Abstract
Background
Pomalidomide, an immunomodulatory drug, was investigated for pediatric brain tumors. The objectives of this analysis were to characterize the PK of pomalidomide and to examine exposure–response relationship in pediatric patients with recurrent or progressive primary brain tumors.
Methods
Nonlinear mixed effects modeling was employed in developing a population PK model of pomalidomide using a total of 343 concentrations from 70 patients. Logistic regression models were used for exposure–response analyses.
Results
The PK of pomalidomide was adequately described with a one compartment model with first-order absorption and elimination. Body surface area (BSA) was identified as a statistically significant covariate of apparent clearance and volume of distribution; however, the impact of BSA on exposure parameters was not deemed clinically relevant. Pomalidomide exposure was not associated with higher probabilities of treatment-emergent adverse events or pomalidomide dose interruptions during Cycle 1. Covariates such as BSA, weight, sex, age, and race had no significant effect on safety endpoints. The PK of pomalidomide in pediatric patients with brain tumors was generally consistent with that in adult patients with multiple myeloma after adjustment for BSA.
Conclusions
This is the first study to characterize PK of pomalidomide in pediatric patients, which supports BSA-based dosing for pediatric patients.
Impact
-
This is the first study to characterize PK of pomalidomide in pediatric patients, which supports BSA-based dosing for pediatric patients.
-
There is no significant pomalidomide PK difference between adults and pediatrics.
-
Pomalidomide exposure was not associated with higher probabilities of treatment-emergent adverse event or pomalidomide dose interruptions during Cycle 1.
Similar content being viewed by others
Introduction
Pomalidomide (CC-4047), an analog of thalidomide, is a novel drug in the class of drugs known as immunomodulatory compounds. Pomalidomide has a pleiotropic mechanism of action, including immunomodulatory, anti-inflammatory, anti-angiogenic, and antitumor activity.1,2 Pomalidomide in combination with dexamethasone was approved in the United States (US) and the European Union (EU) for the treatment of adult patients with multiple myeloma who have received at least two prior therapies including lenalidomide and a proteasome inhibitor (bortezomib in EU) and have demonstrated disease progression on or within 60 days of completion of the last therapy.3,4 Pomalidomide in combination with bortezomib and dexamethasone was also approved in EU for the treatment of adult patients with multiple myeloma who have received at least one prior treatment regimen including lenalidomide.4 In addition, pomalidomide was recently approved in the US for the treatment of adult patients with acquired immunodeficiency syndrome-related Kaposi sarcoma after failure of highly active antiretroviral therapy or in patients with Kaposi sarcoma who are human immunodeficiency virus-negative under accelerated approval based on overall response rate.3
Central nervous system (CNS) tumors (including brain and spinal cord) are the most common solid tumors among children and account for up to 25% of all childhood cancer cases.5 Although the prognosis for pediatric patients with brain tumors has improved over the past few decades with diverse intensive therapeutic modalities such as neurosurgery, chemotherapy, and radiation, many brain tumors remain difficult to treat and are associated with a poor prognosis.6,7 Pomalidomide was considered to be suitable to treat pediatric CNS tumors for various reasons. First, pomalidomide is an agent that possesses multiple mechanisms of action, including anti-angiogenesis and alterations in inflammatory cytokines, which are important targets in CNS tumor propagation.8,9 Second, preclinical evaluation showed that pomalidomide crosses the blood–brain barrier with unbound brain area under the concentration–time curve (AUC) to blood AUC ratio of 0.39 and had significant therapeutic activity against CNS lymphoma.10 There are clinical reports demonstrating effectiveness of pomalidomide against myelomatous meningitis, further supporting CNS penetration and efficacy within the CNS.11,12 In addition, lenalidomide, another thalidomide analog, was well tolerated in children with brain and solid tumors.13,14
Two clinical studies were conducted to evaluate safety, pharmacokinetics (PK), and/or efficacy of pomalidomide in children and young adults with recurrent or progressive brain tumors.15,16 In this study, population PK and exposure–response analyses were performed to characterize the PK variability of pomalidomide and to examine exposure–response relationship in children and young adults with recurrent or progressive primary brain tumor. This is the first study to characterize PK of pomalidomide in pediatric subjects.
