Abstract
Introduction
Maternal body composition may influence fetal body composition.
Objective
The objective of this pilot study was to investigate the relationship between maternal and fetal body composition.
Methods
Three pregnant women cohorts were studied: healthy, gestational diabetes (GDM), and fetal growth restriction (FGR). Maternal body composition (visceral adipose tissue volume (VAT), subcutaneous adipose tissue volume (SAT), pancreatic and hepatic proton-density fat fraction (PDFF) and fetal body composition (abdominal SAT and hepatic PDFF) were measured using MRI between 30 to 36 weeks gestation.
Results
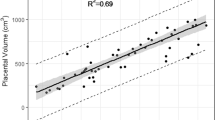
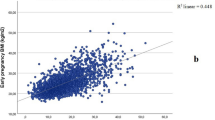
Compared to healthy and FGR fetuses, GDM fetuses had greater hepatic PDFF (5.2 [4.2, 5.5]% vs. 3.2 [3, 3.3]% vs. 1.9 [1.4, 3.7]%, p = 0.004). Fetal hepatic PDFF was associated with maternal SAT (r = 0.47, p = 0.02), VAT (r = 0.62, p = 0.002), and pancreatic PDFF (r = 0.54, p = 0.008). When controlling for maternal SAT, GDM increased fetal hepatic PDFF by 0.9 ([0.51, 1.3], p = 0.001).
Conclusion
In this study, maternal SAT, VAT, and GDM status were positively associated with fetal hepatic PDFF.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that supports the findings of this study are available from the corresponding author upon reasonable request and may require institutional data agreements.
References
Ornoy A. Prenatal origin of obesity and their complications: Gestational diabetes, maternal overweight and the paradoxical effects of fetal growth restriction and macrosomia. Reprod Toxicol. 2011;32:205–12. https://doi.org/10.1016/j.reprotox.2011.05.002.
Johns EC, Denison FC, Norman JE, Reynolds RM. Gestational diabetes mellitus: mechanisms, treatment, and complications. Trends Endocrinol Metab. 2018;29:743–54. https://doi.org/10.1016/j.tem.2018.09.004.
Thorn SR, Rozance PJ, Brown LD, Hay WW. The intrauterine growth restriction phenotype: fetal adaptations and potential implications for later life insulin resistance and diabetes. Semin Reprod Med. 2011;29:225–36.
Ross MG, Desai M. Developmental programming of offspring obesity, adipogenesis, and appetite. Clin Obstet Gynecol. 2013;56:529–36. https://doi.org/10.1097/GRF.0b013e318299c39d.
Kc K, Shakya S, Zhang H. Gestational diabetes mellitus and macrosomia: a literature review. Ann Nutr Metab. 2015;66:14–20. https://doi.org/10.1159/000371628.
Wang Y, He S, He J, Wang S, Liu K, Chen X. Predictive value of visceral adiposity index for type 2 diabetes mellitus: a 15-year prospective cohort study. Herz. 2015;40:277–81. https://doi.org/10.1007/s00059-014-4175-1.
Ly KV, Armstrong T, Yeh J, Ghahremani S, Kim GH, Wu HH, et al. Free-breathing magnetic resonance imaging assessment of body composition in healthy and overweight children: an observational study. J Pediatr Gastroenterol Nutr. 2019;68:782–7. https://doi.org/10.1097/MPG.0000000000002309.
Frondas-Chauty A, Simon L, Flamant C, Hanf M, Darmaun D, Rozé JC. Deficit of fat free mass in very preterm infants at discharge is associated with neurological impairment at age 2 years. J Pediatr. 2018;196:301–4. https://doi.org/10.1016/j.jpeds.2017.12.017.
Borga M, West J, Bell JD, Harvey NC, Romu T, Heymsfield SB, et al. Advanced body composition assessment: from body mass index to body composition profiling. J Investig Med. 2018;66:1–9. https://doi.org/10.1136/jim-2018-000722.
Ross R. Magnetic resonance imaging provides new insights into the characterization of adipose and lean tissue distribution. Can J Physiol Pharm. 1996;74:778–85.
