Abstract
Background
We aimed to investigate the clinical implications of unresponsiveness to single or repeated courses intravenous immunoglobulin (IVIG) and Kawasaki disease (KD) shock syndrome in patients with KD in an era of a single brand of IVIG.
Methods
Data were collected from National Health Insurance database 2010–2013. Characteristics of the KD patients were analyzed, including age, gender, shock, and associated coronary aneurysms.
Results
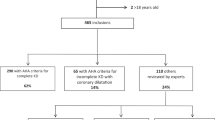
There were 3043 KD patients (male: 1872) identified. Among them, 46 (1.51%) had KDSS, 261 patients (8.5%) had IVIG unresponsiveness, and 225 patients (7.4%) developed coronary aneurysms. Moreover, 51 patients did not respond to the second course IVIG therapy, i.e., re-IVIG unresponsiveness. KDSS was associated with the occurrence of IVIG unresponsiveness (P < 10−4) and re-IVIG unresponsiveness (P = 0.02). In addition to male gender and KD shock syndrome, IVIG unresponsiveness (OR: 2.18, 95% CI: 1.48–3.22, P = 0.001) and re-IVIG unresponsiveness (OR: 2.87, 95% CI: 1.40–5.89, P = 0.004) were both independent risk factors for coronary aneurysms.
Conclusions
In a nationwide KD cohort, both IVIG unresponsiveness and re-IVIG unresponsiveness increase the risk of coronary aneurysms. Such observation addresses the importance of refining the treatment for IVIG unresponsiveness, at least in those with KD shock syndrome.
Similar content being viewed by others
Introduction
Kawasaki disease (KD), an acute febrile systemic vasculitis first reported by Dr. Kawasaki in 1967,1 has become the leading cause of acquired heart disease in children in developed countries.2,3,4 Most patients with KD respond well to a single high-dose intravenous immunoglobulin (IVIG) plus aspirin.2 Nevertheless, 6.7–26.8% of KD patients do not achieve defervescence after the first dose of IVIG.4,5,6 This phenomenon is referred to as IVIG unresponsiveness. IVIG unresponsiveness to the first course of IVIG therapy is associated with an increased risk of having coronary complications and is not uncommon in most populations worldwide.4,7,8 For those with IVIG unresponsiveness, a second course of IVIG is recommended. However, they might still not respond to the second course IVIG, i.e., re-IVIG treatment unresponsiveness.9,10 Furthermore, KD shock syndrome (KDSS) is a less common complication of KD and defined as episodes during the acute stage of KD with hypotension and shock requiring the initiation of volume expanders or the infusion of vasoactive agents. Previous study had indicated that KDSS was associated with IVIG unresponsiveness.11 However, the relationship between KDSS and re-IVIG unresponsiveness was still unclear. In Taiwan, since 2008, TBSF human immunoglobulin (CSL limited, Parkville VIC3052, Australia) has become the only one brand of IVIG available and reimbursed by Taiwan’s National Health Insurance (NHI). Taiwan’s NHI, implemented in 1995, covers >99% of Taiwanese population. The NHI database contains complete medical information of patients, including diagnosis and management, and has become a reliable source of data for epidemiology studies.12 We, therefore, conducted the study, in an era of single brand IVIG, to investigate the recent epidemiological profile of KD, particularly KDSS, IVIG unresponsiveness to the first and the second courses of IVIG therapy and their clinical implications.
Methods
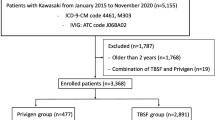
This study was a population-based retrospective cohort study and approved by the Institutional Review Board of National Taiwan University Hospital (201810124RINA). Health care records from 2010 to 2013 were collected from the NHI database. We selected patients with reference to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for Kawasaki disease (446.1). Children aged <10 years who had been admitted to hospitals and received IVIG (K000841248) therapy under a primary diagnosis of KD were enrolled. We collected demographic data, including age, gender, residence code, ICD-9-CM codes, admission and discharge data of hospitalization, inpatient and ambulatory care orders, and reimbursement details. Recurrence was defined as readmission for IVIG because of KD > 30 days after the first admission.