Materials and methods
Clinical study data
Subjects from Studies PBTC-043 and CC-4047-BRN-001 were included in population PK and exposure–response analyses. Study PBTC-043 (NCT02415153) was a multicenter, single-arm, open-label, Phase 1 dose escalation trial of pomalidomide for children with recurrent, progressive, or refractory CNS tumors to determine the maximum tolerated dose (MTD) or recommended Phase 2 dose, to evaluate toxicities, and to characterize the PK of pomalidomide in a pediatric population. Twenty-nine subjects were included in different cohorts assigned to various escalating doses (1.9, 2.6, or 3.4 mg/m2).16 Study CC-4047-BRN-001 (NCT03257631) was a Phase 2 multicenter, open-label, parallel-group study to assess the efficacy, safety, and tolerability of pomalidomide in children and young adults aged 1–<21 years with recurrent or progressive primary brain tumors after at least one prior standard therapy. Fifty-three subjects with one of the four primary brain tumor types (high-grade glioma, medulloblastoma, ependymoma, and diffuse intrinsic pontine glioma) were enrolled. The starting dose was 2.6 mg/m2/day, which was determined as the MTD in Study PBTC-043.15 In both studies, subjects received pomalidomide on Days 1–21, followed by a 7-day rest period, of each 28-day treatment cycle. These studies were conducted in accordance with the Declaration of Helsinki and the International Council for Harmonisation Guideline for Good Clinical Practice (ICH E6). Written informed consent/assent was obtained from all subjects or parents/guardians prior to enrollment into the studies.
PK sampling and bioanalytical methods
Blood samples for measurement of plasma pomalidomide concentrations were collected at predose and 0.5, 1, 2, 4, 8, and 24 h postdose on Cycle 1 Day 1 in Study PBTC-043 and predose and 2 h postdose on Cycle 1 Days 8 and 15 in Study CC-4047-BRN-001. Pomalidomide concentrations in plasma were determined using a validated high-performance liquid chromatography method with tandem mass spectrometric detection. The lower limit of quantification was 0.25 ng/mL.17
Structural population PK model
The population PK analysis was performed using NONMEM Version 7.3 with the first-order conditional estimation and the INTERACTION option (ICON Development Solutions, Ellicott City, MD). Perl-speaks-NONMEM (PsN Version 4.6.0) was used to evaluate the PK model and the results were further analyzed by R (Version 3.5.1).
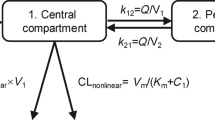
Selection of the most appropriate model was based on prior knowledge of pomalidomide disposition, graphical examination of the raw data, and criteria for assessment of model adequacy. According to prior knowledge, pomalidomide was best described in patients with multiple myeloma by a one- or two-compartment model, as supported by the PK sampling frequency, with first-order absorption and a lag time.17,18 PK linearity was examined by testing a model in which clearance (CL/F) was described by a combination of linear and nonlinear (Michaelis–Menten) terms. Assuming a log-normal distribution for interindividual variability (IIV) in PK parameters, IIV was modeled using an exponential random-effect model to maintain positive PK parameters. Assuming a log-normal distribution of residual variability (RV) in concentration data, RV was modeled using an additive error model after the concentration was log-transformed to stabilize the RV.
Model evaluation and selection were based on pertinent graphical representations of goodness of fit, scientific plausibility, and the minimization of −2 × log-likelihood, which was presented as the objective function value (OFV). A decrease in the OFV of 3.84 (p = 0.05) was considered significant to include a parameter in the model.
