Abstract
Background
The use of corticosteroids in Kawasaki disease (KD) is still controversial. The aim of this study was to investigate the safety and effectiveness of modified methylprednisolone (mPSL) regimen as an initial treatment for refractory KD.
Methods
This is a real-world observational study. We identified refractory KD with a self-developed scoring system. Patients were divided into the intravenous immunoglobulin (IVIG) + mPSL group and the IVIG group. Clinical outcomes and changes in coronary arteries after the treatment during a 12-week period were observed. Propensity-score matching was used to analyze those patients with similar baseline characteristics.
Results
Of a total of 168 patients, 104 patients were assigned into the IVIG group and 64 patients into the IVIG + mPSL group. The therapeutic response rate of the IVIG + mPSL group was significantly higher than that of the IVIG group (98.4 vs 76.0%, P < 0.05). The IVIG + mPSL group had a shorter duration of fever and a higher rate of C-reactive protein decline than the IVIG group (1.17 ± 0.64 vs 1.81 ± 1.16 days; 88.1 vs 83.5%; P < 0.05). The luminal diameter and Z-score of the left circumflex coronary artery (LCX) were significantly smaller and lower in the IVIG + mPSL group than that in the IVIG group at weeks 2 and 12.
Conclusions
Modified mPSL regimen has minimal side effects. It might improve the initial response to IVIG and decrease the dilation of LCX for refractory KD.
Impact
-
Modified mPSL regimen (2–4 mg/kg/day, divided into 2–3 doses for 3–5 days, then 1 mg/kg/day, once a day for 3–5 days, then oral prednisone was tapered over 3–5 weeks in 5–7 days steps) as an intensive initial treatment can decrease LCX dilation in high-risk IVIG-resistant KD patients.
-
Our self-developed scoring system has been proven validated and can be used to identify high-risk IVIG-resistant KD patients in North China.
-
The present study provides an alternative therapeutic regimen for high-risk refractory KD patients.
Similar content being viewed by others
Introduction
Kawasaki disease (KD) is an acute, self-limited febrile illness of unknown etiology that predominantly affects infants and young children. Up to 25% of untreated KD patients develop coronary artery aneurysms. Intravenous immunoglobulin (IVIG) combined with aspirin is the mainstay of initial treatment of KD to reduce inflammation and to prevent coronary artery abnormalities.1 However,10–15% of patients are resistant to IVIG treatment and develop persistent or recrudescent fever 36–48 h after the initial treatment.
IVIG resistance is associated with a high risk of coronary artery abnormalities. Serious conditions, such as a giant coronary artery aneurysm, may lead to myocardial ischemia, infarction, and sudden death.2,3,4,5 KD patients with IVIG resistance may benefit from more aggressive initial therapy.6,7,8,9
The efficacy of steroid therapy in KD remains controversial. Although several issues are still under study, one study shows how to identify high-risk IVIG-resistant KD patients and another study shows how to refine a special therapeutic regimen for those patients.
By far, several scoring systems have been developed to predict IVIG resistance, most of which were derived from Japan, with good sensitivity and specificity.10,11,12,13,14,15,16,17,18,19 However, these systems are insufficient in other populations, which might be attributed to the geographical difference and racial heterogeneity.
Since 2009, there have been two main therapeutic regimens reported in Japan for high-risk IVIG-resistant KD patients,20,21,22,23 one is intravenous methylprednisolone pulse therapy (30 mg/kg over 2 h) and the other is continuously intravenous methylprednisolone (2 mg/kg/day, divided into 3 doses) until the fever resolved, followed by oral prednisolone until CRP level is normal (<5 mg/L), and then prednisolone was tapered over 15 days in a 5-day step. In this study, an alternative therapeutic regimen was investigated for high-risk IVIG-resistant KD patients.
Subjects and methods
Subjects
Children who were diagnosed with KD and hospitalized at the cardiology ward in Children’s Hospital Capital Institute of Pediatrics in Beijing, China, from January 2017 to March 2020 were enrolled in this study. The study was approved by the Ethics Committee of Capital Institute of Pediatrics (No. SHERLL 2015040). Informed consent was obtained from one parent or guardian of each patient.
Inclusion criteria
The inclusion criteria were as follows: (1) first-time hospitalized KD patients; (2) high-risk IVIG-resistant KD patients were identified using a self-developed scoring system;24 (3) one parent or guardian of children signed informed consent.