IVIG unresponsiveness
The name of IVIG used in Taiwan between 2010 and 2013 was “TBSF” Human Immunoglobulin for Intravenous Use, which is prepared from pooled human plasma donated by Taiwan’s voluntary and non-remunerated donors (http://intra.blood.org.tw/upload/51646ad1-c1ae-459b-87b2-2d96611bd6f9.pdf). The IVIG is a sterile, preservative-free solution containing 6 g of human protein and 10 g of maltose in each 100 mL. The solution has a pH of 4.25. Isotonicity is achieved by the addition of maltose. At least 98% of the protein has the electrophoretic mobility of immunoglobulin G (IgG). At least 90% of the protein is IgG monomer and dimer. “TBSF” Human Immunoglobulin for Intravenous Use contains only trace amounts of Immunoglobulin A (IgA) (nominally <0.025 mg/mL). The manufacturing process contains dedicated steps to reduce the possibility of virus transmission including pasteurization (heating at 60 °C for 10 h) and incubation at low pH. The median isoagglutinin titers after immunoaffinity chromatography were 1:8 for anti-A and 1:4 for anti-B.
Between 2010 and 2013, we followed the American Heart Association 2004 scientific statement on KD13 in Taiwan and provided one additional course of IVIG (2 g/kg) to patients with KD who did not exhibit defervescence after the first course of IVIG therapy. Therefore, IVIG unresponsiveness was defined if the patients received two or more courses of IVIG. They are further defined as re-IVIG unresponsiveness if they had to receive three or more courses of IVIG or additional immune modifiers after the second course of IVIG. Because NHI database does not record the exact course number of IVIG given to the patients, we estimated the number of IVIG courses using the following formula:
Estimated number of course (N) = total IVIG amount/[(median body weight by age and gender) × 2 g/Kg].
The age-dependent median body weight was derived from the growth curve used in Taiwan (http://health99.hpa.gov.tw/doc/12024.pdf).14 We defined that the patients had IVIG unresponsiveness when they had been hospitalized for >4 days and had an estimated N > 1.5 and that the patients had “re-IVIG unresponsiveness” when they (1) had an estimated N > 2.5 or (2) had an estimated N > 1.5, concomitant usage of steroids, and hospitalization >6 days.
KD shock syndrome
Our previous studies12,15 showed that KDSS, in Taiwan, was associated with more coronary arterial lesions (CAL). Therefore, in the current study, we also investigated the potential association of KDSS with IVIG unresponsiveness, re-IVIG unresponsiveness, and coronary aneurysms. We used the same approach as previously reported15 to identify those patients with KDSS.
Coronary aneurysms
Those with the diagnostic codes of ICD-9-CM 414.11, 414.8, or 414.9 were regarded as having coronary aneurysm(s).
Statistics
The descriptive analyses were expressed as median (with interquartile range (IQR)) or mean (standard deviation) for continuous variables, such as age and hospitalization duration, and frequency (%) for categorical variables. The two groups were compared with two-sample T test or Mann–Whitney U test for continuous variables and proportionality differences were tested using Chi-square test or Fisher’s exact test. Statistical significance was set at P < 0.05. Statistical analyses were performed using R and SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Overall
Between 2010 and 2013, a total of 3106 hospitalizations for KD and IVIG were reported for 3043 patients aged <10 years. The distribution of patients with KD hospitalized by months is displayed in Fig. 1. KD occurred most frequently (35.3%) in the summer, least frequently (17.6%) in the winter. Their median age was 15.5 months (IQR: 8.3–28.3 months). The age-specific distribution of KD cases is presented in Fig. 2. The incidence of KD was 75.3 per 105 children aged <5 years during the study period (72.6 in 2010, 68.1 in 2011, 70.4 in 2012, 90.1 in 2013, trend test revealed no significant changes). The male-to-female ratio was 1.59 (male: 1872). Recurrence was noted in 34 (1.1%) of the 3043 enrolled KD children. One boy and one girl each had three KD episodes. The median interval between the first and second attacks was 6.5 (IQR: 3.7–16) months. Coronary artery aneurysms were noted in 225 patients (225/3042 = 7.4%, male: 152). No mortalities were noted during the study period.
KD shock syndrome
KDSS was noted in 46 patients (1.51%; male: 25). The median age of KDSS patients was 26.2 months (IQR: 11.5–44.1 months), significantly older than the remaining 2997 KD patients (median: 15.2 months, IQR: 8.2–27.5 months, P = 0.005). Of the 46 KDSS patients, 10 (21.7%) had coronary aneurysms, significantly higher than the remaining KD patients (215/2782, χ2 = 12.0, P = 0.005)
IVIG unresponsiveness
The distribution of N of IVIG therapy is displayed in Supplementary Fig. S1. We discovered that, between 2010 and 2013, 261 (261/3055, 8.5%) patients underwent an estimated number of courses of IVIG > 1.5, thereby demonstrating IVIG unresponsiveness. The annual percentage of IVIG unresponsiveness (defined as the number of cases with IVIG unresponsiveness divided by KD case number) was 8.7% in 2010, 9.3% in 2011, 6.8% in 2012, and 9.4% in 2013 (Fig. 1, trend test revealed no significant changes.).