Covariate analysis
Covariates that may explain variability in the disposition of pomalidomide were evaluated. According to the biological plausibility, the following factors were explored as covariates for their potential to influence pomalidomide PK parameters: age, body surface area (BSA), body mass index, weight, race, and sex. Shrinkage was calculated for the base model to determine whether the PK parameter estimates are reliable. Empirical Bayesian estimates of the parameters were generated from the base model for each subject. Data visualization was used to examine the relationship between potential covariates and subject-level PK parameters. These plots were evaluated for observable trends and assisted in determining the covariates to be tested by NONMEM and the functional form of the relationship between the parameter and the covariate. Generally, the median (continuous) or most prevalent (categorical) covariate values were used as the reference population during covariate modeling. Potential covariates identified in the graphical analyses were formally evaluated within NONMEM using a stepwise forward additive approach using a p value of 0.01 (ΔOFV = −6.63) and a backward elimination using a p value of 0.001 (ΔOFV = −10.83).19
Model performance
The performance of the final population PK model of pomalidomide was evaluated with nonparametric bootstrap resampling and prediction-corrected visual predictive check (VPC).20 The bootstrap method was used to assess the reliability of the model parameter estimates and to select the statistically and clinically important covariates. For this purpose, new datasets were generated using resampling with replacement. The population PK model was re-fitted to the bootstrapped new datasets, and the parameters of the model were then estimated from each of the new datasets. A thousand bootstrap replicates were performed. This resulted in a series of model fits, each with its own set of parameters. The median and non-parametric 95% confidence interval (CI) of these parameters were determined. The prediction-corrected VPC was used to assess how well the current model describes the observed data. A thousand simulated datasets with the same structure as the original dataset were created using the fixed and random parameters of the model. The 95% prediction intervals for the 5th, 50th, and 95th percentiles of simulated data were compared to the corresponding observed data. Binning of observations around PK sample times were done to ensure sufficient density of observations.
Generation of subject-specific exposure measures
Empirical individual Bayesian estimates of PK parameters were generated using the final population PK model. With these individual parameter estimates, the following measures of pomalidomide exposure were computed for each subject and used in exposure–safety analysis: AUC at steady state (AUCss), maximum concentration at steady state (Cmax,ss), and minimum concentration at steady state (Cmin,ss).
Exposure–response analyses
The exposure–efficacy analysis was not performed due to the limited number of responders in both studies. The exposure–safety analysis of treatment-emergent adverse event (TEAE, any grades) was conducted for subjects who had both post hoc estimated pomalidomide exposure data from the final population PK model and safety data and TEAE in Studies PBTC-043 and CC-4047-BRN-001. TEAEs were defined as any adverse events occurring or worsening on or after the first dose of pomalidomide and within 28 days after the last pomalidomide administration date. For the exposure–safety analysis of pomalidomide dose interruptions during Cycle 1, only subjects from Study CC-4047-BRN-001 were included because these safety endpoints were not applicable to Study PBTC-043, the dose-escalation study. The pomalidomide steady-state exposure parameters (e.g., AUCss, Cmax.ss, and Cmin,ss) were used as exposure endpoints in exposure–safety analyses. Logistic regression analyses were conducted to develop a model describing the relationship between pomalidomide exposure and the probability of experiencing safety events after adjusting for effect of significant covariates. Development of the model consisted of three stages. In the first stage, a base model was developed to assess the existence of the relationship between pomalidomide exposure and the probability of experiencing a safety event. The effect of pomalidomide exposure on safety endpoints was evaluated using linear functions. In the second stage, the impact of covariates on the probability of achieving a safety endpoint was examined by adding the candidate factors one by one to the base model and then including all potential covariates in a full model.21 In the third stage, the final model was derived from the full model by dropping non-statistically significant covariates (a p value of 0.05). The exposure parameter was retained in the final model regardless of its statistical significance and its clinical relevance was interpreted, as appropriate. The results of the exposure–safety analysis were presented graphically by overlaying the observed safety event frequency and its 95% CIs within each exposure group with the model-predicted mean probability and its 95% CIs.
Results
Summary of analysis dataset
PK samples from 70 subjects included in Studies PBTC-043 and CC-4047-BRN-001 were used for the population PK analysis of pomalidomide. Of the 382 samples collected, a total of 343 samples were included in the population PK analysis. Of the 39 samples excluded from the population PK analysis, 37 (37/382 = 9.7%) samples had concentrations below the limit of quantification (BLQ), with 29 BLQ prior to the first dose and 8 BLQ observed after the first dose was taken. Of the remaining excluded samples, 2 samples (2/382 = 0.5%) had missing dosing information prior to the PK concentration. The demographics of subjects included in the population PK analysis are shown in Table 1. The PK population included 39 male (55.7%) and 31 female (44.3%) subjects mainly of Caucasian origin (77.1%). Median (range) age and BSA were 12 years (4–20 years) and 1.33 m2 (0.690–2.24 m2), respectively, in the PK population.