Exclusion criteria
The exclusion criteria were as follows: (1) patients were diagnosed with KD after the tenth day of illness (the first illness day was defined as the day of fever onset); (2) patients with a history of KD; (3) patients with contraindications for corticosteroids; (4) patients who had received corticosteroids on account of other diseases.
Other definitions in the study
(1) The diagnosis of classic KD was based on febrile days ≥5 and the presence of ≥4 of the five principal clinical features such as rash, erythema and cracking of lips and strawberry tongue, bilateral bulbar conjunctival injection without exudate, erythema, and edema of the extremities in the acute phase, and/or periungual desquamation in subacute phase and cervical lymphadenopathy (≥1.5 cm in diameter).
The diagnosis of incomplete KD was based on fever ≥5 days and two or three compatible clinical criteria with coronary artery abnormalities, or without coronary artery abnormalities, but had C-reactive protein (CRP) ≥30 mg/L and (or) erythrocyte sedimentation rate ≥40 mm/h, with three or more laboratory findings: albumin ≤30 g/L, anemia for age, increased alanine aminotransferase level, platelet count ≥450 × 109/L after the seventh day of fever, white blood cell (WBC) count ≥15 × 109/L, and urine ≥10 WBC/HP.
(2) The score points for each variable in the high-risk predictive system were as follows: CRP ≥90 mg/L (3 points), the percentage of neutrophils (N%) ≥70% (2.5 points), serum sodium <135 mmol/L (3 points), albumin <35 g/L (2.5 points), and total bilirubin >20 μmol/L (5 points).24 Laboratory data were obtained before treatment. When they were measured multiple times, we were able to record the highest values for CRP, N%, and total bilirubin and the lowest values for serum sodium and albumin. A total of 6 points or more were considered as indicating a high risk of IVIG resistance.
(3) The therapeutic response was defined as axillary temperature <37 °C for 48 h after treatment and disappearance of acute clinical signs associated with KD. Therapeutic response rate refers to the ratio of patients with positive therapeutic responses in each group.
Methods
This is a real-world observational study
The subjects were assigned to either the IVIG group or the IVIG + modified methylprednisolone (mPSL) group by a pediatrician or the parent (or guardian). When the children were admitted, our pediatricians evaluated the children according to the self-developed scoring system. Then, the pediatricians would recommend the treatment plan to the parent (or guardian) for high-risk children whose total score was ≥6 points, and also explain the risks and benefits of corticosteroid application in detail. Finally, the treatment plan would be decided by the parent (or guardian). Then, the patients and the data analysts were blinded to the treatment conditions.
Patients were treated with IVIG (2 g/kg over 8–12 h intravenous injection) and oral aspirin (30–50 mg/kg/day, three times a day, after afebrile followed by 3–5 mg/kg/day, once a day) in the IVIG group. Patients in the IVIG + mPSL group were given mPSL plus the same IVIG and aspirin therapy as in the IVIG group. The use of mPSL was as follows: mPSL intravenous injection 2–4 mg/kg/day, divided into 2–3 doses for 3–5 days. Different doses of methylprednisolone were given depending on our self-developed scoring system. For patients whose score was ≥10 points, we applied methylprednisolone of 4 mg/kg/day. While for patients whose score was <10 points, we administered methylprednisolone of 2 mg/kg/day, followed by 1 mg/kg/day, once a day for 3–5 days, until the fever resolved and CRP went back to normal. Afterwards, oral prednisone was tapered over 3–5 weeks in steps of 5–7 days (1, 0.75, 0.5, and 0.25 mg/kg/day for 5–7 days). The course of oral prednisone depends on the changes in the coronary artery diameter. On progressive dilatation of coronary arteries, the course of treatment was 7 days in each step; otherwise it was 5 days.
Laboratory tests
WBC count, N%, liver enzymes, blood glucose, coagulation function, and CRP were measured before treatment and 72 h after initial treatment. The decreasing rate of CRP, an indicator of therapeutic effectiveness, was calculated by subtracting post-treatment value from pre-treatment value divided by pre-treatment value.
Coronary artery assessment by echocardiography
Transthoracic echocardiography was performed before treatment (baseline days 5–7) and during follow-up week 2 (days 10–14), week 4 (days 20–40), week 8 (days 50–60), and week 12 (days 80–90). The first illness day was defined as the day of fever onset. An echocardiogram was performed every 3–5 days for severe coronary artery abnormality. The internal lumen diameter of the proximal right coronary artery (RCA), left main coronary artery (LMCA), proximal left anterior descending artery (LAD), and left circumflex coronary artery (LCX) was measured at each time-point.
