Abstract
Introduction
Preterm birth is a leading cause for prolonged length of stay (LOS) in the hospital. In the USA, the rate of preterm birth is around 10.5%, thereby contributing substantially to the burden of hospitalization. The interaction of demographic, financial, and hospital factors with LOS of preterm infants has not been studied.
Objective
To assess the effect of demographic, financial, and hospital factors on LOS of surviving preterm infants born at 23 0/7–36 6/7 weeks of gestational age (GA).
Methods
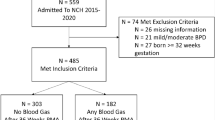
We utilized de-identified patient information from the Healthcare Cost and Utilization Project (HCUP) from 2016–2020. All infants with GA between 23 0/7 and 36 6/7 weeks were identified. ANOVA test was used to assess LOS differences at different GA. Cochran-Armitage test was used for trend analyses.
Results
A total of 1,359,280 surviving premature infants were included in the study. LOS was significantly (p < 0.001) impacted by GA, ethnic group, hospital size and type, and US geographic region. LOS was not affected by sex or type of health insurance.
Conclusion
LOS of preterm infants is significantly affected by multiple demographic factors that are potentially modifiable. These findings can remarkably help policymakers and stakeholders optimize interventions and resource allocations for preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–72. https://doi.org/10.1016/S0140-6736(12)60820-4.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039-51. https://doi.org/10.1001/jama.2015.10244
Glass HC, Costarino AT. Neurological and developmental outcomes for preterm infants in the neonatal intensive care unit. Semin Fetal Neonat Med. 2019;24:176–82.
Behrman RE, Butler AS, editors. Preterm birth: causes, consequences, and prevention. National Academies Press; 2007. https://doi.org/10.17226/11622.
Petrou S, Abangma G. Economic consequences of preterm birth: a systematic review of the recent literature (2009-2017). Arch Dis Child. 2019;104:456–65.
Horbar JD, Carpenter JH, Badger GJ. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129:1019–26.
Battersby C, Statnikov Y, Santhakumaran S, for the Medicines for Neonates Investigator Group. The United Kingdom neonatal collaborative’s framework for practice variation analysis and benchmarking of outcomes in neonatal care. Semin Fetal Neonat Med. 2018;23:316–24.
Valdez LM, Charpak N, DeMauro SB, Hamvas A, Sánchez PJ. Factors associated with length of stay in late preterm infants: an NICHD Neonatal Research Network Study. J Pediatr. 2017;187:144–9.
Aly H, Hoffman H, El-Dib M, Said L, Mohamed M. Factor affecting length of stay in late preterm infants: an US national database study. J Matern Fetal Neonatal Med. 2015;28:598–604.
Narayan S, Aggarwal R, Deorari AK. Factors affecting length of stay in neonatal intensive care unit: a prospective observational study. Indian Pediatr. 2018;55:1029–34.
Profit J, Gould JB, Bennett M, Goldstein BA, Draper D, Phibbs CS, et al. Racial/Ethnic Disparity in NICU Quality of Care Delivery. Pediatrics. 2017;140:e20170918 https://doi.org/10.1542/peds.2017-0918.
Shah PS, Seidlitz W, Chan P, Yeh S, Musrap N, Lee SK, et al. Internal audit of the Canadian Neonatal Network data collection system. BMC Pediatr. 2019;19:83.
Howell EA, Janevic T, Hebert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in morbidity and mortality rates in black, white, and Hispanic very preterm infants among New York City hospitals. JAMA Pediatr. 2018;172:269–77.
Chesley CF, Chowdhury M, Small DS, Schaubel D, Liu VX, Lane-Fall MB, et al. Racial disparities in length of stay among severely Ill patients presenting with sepsis and acute respiratory failure. JAMA Netw Open. 2023;6:e239739 https://doi.org/10.1001/jamanetworkopen.2023.9739.
Qattea I, Farghaly MAA, Kattea MO, Abdula N, Mohamed MA, Aly H. Survival of infants born at periviable gestation: The US national database. Lancet Reg Health Am. 2022;14:100330.
Fröhlich M, Tissen-Diabaté T, Bührer C, Roll S. Sex-specific long-term trends in length of hospital stay, postmenstrual age at discharge, and survival in very low birth weight infants. Neonatology. 2021;118:416–24.
Harrison WN, Wasserman JR, Goodman DC. Regional variation in neonatal intensive care admissions and the relationship to bed supply. J Pediatr. 2019;204:14–20.e1.
Xie F, Shu Q, Chen Z-Y, Li J. Length of stay and influencing factors of NICU in the Western Hunan, an underdeveloped area of China: A 9-year retrospective study. J Int Med Res. 2022;50:3000605221100753. https://doi.org/10.1177/03000605221100753.
Author information
Authors and Affiliations
Contributions
IQ conceptualized and designed the study, conducted the analysis, drafted the initial manuscript, and reviewed the manuscript. RK and SC drafted the initial manuscript and reviewed the manuscript. HA conceptualized and designed the study, interpreted the analysis, drafted the initial manuscript, and reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Qattea, I., Ejaz, S., Kattea, M.O. et al. The effect of demographic, financial and hospital factors on the length of stay of preterm infants: a US national database study. J Perinatol 44, 173–178 (2024). https://doi.org/10.1038/s41372-023-01836-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01836-9