Structural population PK model
A population PK analysis was performed based on rich and sparse samples collected in Studies PBTC-043 and CC-4047-BRN-001, respectively. The starting point was a one-compartment model with first-order absorption and elimination based on the observed concentration–time profile. The one-compartment model was preferred over the two-compartment model due to better minimization and more reliable parameter estimates, which is consistent with the PK sampling schedule from Study PBTC-043. The one-compartment linear model was preferred over a nonlinear model across the overall dose range (1.9, 2.6, and 3.4 mg/m2), in which pomalidomide elimination was described by a combination of linear and nonlinear (Michaelis–Menten) terms. In addition, the nonlinear model suffered from poor convergence.
According to goodness-of-fit and statistical criteria, the one-compartment model with first-order absorption and elimination and absorption lag time was selected as the structural model. Log-transformation of concentrations allowed better estimates of parameters and results from the analysis were more stable. IIV on apparent clearance (CL/F) and first-order absorption rate constant (Ka) was modeled and estimated with acceptable shrinkage (13.5 and 26.5%, respectively). IIV on apparent volume of distribution (V/F) was not modeled in the structural model because inclusion of IIV on V/F resulted in an unreliable V/F estimation associated with a high relative standard error. Moreover, the model with IIV on V/F became unstable and very sensitive to initial values.
Overall, observed concentrations of pomalidomide were adequately described, with the population- and individual-predicted concentrations exhibiting close agreement with the observed data. Furthermore, the distribution of conditional weighted residuals (CWRES) was homogeneously and evenly distributed around zero across the population-predicted concentrations or sampling times, suggesting no obvious bias in the predictions of high and low concentrations of pomalidomide.
Covariate analysis
A stepwise covariate analysis was performed to identify sources of variability in PK parameters of pomalidomide. The effect of BSA on V/F resulted in the greatest decrease in OFV as part of the first step of the analysis (ΔOFV = −27.437). In the second step, the effect of BSA on CL/F resulted in the greatest decrease in OFV (ΔOFV = −22.169). During the backward elimination, none of the covariates were removed. After including BSA in the model, there was no effect of age, sex, or race. The equations of the final covariate models are:
The inclusion of BSA in the model explained the IIV in CL/F and V/F.
Using results of the bootstrap, the effect of BSA on CL/F, V/F, and pomalidomide exposure (AUCss and Cmax,ss) is presented in Fig. 1. The CL/F and V/F of pomalidomide were dependent on BSA. The exponent for the effect of BSA on CL/F and V/F suggests a higher CL/F or V/F of pomalidomide in subjects with larger BSA. The median CL/F in subjects with BSA of 0.8 and 2 m2, which represents the 5th and 95th quantiles of BSA in the population, are 41% lower and 53% higher, respectively, than CL/F in a subject with BSA of 1.33 m2. The median V/F in subjects with BSA of 0.8 and 2 m2 are 55% lower and 86% higher, respectively, than V/F in a subject with BSA of 1.33 m2. The effect of BSA on pomalidomide exposure was investigated at the dose of 2.6 mg/m2, and no clinically significant difference (<25%) was expected in the median exposure level between the 5th or 95th quantile of BSA and the reference value.
(a) apparent clearance, (b) apparent volume of distribution, (c) area under the concentration–time curve at steady state, and (d) maximum concentration at steady state. The values for body surface area represent 5th, 50th, and 95th quantiles. The reference corresponds to a subject with body surface area of 1.33 m2. For exposure parameters, the clinically relevant effect is a change that would likely warrant a ±50% change in the dose. AUCss area under the concentration–time curve at steady state for a dose of 2.6 mg/m2, CI confidence interval, CL/F apparent clearance, Cmax,ss maximum concentration at steady state for a dose of 2.6 mg/m2, V/F apparent volume of distribution.