We measured the coronary arterial diameter at the minimum gain setting and used a high-frequency transducer optimize resolution. According to the standard method of visualizing and measuring coronary arteries, which has been proposed by McCrindle et al.,1 the diameter is measured during the early diastolic phase at the end of the T wave. Diameter is the distance between the internal wall of vessels, avoiding arterial bifurcation. Imaging resolution was set to maximum, and sedation was applied to young or uncooperative children. It is important to observe all locations where coronary lesions are likely to occur. Coronary artery abnormalities were defined as Z-score >2.0 according to the criteria of Kobayashi Z-score adjusted for body surface area.25 Dilation only: Z-score ≥2.0 or more and <2.5; small aneurysm: 2.5 ≤ Z-score < 5; medium aneurysm: 5.0 ≤ Z-score < 10.0; giant aneurysm: Z-score ≥ 10.
Statistical analyses
The U test was used to identify whether variables had a normal distribution. Continuous variables were expressed as \(\overline \chi\) ± S for data that were normally distributed, and median and quartile range (M (Q1, Q3)) were used for data that were not normally distributed. T test was used for continuous variables if the data were normally distributed. χ2 test was used to analyze the categorical variables.
Given the differences in the baseline characteristics between eligible participants in those two groups (Table 1), propensity-score matching was used to identify a group of patients with similar baseline characteristics. The propensity score is a conditional probability of having a particular exposure (IVIG + mPSL vs IVIG) given a set of baseline measured covariates. The propensity score was estimated with the use of a non-parsimonious multivariable logistic regression model, with the use of IVIG + mPSL as the dependent variable and all the baseline characteristics outlined in Table 1 as covariates. Matching was performed with a 1:1 matching protocol without replacement (greedy-matching algorithm), with a caliper width equal to 0.2 of the standard deviation of the logit of propensity score.
The primary outcome analysis used a mixed model of longitudinal regression for repeated measures that accounted for the correlation among outcome scores for the same patient. The adjusted mean difference in the primary outcome was tested at 2-week follow-up. Model included the treatment, time, and the interaction between trial group and visit. The score at baseline was included as a covariate.
Analyses were performed using Stata version 14.2. All tests were two-sided and P value < 0.05 was considered statistically significant. Statistical power was calculated with PASS 2021.
Results
Demographic characteristics
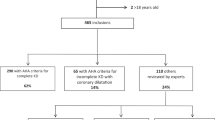
From January 2017 to March 2020, there were 1371 children diagnosed and hospitalized with KD at the Children’s Hospital Capital Institute of Pediatrics, Beijing, China. Among them, 186 patients met the inclusion criteria. Eighteen patients were excluded due to incomplete coronary artery data, and the rest of 168 patients were enrolled in the study (Fig. 1). There were 64 patients (38%) in the IVIG + mPSL group, 38 boys (59.4%) and 26 girls (40.6%), and 104 patients (62%) in the IVIG group, 60 boys (57.7%) and 44 girls (42.3%); mean age was 2.57 ± 1.76 years old, minimum age was 2 months, and maximum age was 9 years old (Table 1).
Clinical data before initial treatment
Patients in the two groups had similar baseline characteristics in age, sex, and inflammatory index (WBC, N%, and CRP). The distribution of Z-score of each coronary artery before initial treatment was shown in Fig. 2. There were significant differences between the IVIG + mPSL group and the IVIG group with regard to scores of high-risk IVIG resistance, luminal diameter, and Z-score of LMCA (Table 1). Propensity-score matching was used to identify patients with similar baseline characteristics (Table 1). After propensity-score matching, there were 53 patients in each group, the minimum age was 2 months and the maximum age was 9 years old.
Therapeutic response
Therapeutic response rate in the IVIG + mPSL group was significantly higher than that in the IVIG group [98.4% (63/64) vs 76.0% (79/104), P < 0.001]. Patients in the IVIG + mPSL group had a shorter duration of fever than the IVIG group (1.22 ± 0.766 vs 1.74 ± 1.174 days, P = 0.002). CRP decreasing rate of the IVIG + mPSL group was significantly higher than that in the IVIG group (87.7 vs 81.4%, P = 0.014).
Twenty-six patients did not respond to initial therapy, one in the IVIG + mPSL group and 25 in the IVIG group. Eighty-eight percent (22/25) of the patients in the IVIG group were treated with glucocorticoids (alone or in combination with IVIG).