Armstrong T, Ly KV, Ghahremani S, Calkins KL, Wu HH. Free-breathing 3-D quantification of infant body composition and hepatic fat using a stack-of-radial magnetic resonance imaging technique. Pediatr Radiol. 2019;49:876–88. https://doi.org/10.1007/s00247-019-04384-7.
Reeder SB, Hu HH, Sirlin CB. Proton density fat-fraction: a standardized MR-based biomarker of tissue fat concentration. J Magn Reson Imaging. 2012;36:1011–4. https://doi.org/10.1002/jmri.23741.
Yokoo T, Serai SD, Pirasteh A, Bashir MR, Hamilton G, Hernando D, et al. RSNA-QIBA PDFF Biomarker Committee. Linearity, bias, and precision of hepatic proton density fat fraction measurements by using MR imaging: a meta-analysis. Radiology. 2018;286:486–98. https://doi.org/10.1148/radiol.2017170550.
Schwimmer JB, Middleton MS, Behling C, Newton KP, Awai HI, Paiz MN, et al. Magnetic resonance imaging and liver histology as biomarkers of hepatic steatosis in children with nonalcoholic fatty liver disease. Hepatology. 2015;61:1887–95. https://doi.org/10.1002/hep.27666.
Caussy C, Reeder SB, Sirlin CB, Loomba R. Non‐invasive, quantitative assessment of liver fat by MRI‐PDFF as an endpoint in NASH trials. Hepatology. 2018;68:763–772.
Loomba R. MRI-proton density fat fraction treatment response criteria in nonalcoholic steatohepatitis. Hepatology. 2021;73:881–3. https://doi.org/10.1002/hep.31624.
Blondiaux E, Chougar L, Gelot A, Valence S, Audureau E, Ducou le Pointe H, et al. Developmental patterns of fetal fat and corresponding signal on T1-weighted magnetic resonance imaging. Pediatr Radiol. 2018;48:317–24. https://doi.org/10.1007/s00247-017-4038-z.
Victoria T, Jaramillo D, Roberts TP, Zarnow D, Johnson AM, Delgado J, et al. Fetal magnetic resonance imaging: jumping from 1.5 to 3 tesla (preliminary experience). Pediatr Radiol. 2014;44:376–86. https://doi.org/10.1007/s00247-013-2857-0.
Armstrong T, Liu D, Martin T, Masamed R, Janzen C, Wong C, et al. 3D R2* mapping of the placenta during early gestation using free-breathing multiecho stack-of-radial MRI at 3 T. J Magn Reson Imaging. 2019;49:291–303. https://doi.org/10.1002/jmri.26203.
US Preventive Services Task Force, Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, et al. Screening for gestational diabetes: US preventive services task force recommendation statement. JAMA. 2021;326:531–8. https://doi.org/10.1001/jama.2021.11922.
Combs CA, Castillo R, Webb GW, Del Rosario A. Impact of adding abdominal circumference to the definition of fetal growth restriction. Am J Obstet Gynecol MFM. 2021;3:100382. https://doi.org/10.1016/j.ajogmf.2021.100382.
Zhong X, Nickel MD, Kannengiesser SA, Dale BM, Kiefer B, Bashir MR. Liver fat quantification using a multi-step adaptive fitting approach with multi-echo GRE imaging. Magn Reson Med. 2014;72:1353–65. https://doi.org/10.1002/mrm.25054.
Mandava S, Keerthivasan MB, Martin DR, Altbach MI, Bilgin A. Radial streak artifact reduction using phased array beamforming. Magn Reson Med. 2019;81:3915–23. https://doi.org/10.1002/mrm.27689.
Shih S-F, Wu HH. A beamforming-based coil combination method to reduce streaking artifacts and preserve phase fidelity in radial MRI. Proceedings of the ISMRM 30th Annual Meeting, 2022, p1697.
Armstrong T, Ly KV, Murthy S, Ghahremani S, Kim GHJ, Calkins KL, et al. Free-breathing quantification of hepatic fat in healthy children and children with nonalcoholic fatty liver disease using a multi-echo 3-D stack-of-radial MRI technique. Pediatr Radiol. 2018;48:941–53. https://doi.org/10.1007/s00247-018-4127-7.
