.R.B., W.B.B., J.C., C.D.M., T.S.K., A.G.Y., T.J.K., D.J.L. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
D.R.B., W.B.B., A.G.Y., D.J.L. have patents and patent applications related to diffuse correlation and optical spectroscopies. These patents have not been licensed and the authors receive no revenue.
Patient consent
Under a protocol approved by the Institutional Review Board of the Children’s Hospital of Philadelphia, informed consent was obtained by a physician researcher from each subject’s parents.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Busch, D.R., Baker, W.B., Mavroudis, C.D. et al. Noninvasive optical measurement of microvascular cerebral hemodynamics and autoregulation in the neonatal ECMO patient. Pediatr Res 88, 925–933 (2020). https://doi.org/10.1038/s41390-020-0841-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0841-6
This article is cited by
-
Advanced Neuromonitoring Modalities on the Horizon: Detection and Management of Acute Brain Injury in Children
Neurocritical Care (2023)
-
Stroke in pediatric ECMO: a target for prevention and improvement
Pediatric Research (2022)
-
Effects of circulatory arrest and cardiopulmonary bypass on cerebral autoregulation in neonatal swine
Pediatric Research (2022)
-
Preliminary Research: Application of Non-Invasive Measure of Cytochrome c Oxidase Redox States and Mitochondrial Function in a Porcine Model of Carbon Monoxide Poisoning
Journal of Medical Toxicology (2022)
-
Impact of Arterial Carbon Dioxide and Oxygen Content on Cerebral Autoregulation Monitoring Among Children Supported by ECMO
Neurocritical Care (2021)