Changes in coronary artery
Incidence of coronary artery abnormality at baseline
The incidence of abnormalities of RCA, LMCA, LAD, and LCX at baseline in two groups was 21.4% (36/168), 24.4% (41/168), 11.9% (20/168), and 2.4% (4/168), respectively. If one coronary artery was abnormal, we considered it as coronary artery abnormality. Therefore, the incidence of coronary artery abnormality was 36.9% (62/168).
Comparison of the changes in coronary artery internal lumen diameter and Z-score
Mean values of luminal diameter and Z-scores of LCX were significantly lower in the IVIG + mPSL group than those in the IVIG group at week 2 (1.43 ± 0.04 vs 1.60 ± 0.04, P = 0.001; −0.21 ± 0.11 vs 0.32 ± 0.11, P < 0.001) and week 12 (1.46 ± 0.04 vs 1.57 ± 0.04, P = 0.034; −0.13 ± 0.11 vs 0.18 ± 0.11, P = 0.056). There were no significant differences in RCA, LMCA, and LAD between the two groups at each follow-up time-points through 12 weeks (P > 0.05) (Figs. 3 and 4 and Tables 2 and 3). We used propensity-score matching to analyze patients with similar baseline characteristics, and this led to a reduced number of patients in both groups. The statistical power was calculated, and it was powered enough for LCX at week 2. However, it was not powered enough for other coronary arteries such as RCA, LMCA, and LAD (Supplementary part, Table S1).
There were seven patients with medium or large coronary artery aneurysm at 2 weeks of the disease, four in the IVIG + mPSL group, and three in the IVIG group. In the IVIG + mPSL group, the Z-score of each coronary artery diameter reached the peak at 2–4 weeks of the disease, and then it became stable or decreased. While in the IVIG group, each coronary artery showed progressive dilation (Supplementary part, Table S2). Because the number of cases was small, we did not carry out further analysis. The phenomenon suggests that corticosteroids may have a better protective effect on severe coronary aneurysm.
Comparison of the changes in coronary artery internal lumen diameter and Z-score with different steroid regimen
We investigated the influence of different selected doses of mPSL on the coronary artery during the initial treatments in this study. (1) 2 mg/kg Group: patients received mPSL 2 mg/kg/day and (2) above 2 mg/kg group: patients received mPSL between 2 and 4 mg/kg/day. There were no significant differences in luminal diameter and Z-scores of RCA, LMCA, LAD, and LCX between the two groups at each follow-up time-point through 12 weeks (P > 0.05) (Supplementary part, Table S3).
Additional treatments and methylprednisolone-related adverse reactions and side effects
The incidence of additional rescue treatments was lower in the IVIG + mPSL group than in the IVIG group (1.6% (1/64) vs 24.0% (25/104), P < 0.001). Twenty patients received additional rescue treatments in the IVIG group with IVIG (alone or in combination with mPSL).
There was no serious adverse effect. Heart rate and blood pressure were monitored during the treatment in both the IVIG group and IVIG + mPSL group. There were no significant differences in heart rate (119 ± 38 vs 116 ± 40 beats/min, P = 0.625) and blood pressure (92/55 vs 90/52 mm Hg, P = 0.550) between the IVIG and IVIG + mPSL group. There was no significant difference in mean heart rate by 24-h dynamic electrocardiogram at week 2 between the IVIG and IVIG + mPSL group (115 ± 22 vs 108 ± 25 beats/min, P = 0.512). Children had higher WBC (15.01 ± 5.52 vs 12.05 ± 6.60, P = 0.014) and N% (58.16 ± 13.80 vs 43.76 ± 17.20, P = 0.000) at week 2 in the IVIG + mPSL group than those in the IVIG group. Other laboratory indicators were similar between the two groups. No coronary artery thrombus was found by echocardiography.
Discussion
The present study showed that a modified mPSL regimen plus IVIG as an intensive initial treatment can be safe and effective in decreasing LCX dilation for high-risk refractory KD patients. The therapy not only decreased the dilation of the LCX but also improved the therapeutic response, shortened the duration of fever, and accelerated the decline of inflammatory marker (CRP) in the early stage of the disease. These findings can be useful in guiding clinicians to individualize treatments for KD patients. Another significant advantage of an intensive initial treatment regimen in high-risk refractory KD patients is the health economics effect. Low-dose corticosteroid application limits the need of expensive IVIG re-use and IVIG-related blood transfusion risks, thus reducing medical costs.