Armstrong T, Zhong X, Shih SF, Felker E, Lu DS, Dale BM, et al. Free-breathing 3D stack-of-radial MRI quantification of liver fat and R2* in adults with fatty liver disease. Magn Reson Imaging. 2022;85:141–52. https://doi.org/10.1016/j.mri.2021.10.016.
Story JD, Ghahremani S, Kafali SG, Shih S-F, Kuwahara K, Calkins KL, et al. Using free-breathing MRI to quantify pancreatic fat and investigate spatial heterogeneity in children. J Magn Reson Imaging. 2022, in press. https://doi.org/10.1002/jmri.28337. PMID: 35778376.
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics. 2010;125:e214–24. https://doi.org/10.1542/peds.2009-0913.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. https://doi.org/10.1016/j.jbi.2008.08.010.
Berger-Kulemann V, Brugger PC, Reisegger M, Klein K, Hachemian N, Koelblinger C, et al. Quantification of the subcutaneous fat layer with MRI in fetuses of healthy mothers with no underlying metabolic disease vs. fetuses of diabetic and obese mothers. J Perinat Med. 2011;40:179–84. https://doi.org/10.1515/JPM.2011.122.
Giza SA, Olmstead C, McCooeye DA, Miller MR, Penava DA, Eastabrook GD, et al. Measuring fetal adipose tissue using 3D water-fat magnetic resonance imaging: a feasibility study. J Matern Fetal Neonatal Med. 2020;33:831–7. https://doi.org/10.1080/14767058.2018.1506438.
Anblagan D, Deshpande R, Jones NW, Costigan C, Bugg G, Raine-Fenning N, et al. Measurement of fetal fat in utero in normal and diabetic pregnancies using magnetic resonance imaging. Ultrasound Obstet Gynecol. 2013;42:335–40. https://doi.org/10.1002/uog.12382.
Köşüş N, Köşüş A. Can fetal abdominal visceral adipose tissue and subcutaneous fat thickness be used for correct estimation of fetal weight? A preliminary study. J Obstet Gynaecol. 2019;39:594–600. https://doi.org/10.1080/01443615.2018.1530971.
US Preventive Services Task Force, Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, et al. Behavioral counseling interventions for healthy weight and weight gain in pregnancy: US preventive services task force recommendation statement. JAMA. 2021;325:2087–93. https://doi.org/10.1001/jama.2021.6949.
Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. The pathophysiology of gestational diabetes mellitus. Int J Mol Sci. 2018;19:3342. https://doi.org/10.3390/ijms19113342.
Bader J, Carson M, Enos R, Velazquez K, Sougiannis A, Singh U, et al. High-fat diet-fed ovariectomized mice are susceptible to accelerated subcutaneous tumor growth potentially through adipose tissue inflammation, local insulin-like growth factor release, and tumor associated macrophages. Oncotarget. 2020;11:4554–69. https://doi.org/10.18632/oncotarget.27832.
Zhou Y, Zhao R, Lyu Y, Shi H, Ye W, Tan Y, et al. Serum and amniotic fluid metabolic profile changes in response to gestational diabetes mellitus and the association with maternal-fetal outcomes. Nutrients. 2021;13:3644. https://doi.org/10.3390/nu13103644.
Tan K, Tint MT, Michael N, Yap F, Chong YS, Tan KH, et al. Determinants of cord blood adipokines and association with neonatal abdominal adipose tissue distribution. Int J Obes (Lond). 2022;46:637–45. https://doi.org/10.1038/s41366-021-00975-3.
Skinner J, O’Donoghue K, Gardeil F, Greene R, Turner MJ. Is fetal abdominal subcutaneous fat comparable with established indices of growth restriction? J Obstet Gynaecol. 2001;21:439–42. https://doi.org/10.1080/01443610120071947.