Final population PK model
Typical values of PK parameters derived with the final PK model of pomalidomide and bootstrap are presented in Table 2. The typical values of CL/F, V/F, Ka, and lag time of pomalidomide were 3.94 L/h, 43.0 L, 1.45 h−1 and 0.454 h, respectively. The terminal elimination half-life of pomalidomide was 7.33 h. The rate constant of pomalidomide absorption was 1.45 h−1, which corresponds to an absorption half-life of 0.478 h. The RV on predicted concentrations was 0.627 (CV% = 69.4%). Diagnostic plots of the final population PK model are presented in Fig. 2. Overall, individual-predicted concentrations of pomalidomide were adequately fitted with the final population PK model. Population- and individual-predicted concentrations of pomalidomide from the final model suggest good agreement with the observed data. Concentration values were evenly distributed around the line of identity. Weighted residuals were evenly distributed around 0, with only one observation associated with |CWRES | > 4.
The final population PK model of pomalidomide was evaluated using a bootstrap resampling method. A total of 1000 bootstrap runs were performed using the population PK model, and 995 runs were successfully minimized. The final model estimates and the bootstrap median estimates were similar for the fixed-effect parameters and the random-effect parameters (Table 2). These results suggested that the final model is robust and stable. The final population PK model of pomalidomide was also evaluated using prediction-corrected VPC with 1000 simulations (Fig. 3). The 5th, 50th, and 95th percentiles of the observed concentration data at each time point were generally contained within the respective 95% CI of the simulated data. There was a good agreement in the time course and central tendency between distributions of observed and simulated concentration data, with no obvious bias. Taken together, pomalidomide concentrations were well characterized by the final population PK model and enabled the use of the model to predict pomalidomide exposure for exposure–safety analysis.
(a) Study PBTC-043 and (b) Study CC-4047-BRN-001. Black dots represent observed data, and black lines represent observed 5th, 50th, and 95th percentiles. Solid lines represent the 5th (red), 50th (blue), and 95th (red) percentiles of the simulated data. Shaded areas represent 95% confidence intervals about the 5th, 50th, and 95th percentiles for the corresponding simulated data.
Bayesian PK and exposure parameters were estimated from the final population PK model for each subject. The descriptive statistics of these parameters were summarized in Supplementary Table S1.
Exposure–safety analyses
The exposure–safety analysis for TEAEs indicated that exposure parameters of pomalidomide were not associated with higher probabilities of TEAE (AUCss: Fig. 4a). Exposure–safety analysis of pomalidomide dose interruptions during Cycle 1 indicated that exposure parameters of pomalidomide were not associated with higher probabilities of pomalidomide dose interruption during Cycle 1 (AUCss: Fig. 4b). Covariates such as BSA, weight, sex, age, and race had no significant effect on safety endpoints.
Discussion
This is the first population PK study of pomalidomide in pediatric subjects. Pomalidomide concentration–time data from doses of 1.9 to 3.4 mg/m2 administered daily to children and young adult subjects with recurrent, progressive, or refractory CNS tumors from Phase 1 study (PBTC-043) and with recurrent or progressive brain tumors in Phase 2 study (CC-4047-BRN-001) were adequately described by a one-compartment model with first-order absorption and elimination. The typical values of CL/F and V/F of pomalidomide were 3.94 L/h and 43.0 L, respectively. The terminal elimination half-life of pomalidomide was 7.33 h. BSA was identified as the only statistically significant covariate of CL/F and V/F.
Both CL/F and V/F were found to increase with increasing BSA according to an allometric relationship, with exponent values of 1.04 and 1.54, respectively. The median CL/F in subjects with BSA of 0.8 and 2 m2 are 41% lower and 53% higher, respectively, than CL/F in a subject with BSA of 1.33 m2. The median V/F in subjects with BSA of 0.8 and 2 m2 are 55% lower and 86% higher, respectively, than V/F in a subject with BSA of 1.33 m2. At the dose of 2.6 mg/m2, no clinically significant difference (<25%) was expected in the median exposure level between the 5th or 95th quantile of BSA and the reference value. The BSA effect on exposure is unlikely to affect safety given the wide pomalidomide exposure range at the clinical dose of 2.6 mg/m2 and the lack of exposure–safety relationship. Thus dose adjustment in patients with extreme BSA values is not necessary. Other factors such as age, sex, and race had no effect on pomalidomide PK.