Of the 261 KD patients with IVIG unresponsiveness, 152 were male (58.2 %, M:F = 1.4:1). No significant difference was noted on the distribution of IVIG unresponsiveness among seasons (Fig. 1). Univariate analysis showed that KDSS, rather than gender and age, was associated with IVIG unresponsiveness. (Table 1A) The median duration of hospitalization for KD patients with IVIG unresponsiveness was 9 days (IQR: 7–12 days), significantly longer than those without (5 days, IQR: 4–7 days, P < 10−4). We conducted a multivariate logistic regression to evaluate the independent effects of gender, KDSS, and age on IVIG unresponsiveness and found that KDSS was the only independent risk factor for IVIG unresponsiveness. (odds ratio (OR): 10.19, 95% confidence interval (CI): 5.62–18.51, P = 0.001).
Of the 261 KD patients with IVIG unresponsiveness, 39 (14.9%) had coronary aneurysms (Fig. 3). The percentage of patients who developed coronary aneurysms differed significantly between the KD patients who were IVIG unresponsive or not (39/261 vs 186/2782, χ2 = 22.8, P < 10−4).
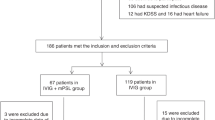
Patients unresponsive to the second course of IVIG (re-IVIG unresponsiveness)
Of the 261 KD patients with IVIG unresponsiveness, 51 (51/261, 19.5%; 51/3043, 1.7%) did not achieve defervescence after receiving the second course of IVIG, so-called “re-IVIG unresponsiveness,” and required a third course of IVIG in 42 or steroids alone in 9. Re-IVIG unresponsiveness was not associated with the calendar years (11 in 2010, 14 in 2011, 9 in 2012, and 17 in 2013; χ2 = 1.12, P = 0.77). Of the 51 KD patients with re-IVIG unresponsiveness, the median age was 12.8 months and the percentage who were boys was 66.7%, which were similar results to those for the remaining 210 KD patients responsive to re-IVIG. (Table 1B) However, patients with re-IVIG unresponsiveness had a significantly longer hospitalization duration (median: 11 days) and greater prevalence of KDSS (9/51) (Table 1B). Again, a multivariate logistic regression showed that KDSS, rather than age or gender, was the only independent risk factor for re-IVIG unresponsiveness (OR: 3.38, 95% of CI: 1.34–8.53, P = 0.01). The 51 patients with re-IVIG unresponsiveness had a significantly higher percentage (13/51, 24.5%) of coronary aneurysms compared with the remaining 2992 KD patients (212/2992, P < 10−4). Furthermore, compared with the 210 KD patients responsive to the second course of IVIG, the 51 patients still had significantly higher risk to have coronary aneurysms (13/51 vs 26/210, P = 0.04) (Fig. 3). We failed to detect significant difference in the percentages of CAL between re-IVIG unresponsive KD patients with steroid therapies and those without (2/9 vs 11/42, χ2 = 0.03, P = 1.0).
Risk factors of coronary aneurysms
Based on the above, univariate analysis (Table 2) determined that the development of coronary aneurysms was associated with KDSS (P = 0.002), IVIG unresponsiveness (P < 10−4), and re-IVIG unresponsiveness (P < 10−4). To avoid interactions among gender, KDSS, and IVIG unresponsiveness, we conducted a multivariate logistic regression to evaluate their independent effects on the risk of coronary aneurysms. The results demonstrated that IVIG unresponsiveness (Table 2A, OR: 2.16, 95% of CI: 1.46–3.19, P = 0.001), male gender (P = 0.04), and KDSS (P = 0.01) were all independent risk factors for the occurrence of coronary aneurysms.
We also conducted a multivariate logistic regression analysis to evaluate the independent effect of “re-IVIG unresponsiveness” on the development of coronary aneurysms (Table 2B). The results showed, independent from KDSS, that re-IVIG unresponsiveness was still significantly associated with the occurrence of coronary aneurysms (Table 2B, P = 0.001). However, among the 261 patients with IVIG unresponsiveness, a multivariate logistic regression analysis demonstrated, for the development of coronary aneurysms, the OR of “re-IVIG unresponsiveness” and KDSS were 1.79 (95% CI: 0.81–3.98, P = 0.15) and 1.19 (95% of CI: 0.37–3.86, P = 0.77), respectively.