Corticosteroids were considered as a treatment option for KD first reported in 1979.26 The study concluded that corticosteroids could increase the risk of coronary aneurysm, which made the clinical application of corticosteroids controversial in KD patients for a long time. In 2001, Hashino et al. reported that steroid pulse therapy as an additional rescue treatment for IVIG-resistant KD patients had a better prognosis.27 In 2003, the study of Sundel et al. showed that KD patients can benefit from an initial methylprednisolone pulse therapy.28 In a retrospective study in 2009, Kobayashi et al. showed that an initial adjunctive prednisolone treatment was associated with improving clinical and coronary outcomes in high-risk IVIG-resistant KD patients, instead of all KD patients. In 2012, they showed that an initial adjunctive prednisolone improved coronary outcomes in high-risk IVIG-resistant KD patients in Japan in a randomized controlled trial.20,23 Based on the above studies, we have found that initial adjuvant treatment with corticosteroids seems to help reduce the probability of coronary artery disease and treatment failure in KD patients.
The assessment of the efficacy of corticosteroids, as an initial therapy with IVIG in KD, was previously conducted with patients as the study object, taking into account all coronary artery lesions in the patient. If the difference in one of the coronary arteries showed statistical significance, the patient was considered.6,23,27 With further study, each coronary artery became the object of study.20 Due to the special location of LCX and technical difficulties of echocardiography to detect LCX, compared with the other three coronary arteries (LMCA, LAD, and RCA), LCX has been least reported. However, it does not mean that LCX is not important. In our study, we analyzed the efficacy of corticosteroid application on each coronary artery. The study is sufficiently powered to prove the improvement of LCX dilation at week 2, but it was not powered enough for other coronary arteries such as LMCA, RCA, and LAD. The patients in this study had mild coronary dilatation in two groups after propensity-score matching. It showed that our modified therapeutic regimen affected the diameter and dilation of all the coronary arteries; however, it was only statistically significant in decreasing LCX dilation at week 2. So far, there are many reports on LAD and RCA in KD patients with severe coronary artery complications.20,21,22 Does it have the same efficacy on all coronary arteries or have different effect on coronary arteries with different degrees of lesions when initial treatment started? Or it may due to lack of power? Further research is needed. Our research is still ongoing, and we will continue to summarize the results and answer these questions.
The use of corticosteroids, including doses, routes, and patients for initial treatment of KD, still requires further research. Since 2009, there have been reported several therapeutic regimens for high-risk IVIG-resistant KD patients. One is intravenous methylprednisolone pulse therapy (30 mg/kg over 2 h) and the other one is intravenous prednisolone (2 mg/kg/day, divided into 3 doses) until the fever resolved, followed by oral prednisolone until CRP levels normalized (<5 mg/L), and then prednisolone was tapered over 15 days in 5-day steps, from 2 to 1 to 0.5 mg/kg/day.
Okubo et al.29 conducted a retrospective study and found a shorter total length of hospital stay in the high-dose (methylprednisolone 10–40 mg/kg/day) corticosteroid group and similar risks of coronary artery lesions, readmissions, and total hospitalization costs between the normal-dose (prednisolone 0.5–4.0 mg/kg/day) and the high-dose corticosteroid groups for patients with KD. It was found in our clinical practice that single-pulsed dose intravenous methylprednisolone could cause temporary elevation of blood pressure and/or temporarily elevated blood glucose, while the second therapy did not modifiy the dose of glucocorticoid according to the change of the coronary artery diameter. The most recent American Heart Association guidelines note that a longer course of corticosteroids may be considered in high-risk patients as primary adjunctive therapy or in IVIG-resistant cases.1 However, it was found that some patients with high-risk IVIG resistance identified by our self-developed scoring system still had fever when they were given the same dose of methylprednisolone for 2 mg/kg/day, which was most frequently used in previous literature29,30,31 in our clinical practice. Therefore, we decided to choose methylprednisolone in the range 2–4 mg/kg/day in the present study. Different doses of methylprednisolone were given depending on the scores evaluated by our self-developed scoring system. We modified treatment strategy as follows: methylprednisolone intravenous injection 2–4 mg/kg/day, divided into 2–3 doses for 3–5 days, then 1 mg/kg/day, once a day for 3–5 days until the fever resolved and CRP normalized, then oral prednisone was tapered over 3–5 weeks in 5–7 days steps. The course of oral prednisone depends on the changes in the coronary artery diameter. When coronary arteries were progressively dilating, the course of the treatment was 7 days in each step; otherwise it was 5 days in the present study, which was demonstrated to be safe and effective in the 12-week study period.