Exposure parameters of pomalidomide were not associated with higher probabilities of TEAEs or pomalidomide dose interruptions during Cycle 1, suggesting that pomalidomide was safe at the tested exposure range. Covariates such as BSA, weight, sex, age, and race had no significant effect on TEAE. The exposure–safety analysis for pomalidomide dose reductions during the treatment period was not performed as only 2 subjects (2/41 = 5%) in Study CC-4047-BRN-001 had dose reductions. The exposure–efficacy analysis was not performed due to the limited number of responders in both studies. For Study PBTC-043, out of the 29 treated subjects, no patients experienced complete response or partial response, 2 (6.9%) patients experienced long-term stable disease lasting ≥6 cycles.16 For Study CC-4047-BRN-001, out of the 46 subjects who were evaluable for the primary endpoint, only 3 (6.5%) subjects achieved objective response or long-term stable disease.15
The population PK model of pomalidomide in pediatric patients with brain tumors was generally consistent with that in adult patients with multiple myeloma.18 Both population PK models were a one-compartment model with first-order absorption and elimination with the effects of BSA on both CL/F and V/F. At the median BSA of 1.33 m2 in pediatric patients with recurrent or progressive brain tumors, both pediatric and adult models share comparable values of CL/F (3.94 vs. 4.01 L) and V/F (43.0 vs. 53.2 L). These findings suggest no apparent PK difference between pediatric and adult patients for a BSA-based dosing. The recommended Phase 2 dose of pomalidomide in children with recurrent brain tumors, 2.6 mg/m2 once daily for 21 consecutive days of a 28-day cycle, is comparable to the Food and Drug Administration-approved adult dose of pomalidomide (4 mg once daily for 21 consecutive days of a 28-day cycle), assuming an average adult BSA of 1.7 m2 (4 mg/1.7 m2 = 2.35 mg/m2). Pomalidomide PK profile was simulated at both 4 mg once daily (fixed dosing) and 2.6 mg/m2 once daily (BSA-based dosing) using 70 patients in the population PK analysis. Simulation results demonstrated that BSA-based dosing reduced interindividual variation in pomalidomide exposure (Supplementary Fig. S1), which supports BSA-based dosing for pediatric patients.
Pomalidomide showed moderate distribution in the brain in mice.10 Pomalidomide is a substrate for P-glycoprotein (P-gp),22 which is expressed in the luminal membrane of the blood–brain barrier and the small intestine and in the apical membranes of excretory cells, such as hepatocytes and kidney proximal tubule epithelia.23 Coadministration of pomalidomide with the strong P-gp and Cytochrome P450 3A inhibitor ketoconazole had no clinically relevant effect on plasma pomalidomide exposure in healthy subjects,22 suggesting no significant contribution of P-gp to absorption and excretion of pomalidomide. However, the contribution of P-gp to limiting entry of pomalidomide into the CNS is unknown.
In summary, pomalidomide concentration–time profiles were adequately described with a one-compartment PK model with first-order absorption and elimination. Except for BSA, none of the tested covariates including age, sex, and race had effect on pomalidomide PK. Although BSA was identified as a statistically significant covariate of pomalidomide CL/F and V/F, the impact of BSA on exposure parameters was not deemed clinically relevant. There is no significant pomalidomide PK difference between adults and pediatrics. Pomalidomide exposure was not associated with higher probabilities of TEAE or pomalidomide dose interruptions during Cycle 1.
References
Lacy, M. Q. & McCurdy, A. R. Pomalidomide. Blood 122, 2305–2309 (2013).
Mark, T. M., Coleman, M. & Niesvizky, R. Preclinical and clinical results with pomalidomide in the treatment of relapsed/refractory multiple myeloma. Leuk. Res. 38, 517–524 (2014).
Celgene Corporation. POMALYST (Pomalidomide) label. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/204026s027lbl.pdf (2020).
Celgene Ltd. IMNOVID (Pomalidomide) summary of product characteristics. https://www.medicines.org.uk/emc/product/1262/smpc#gref (2019).
Fleming, A. J. & Chi, S. N. Brain tumors in children. Curr. Probl. Pediatr. Adolesc. Health Care 42, 80–103 (2012).
Grondin, R. T., Scott, R. M. & Smith, E. R. Pediatric brain tumors. Adv. Pediatr. 56, 249–269 (2009).