Discussion
State-of-the-art therapy for KD emphasizes the importance of identifying patients with risk of coronary complication. In this nationwide KD cohort receiving only a single brand of IVIG, we demonstrated three novels findings: (1) re-IVIG unresponsiveness accounted for 19.5% of the KD patients unresponsive to the first course of IVIG; (2) KDSS was associated not only with IVIG unresponsiveness but also with re-IVIG unresponsiveness; and (3) re-IVIG unresponsiveness, in addition to IVIG unresponsiveness, KDSS, and male gender, was also an independent risk factor for coronary complication. Such observation had never been described before and addresses the importance of refined strategy for second course of IVIG therapy in KD patients with IVIG unresponsiveness, at least in those with KDSS.
Though the studies in some countries suggested an increasing trend with calendar year, in the current study, between 2010 and 2013, the incidence of KD in children aged <5 years remains 75.3 per 105 and was stationary over years. The incidence data of KD in Taiwan was the third world highest, just next to Japan and Korea.4 The IVIG therapy is now the standard treatment for KD during the acute stage. Nevertheless, IVIG unresponsiveness was observed in 6.7–26.8% of KD patients.4,5,6 In our cohort, 8.5% (261/3043) and 1.7% (51/3043) of KD patients did not respond to the first and the second courses of IVIG, respectively. Namely, 19.5% (51/261) of those unresponsive to the first IVIG therapy would not respond to the second course of IVIG therapy. The percentage of the re-IVIG unresponsiveness was less studied before. From a Korean institutional cohort, the percentage of re-IVIG unresponsiveness in those with IVIG unresponsiveness was 11.3%.10 The brand of IVIG was not specified and almost half (48%) of their patients with IVIG unresponsiveness also received intravenous methyl-prednisolone with the second course of IVIG.10 The unique characteristic of the current cohort was that only a single brand of IVIG was used during the study period. Such unique characteristic enabled us to minimize the bias generated from different processing of IVIG and provided us the optimal estimate for the percentage of IVIG unresponsiveness and re-IVIG unresponsiveness.
In our patients, coronary aneurysms occurred in 14.9% of those unresponsive to the first course of IVIG therapy. But if they were still unresponsive to the second IVIG course, coronary aneurysm occurred in 24.5% of the patients and almost doubled the risk. Both the IVIG and re-IVIG unresponsiveness significantly increased in patients with KDSS and were at risk of developing coronary aneurysms, suggesting a strategic approach for the IVIG unresponsiveness. There are currently two treatment strategies for patients with IVIG unresponsiveness.6,16 The first is intensification of primary therapy, that is, initial administration of IVIG and adjuvant therapies (usually steroid) to certain KD patients selected by using a scoring system5 such as Kobayashi17 and Egami18 scoring systems. The second is rescue therapy, that is, retreatment with the second course of IVIG, steroids, infliximab, or a combination of these medications after the first course of IVIG therapy.2,5 The predictors for re-IVIG unresponsiveness remain unclear. A low serum protein level had been suggested, but half of that study cohort also received intravenous methyl-prednisolone with the second course of IVIG.10 In the current study cohort who received a single brand of IVIG, we demonstrated that KDSS is an important predictor not only for IVIG unresponsiveness but also for re-IVIG unresponsiveness. Previous hospital-based studies have reported that KD patients admitted to Intensive Care Unit were more likely to have IVIG unresponsiveness.19 The real pathophysiology responsible for such association is unclear, but higher underlying inflammation along with decreased myocardial contractility or capillary leakage19,20 may play important roles. We, therefore, suggest that (1) KDSS patients may need more aggressive therapy at the initial treatment and (2) retreatment with second course of IVIG should be refined to combine either of steroids, infliximab, or others, at least in patients with KDSS.
Study limitations
This study was subject to certain limitations. First, the NHI database only recorded the items of medication and their respective expense. Laboratory data, dosage of medication (like aspirin), duration of fever, and how far apart each IVIG dose was administrated cannot be retrieved from the current database. That may cause overestimation of IVIG or re-IVIG unresponsiveness and made us unable to analyze further the detailed potential laboratory risk factors of IVIG unresponsiveness. Second, HNI database does not have messages on the presence of major KD symptoms, which we can differentiate into typical or atypical KD. Third, the coronary aneurysms were defined on the basis of ICD-9-CM code 414.11, and we therefore might miss those with coronary dilatation (without aneurysm)/ectasia and underestimate the number of KD patients with CAL.
Conclusions
In a nationwide KD cohort 2010–2013, the incidence profile of KD in children aged <5 years was stationary over time. In the study period, KD cohort was treated with only one brand of IVIG, and the percentages of KDSS and IVIG unresponsiveness were 1.5% and 8.5%, respectively. Among those with IVIG unresponsiveness, 19.5% did not respond to re-IVIG therapy. KDSS was associated with IVIG and re-IVIG unresponsiveness. Both IVIG and re-IVIG unresponsiveness were major independent predictors for coronary aneurysms besides male gender and KDSS. Such observation addresses the importance of refining the treatment for IVIG unresponsiveness, at least in those with KDSS.