Although patients were treated with different doses, they belong to the same therapeutic range (normal dose, not high dose) which was the most appropriate individual dose for each patient. Those two doses have the same therapeutic effects with regard to the duration of fever, CRP, and coronary artery recovery ratio. When potential costs and possible adverse events were considered, initial glucocorticoid doses <4 mg/kg/day may be sufficient. This study provides an alternative therapeutic regimen for high-risk refractory KD patients in a real-world study.
Emerging data suggest that patients at particularly high risk for development of coronary artery lesions may benefit from the early use of corticosteroids as primary adjunctive therapy with IVIG and ASA. Although several scoring systems have been developed to predict IVIG resistance, most of which were derived from Japan, these systems are insufficiently useful in other populations, which might be attributed to geographical location and racial heterogeneity. For example, in the most widely used Kobayashi scoring system, the sensitivity and specificity were 86% and 68%, respectively, in the Japanese population. However, it was not suitable for the North American (sensitivity of 33% and specificity of 87%),32 the British (sensitivity of 58% and specificity of 35%),12 and the Italian (sensitivity of 64% and specificity of 62.5%).33 It is also insufficiently useful for Asian populations, such as North Chinese (sensitivity of 16–49% and specificity of 72–86%),34,35 East Chinese (sensitivity of 57% and specificity of 88%),36 Singaporean (sensitivity of 21% and specificity of 62%),37 and Korean (sensitivity of 31% and specificity of 83%).38 Sano et al. scoring system13 was more specific (81–95%), while less sensitive (20.7–60%) in Asian KD patients, such as China, Japan, and Korea.14,15,16 Formosa scoring system’s17 sensitivity and specificity in our population were <50%.24 In order to develop a predictive tool for the efficacy of IVIG therapy in children with KD in Beijing, China, we conducted our previous study and validated a new predictive scoring system for IVIG-resistant KD in our population (sensitivity of 56% and specificity of 79%).24
The present study used the self-developed scoring system, which is more applicable for identifying high-risk IVIG-resistant KD patients in the local population. Studies have shown that IVIG resistance in KD patients is associated with coronary artery complications. In our present study, the proportion of coronary artery abnormality in high-risk IVIG-resistant children selected by our predictive system is as high as 36.9% (62/168), suggesting that children with a coronary abnormality can be selected early, and an initial individualized treatment can improve the prognosis of coronary complications.
The therapeutic response rate predicted how many patients would need secondary therapy. Further analysis of secondary therapy manifested that 88% (22/25) of patients in the IVIG group were treated with glucocorticoids (alone or in combination with IVIG), suggesting that glucocorticoids might be more effective when used as early as possible in refractory KD.
The side effects of corticosteroids include thrombocytosis, increased blood viscosity and fibrinogen concentration, glucose metabolism, and water and salt metabolism disorders. These side effects mainly occur in children with long-term and high-dose corticosteroids. The usage of methylprednisolone regimen in the present study was short term and low dose. The blood pressure, heart rate, biochemistry, and blood coagulation index were monitored during the study, and no abnormality was observed, which indicates our regimen is most likely safe.
However, the study has the following limitations. First, this study is a real-world cohort study, and the number of missing cases increased with the prolongation of follow-up time. The bias occurred when patients were randomized by parental choice. We used propensity-score matching to analyze patients with similar baseline characteristics, which lead to a reduced number of patients included in both groups. Our finding was only in LCX, which may due to the lack of power, and could not completely reflect the real-world situation since not all patients (especially the more severe patients) were included. Second, this is a single-center study. Because of the unbalanced distribution of cases and baseline differences, mild coronary abnormalities were compared after matching the propensity scores, while for the small number (total seven cases described in the text) of moderate to severe coronary abnormalities, further analysis was not conducted. However, it may be an important part. Therefore, the current results are mainly applicable for KD patients with mild coronary abnormalities, and the prognosis of moderate or severe coronary abnormalities needs to be further studied in larger populations.
Conclusion
The present study showed that a modified mPSL regimen plus IVIG as an intensive initial treatment has minimal side effects. It might improve the initial response to IVIG and decrease the dilation of LCX in KD patients with IVIG resistance identified by our self-developed scoring system.
References
McCrindle, B. W. et al. Diagnosis, treatment, and long-term management of kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation 135, e927–e999 (2017).
Yeung, R. S. Kawasaki disease: update on pathogenesis. Curr. Opin. Rheumatol. 22, 551–560 (2010).