Hummel, T. R., Chow, L. M., Fouladi, M. & Franz, D. Pharmacotherapeutic management of pediatric gliomas: current and upcoming strategies. Paediatr. Drugs 15, 29–42 (2013).
Jain, R. K. et al. Angiogenesis in brain tumours. Nat. Rev. Neurosci. 8, 610–622 (2007).
Sie, M., den Dunnen, W. F., Hoving, E. W. & de Bont, E. S. Anti-angiogenic therapy in pediatric brain tumors: an effective strategy? Crit. Rev. Oncol. Hematol. 89, 418–432 (2014).
Li, Z. et al. Pomalidomide shows significant therapeutic activity against CNS lymphoma with a major impact on the tumor microenvironment in murine models. PLoS ONE 8, e71754 (2013).
Gertz, M. A. Pomalidomide and myeloma meningitis. Leuk. Lymphoma 54, 681–682 (2013).
Mussetti, A., Dalto, S. & Montefusco, V. Effective treatment of pomalidomide in central nervous system myelomatosis. Leuk. Lymphoma 54, 864–866 (2013).
Berg, S. L. et al. Safety, pharmacokinetics, and immunomodulatory effects of lenalidomide in children and adolescents with relapsed/refractory solid tumors or myelodysplastic syndrome: a Children’s Oncology Group Phase I Consortium report. J. Clin. Oncol. 29, 316–323 (2011).
Warren, K. E. et al. Phase I trial of lenalidomide in pediatric patients with recurrent, refractory, or progressive primary CNS tumors: Pediatric Brain Tumor Consortium study PBTC-018. J. Clin. Oncol. 29, 324–329 (2011).
Fangusaro, J. R. et al. A phase II clinical study of pomalidomide (CC-4047) monotherapy for children and young adults with recurrent or progressive primary brain tumors. J. Clin. Oncol. 37, 10035–10035 (2017).
Fangusaro, J. R. et al. A phase I trial of pomalidomide for children with recurrent, progressive/refractory central nervous system (CNS) tumors: a pediatric brain tumor. J. Clin. Oncol. 35, 10543–10543 (2017).
Li, Y. et al. Population pharmacokinetics of pomalidomide. J. Clin. Pharmacol. 55, 563–572 (2015).
Li Y., Kassir N., Wang X., Palmisano M. & Zhou S. Population pharmacokinetics and exposure response analysis of pomalidomide in subjects with relapsed or refractory multiple myeloma from the novel combination treatment of pomalidomide, bortezomib, and low-dose dexamethasone. J. Clin. Pharmacol. 60, 1061–1075 (2020).
Jonsson, E. N. & Karlsson, M. O. Automated covariate model building within NONMEM. Pharm. Res. 15, 1463–1468 (1998).
U. S. Food and Drug Administration. Guidance for industry: population pharmacokinetics. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/population-pharmacokinetics (2019).
Gastonguay, M. R. Full covariate models as an alternative to methods relying on statistical significance for inferences about covariate effects: a review of methodology and 42 case studies. In 20th Annual Meeting of the Population Approach Group Europe (PAGE) (Metrum, 2011).
Kasserra, C. et al. Pomalidomide: evaluation of cytochrome P450 and transporter-mediated drug-drug interaction potential in vitro and in healthy subjects. J. Clin. Pharmacol. 55, 168–178 (2015).
International Transporter Consortium et al. Membrane transporters in drug development. Nat. Rev. Drug Discov. 9, 215–236 (2010).
Author information
Authors and Affiliations
Contributions
N.K. and Y.L. contributed to conception and design and analysis; X.W. and Y.L. contributed to acquisition of data; all authors contributed to interpretation of data; K.O. and Y.L. drafted and revised the article; all authors reviewed and approved the article.
Corresponding author
Ethics declarations
Competing interests
K.O., X.W., B.B., S.Z., M.P., and Y.L. are employees and hold equity ownership in Bristol Myers Squibb.
Consent statement
Written informed consent/assent was obtained from all subjects or parents/guardians prior to enrollment into the studies.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ogasawara, K., Kassir, N., Wang, X. et al. Recurrent or progressive pediatric brain tumors: population pharmacokinetics and exposure–response analysis of pomalidomide. Pediatr Res 90, 832–839 (2021). https://doi.org/10.1038/s41390-020-01304-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01304-6