References
Kawasaki, T. Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children. Arerugi 16, 178–222 (1967).
McCrindle, B. W. et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a Scientific Statement for Health Professionals From the American Heart Association. Circulation 135, e927–e929 (2017).
Lin, M. T. et al. Acute and late coronary outcomes in 1073 patients with Kawasaki disease with and without intravenous gamma-immunoglobulin therapy. Arch. Dis. Child. 100, 542–547 (2015).
Lin, M. T. & Wu, M. H. The global epidemiology of Kawasaki disease: review and future perspectives. Glob. Cardiol. Sci. Pract. 2017, e201720 (2017).
JCS Joint Working Group. Guidelines for diagnosis and management of cardiovascular sequelae in Kawasaki disease (JCS 2013). Digest version. Circ. J. 78, 2521–2562 (2014).
Newburger, J. W., Takahashi, M. & Burns, J. C. Kawasaki disease. J. Am. Coll. Cardiol. 67, 1738–1749 (2016).
Saji, B. T., Newburger, J. W., Burns, J. C. & Takahashi, M. in Kawasaki Disease: Current Understanding of the Mechanism and Evidence-Based Treatment Epidemiology 77–103 (Springer Japan, 2017).
Tremoulet, A. H. et al. Resistance to intravenous immunoglobulin in children with Kawasaki disease. J. Pediatr. 153, 117–121 (2008).
Hashino, K. et al. Re-treatment for immune globulin-resistant Kawasaki disease: a comparative study of additional immune globulin and steroid pulse therapy. Pediatr. Int. 43, 211–217 (2001).
Seo, E. et al. Prediction of unresponsiveness to second intravenous immunoglobulin treatment in patients with Kawasaki disease refractory to initial treatment. Korean J. Pediatr. 59, 408–413 (2016).
Kanegaye, J. T. et al. Recognition of a Kawasaki disease shock syndrome. Pediatrics 123, e783–e789 (2009).
Wu, M. H., Lin, M. T., Chen, H. C., Kao, F. Y. & Huang, S. K. Postnatal risk of acquiring Kawasaki disease: a nationwide birth cohort database study. J. Pediatr. 180, 80.e2–86.e2 (2017).
Newburger, J. W. et al. Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease; Council on Cardiovascular Disease in the Young; American Heart Association; American Academy of Pediatrics. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 110, 2747–2771 (2004).
Chen, W. & Chang, M. H. New growth charts for Taiwanese children and adolescents based on World Health Organization standards and health-related physical fitness. Pediatr. Neonatol. 51, 69–79 (2010).
Lin, M. T., Fu, C. M., Huang, S. K., Huang, S. C. & Wu, M. H. Population-based study of Kawasaki disease shock syndrome in Taiwan. Pediatr. Infect. Dis. J. 32, 1384–1386 (2013).
Tremoulet, A. H. Adjunctive therapies in Kawasaki disease. Int. J. Rheum. Dis. 21, 76–79 (2018).
Kobayashi, T. et al. RAISE study group investigators. Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (RAISE study): a randomised, open-label, blinded-endpoints trial. Lancet 379, 1613–1620 (2012).
Ogata, S. et al. Corticosteroid pulse combination therapy for refractory Kawasaki disease: a randomized trial. Pediatrics 129, e17–e23 (2012).
Dominguez, S. R. et al. Kawasaki disease in a pediatric intensive care unit: a case-control study. Pediatrics 122, e786–e790 (2008).
Knockaert, D. C. Cardiac involvement in systemic inflammatory diseases. Eur. Heart J. 28, 1797–1804 (2007).
Acknowledgements
This study was supported by the Ministry of Science and Technology, Taiwan (grant no. 107-2321-B-002 -026).
Author information
Authors and Affiliations
Contributions
Y.-C.L. and C.-H.C. worked for data collection and initial manuscript. F.-Y.K. and S.-K.H. provided statistics counseling. M.-H.W. worked for data interpretation. M.-T.L. had full access to all the data and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Liang, YC., Chang, CH., Lin, MT. et al. Shock and unresponsiveness to repeated courses of intravenous immunoglobulin in Kawasaki disease: a nationwide database study. Pediatr Res 87, 961–966 (2020). https://doi.org/10.1038/s41390-019-0668-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0668-1
This article is cited by
-
Kawasaki disease and influenza—new lessons from old associations
Clinical Rheumatology (2021)