Kim, J. Y. & Kim, H. J. A case of Kawasaki disease with coronary aneurysm responding to the 4th IVIG treatment. Case Rep. Cardiol. 2014, 821812 (2014).
Burns, J. C., Capparelli, E. V., Brown, J. A., Newburger, J. W. & Glode, M. P. Intravenous gamma-globulin treatment and retreatment in Kawasaki disease. Pediatr. Infect. Dis. J. 17, 1144–1148 (1998).
Adachi, S. et al. High regression rate of coronary aneurysms developed in patients with immune globulin-resistant Kawasaki disease treated with steroid pulse therapy. Tohoku J. Exp. Med. 220, 285–290 (2010).
Wardle, A. J., Connolly, G. M., Seager, M. J. & Tulloh, R. M. Corticosteroids for the treatment of Kawasaki disease in children. Cochrane Database Syst. Rev. 1, CD011188 (2017).
Hur, G. et al. Infliximab treatment for intravenous immunoglobulin-resistant Kawasaki disease: a multicenter study in Korea. Korean Circ. J. 49, 183–191 (2019).
Suzuki, H. et al. Cyclosporin A treatment for Kawasaki disease refractory to initial and additional intravenous immunoglobulin. Pediatr. Infect. Dis. J. 30, 871–876 (2011).
Tremoulet, A. H. et al. Calcineurin inhibitor treatment of intravenous immunoglobulin-resistant Kawasaki disease. J. Pediatr. 161, 506–512 (2012).
Loomba, R. S., Raskin, A., Gudausky, T. M. & Kirkpatrick, E. Role of the Egami score in predicting intravenous immunoglobulin resistance in Kawasaki disease among different ethnicities. Am. J. Ther. 23, e1293–e1299 (2016).
Kobayashi, T. et al. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation 113, 2606–2612 (2006).
Davies, S. et al. Predicting IVIG resistance in UK Kawasaki disease. Arch. Dis. Child. 100, 366–368 (2015).
Sano, T. et al. Prediction of non-responsiveness to standard high-dose gamma-globulin therapy in patients with acute Kawasaki disease before starting initial treatment. Eur. J. Pediatr. 166, 131–137 (2007).
Ye, X. & Zhang, J. Evaluation of the efficiency of different scoring systems in predicting intravenous immunoglobulin unresponsiveness in Kawasaki disease. Chin. J. Evid. Based Pediatr. 11, 337–340 (2016).
Takeshita, S., Kanai, T., Kawamura, Y., Yoshida, Y. & Nonoyama, S. A comparison of the predictive validity of the combination of the neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio and other risk scoring systems for intravenous immunoglobulin (IVIG) resistance in Kawasaki disease. PLoS ONE 12, e0176957 (2017).
Park, H. M., Lee, D. W., Hyun, M. C. & Lee, S. B. Predictors of nonresponse to intravenous immunoglobulin therapy in Kawasaki disease. Korean J. Pediatr. 56, 75–79 (2013).
Lin, M. T. et al. Risk factors and derived formosa score for intravenous immunoglobulin unresponsiveness in Taiwanese children with Kawasaki disease. J. Formos. Med. Assoc. 115, 350–355 (2016).
Xiao, L. & Zhang, J. Progress of Predictive Scoring Systems of Intravenous Immunoglobulin Unresponsiveness in Children with Kawasaki Disease. J. Pediatr. Pharm. 25, 55–58 (2019).
Qian, W., Tang, Y., Yan, W., Sun, L. & Lv, H. A comparison of efficacy of six prediction models for intravenous immunoglobulin resistance in Kawasaki disease. Ital. J. Pediatr. 44, 33 (2018).
Kobayashi, T. et al. Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (RAISE study): a randomised, open-label, blinded-endpoints trial. Lancet 379, 1613–1620 (2012).
Okada, K. et al. Pulse methylprednisolone with gammaglobulin as an initial treatment for acute Kawasaki disease. Eur. J. Pediatr. 168, 181–185 (2009).
Ogata, S. et al. Corticosteroid pulse combination therapy for refractory Kawasaki disease: a randomized trial. Pediatrics 129, e17–e23 (2012).
Kobayashi, T. et al. Risk stratification in the decision to include prednisolone with intravenous immunoglobulin in primary therapy for Kawasaki disease. Pediatr. Infect. Dis. J. 28, 498–502 (2009).
Yang, S., Song, R., Zhang, J., Li, X. & Li, C. Predictive tool for intravenous immunoglobulin resistance of Kawasaki disease in Beijing. Arch. Dis. Child. 104, 262–267 (2019).
Kobayashi, T. et al. A new Z score curve of the coronary arterial internal diameter using the lambdamusigma method in a pediatric population. J. Am. Soc. Echocardiogr. 29, 794–801 (2016).
Kato, H., Koike, S. & Yokoyama, T. Kawasaki disease: effect of treatment on coronary artery involvement. Pediatrics 63, 175–179 (1979).
Hashino, K., Ishii, M., Iemura, M., Akagi, T. & Kato, H. Re-treatment for immune globulin-resistant Kawasaki disease: a comparative study of additional immune globulin and steroid pulse therapy. Pediatr. Int. 43, 211–217 (2001).
Sundel, R. P., Baker, A. L., Fulton, D. R. & Newburger, J. W. Corticosteroids in the initial treatment of Kawasaki disease: report of a randomized trial. J. Pediatr. 142, 611–616 (2003).
Okubo, Y. et al. Association between dose of glucocorticoids and coronary artery lesions in Kawasaki disease. Arthritis Care Res. 70, 1052–1057 (2018).
Chen, S. et al. Coronary artery complication in Kawasaki disease and the importance of early intervention: a systematic review and Meta-analysis. JAMA Pediatr. 170, 1156–1163 (2016).
Chang, L. S. & Kuo, H. C. The role of corticosteroids in the treatment of Kawasaki disease. Expert Rev. Anti Infect. Ther. 18, 155–164 (2020).
Sleeper, L. A. et al. Evaluation of Kawasaki disease risk-scoring systems for intravenous immunoglobulin resistance. J. Pediatr. 158, 831–835. e3 (2011).
Fabi, M. et al. Inability of Asian risk scoring systems to predict intravenous immunoglobulin resistance and coronary lesions in Kawasaki disease in an Italian cohort. Eur. J. Pediatr. 178, 315–322 (2019).
Fu, P. P., Du, Z. D. & Pan, Y. S. Novel predictors of intravenous immunoglobulin resistance in Chinese children with Kawasaki disease. Pediatr. Infect. Dis. J. 32, e319–e323 (2013).
Song, R., Yao, W. & Li, X. Efficacy of four scoring systems in predicting intravenous immunoglobulin resistance in children with Kawasaki disease in a children’s hospital in Beijing, North China. J. Pediatr. 184, 120–124 (2017).
Tang, Y. et al. Prediction of intravenous immunoglobulin resistance in Kawasaki disease in an East China population. Clin. Rheumatol. 35, 2771–2776 (2016).
Grignani, R., Rajgor, D. D., Leow, Y. G., Heng, C. K. & Quek, S. C. A novel model for predicting non-responsiveness to intravenous immunoglobulins in Kawasaki disease: the Singapore experience. J. Paediatr. Child Health 55, 962–967 (2019).
Shin, J., Lee, H. & Eun, L. Verification of current risk scores for Kawasaki disease in Korean children. J. Korean Med. Sci. 32, 1991–1996 (2017).
Acknowledgements
This study was supported by the following grants: Science Foundation for Clinical Technical Innovation Project of Beijing Municipal Administration of Hospital (XMLX201612), “Peak Climbing” Talents Development Program of Beijing Hospital Authority (DFL20181301), Key Project of Capital Clinical Characteristic Application Research (Z181100001718189), and Research Project of Capital Institute of Pediatrics (PY-2019-11).
Author information
Authors and Affiliations
Contributions
X.L. conceptualized and designed the study, interpreted the data, and revised it critically for important intellectual content. M.Z. and Y.Z. acquired and analyzed the data, and drafted the initial manuscript. S.Y. contributed to acquire and analyze the data. L.S., A.L. and Y.L. contributed to treatment and follow-up of patients and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Parental/guardian consent was obtained.
Ethics approval
All procedures regarding this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Declaration of Helsinki, as revised in 2008. The study was approved by the Ethics Committee of the Capital Institute of Pediatrics (No. SHERLL 2015040).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhang, M., Zheng, Y., Li, X. et al. Refractory Kawasaki disease: modified methylprednisolone regimen decreases coronary artery dilatation. Pediatr Res 91, 1542–1550 (2022). https://doi.org/10.1038/s41390-021-01576-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01576-6
This article is cited by
-
Aspirin/immune-globulin/methylprednisolone
Reactions Weekly (2022)