Brown LD, Hay WW Jr. Impact of placental insufficiency on fetal skeletal muscle growth. Mol Cell Endocrinol. 2016;435:69–77. https://doi.org/10.1016/j.mce.2016.03.017.
de Fluiter KS, van Beijsterveldt IALP, Breij LM, Acton D, Hokken-Koelega ACS. Association between fat mass in early life and later fat mass trajectories. JAMA Pediatr. 2020;174:1141–8. https://doi.org/10.1001/jamapediatrics.2020.2673.
Ong YY, Sadananthan SA, Aris IM, Tint MT, Yuan WL, Huang JY, et al. Mismatch between poor fetal growth and rapid postnatal weight gain in the first 2 years of life is associated with higher blood pressure and insulin resistance without increased adiposity in childhood: the GUSTO cohort study. Int J Epidemiol. 2020;49:1591–603. https://doi.org/10.1093/ije/dyaa143.
Rolland-Cachera MF, Péneau S. Growth trajectories associated with adult obesity. World Rev Nutr Diet. 2013;106:127–34. https://doi.org/10.1159/000342564.
Sinclair KJ, Friesen-Waldner LJ, McCurdy CM, Wiens CN, Wade TP, de Vrijer B, et al. Quantification of fetal organ volume and fat deposition following in utero exposure to maternal Western Diet using MRI. PLoS One. 2018;13:e0192900. https://doi.org/10.1371/journal.pone.0192900.
Huang SW, Ou YC, Tang KS, Yu HR, Huang LT, Tain YL, et al. Metformin ameliorates maternal high-fat diet-induced maternal dysbiosis and fetal liver apoptosis. Lipids Health Dis. 2021;20:100 https://doi.org/10.1186/s12944-021-01521-w.
Wang YW, Yu HR, Tiao MM, Tain YL, Lin IC, Sheen JM, et al. Maternal obesity related to high fat diet induces placenta remodeling and gut microbiome shaping that are responsible for fetal liver lipid dysmetabolism. Front Nutr. 2021;8:736944. https://doi.org/10.3389/fnut.2021.736944.
Chang GQ, Gaysinskaya V, Karatayev O, Leibowitz SF. Maternal high-fat diet and fetal programming: increased proliferation of hypothalamic peptide-producing neurons that increase risk for overeating and obesity. J Neurosci. 2008;28:12107–19. https://doi.org/10.1523/JNEUROSCI.2642-08.2008.
Kislal S, Shook LL, Edlow AG. Perinatal exposure to maternal obesity: Lasting cardiometabolic impact on offspring. Prenat Diagn. 2020;40:1109–25. https://doi.org/10.1002/pd.5784.
Lindberger E, Wikström AK, Bergman E, Eurenius K, Mulic-Lutvica A, Sundström Poromaa I, et al. Association of maternal central adiposity measured by ultrasound in early mid pregnancy with infant birth size. Sci Rep. 2020;10:19702. https://doi.org/10.1038/s41598-020-76741-8.
Jarvie EM, Stewart FM, Ramsay JE, Brown EA, Meyer BJ, Olivecrona G, et al. Maternal adipose tissue expansion, a missing link in the prediction of birth weight centile. J Clin Endocrinol Metab. 2020;105:dgz248. https://doi.org/10.1210/clinem/dgz248.
Paula VG, Sinzato YK, de Moraes-Souza RQ, Soares TS, Souza FQG, Karki B, et al. Metabolic changes in female rats exposed to intrauterine hyperglycemia and postweaning consumption of high-fat diet†. Biol Reprod. 2022;106:200–12. https://doi.org/10.1093/biolre/ioab195.
Haghiac M, Basu S, Presley L, Serre D, Catalano PM, Hauguel-de Mouzon S. Patterns of adiponectin expression in term pregnancy: impact of obesity. J Clin Endocrinol Metab. 2014;99:3427–34. https://doi.org/10.1210/jc.2013-4074.
Ikenoue S, Kasuga Y, Endo T, Tanaka M, Ochiai D. Newer insights into fetal growth and body composition. Front Endocrinol (Lausanne). 2021;12:708767. https://doi.org/10.3389/fendo.2021.708767.
Catalano PM, Thomas A, Huston-Presley L, Amini SB. Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol. 2003;189:1698–704. https://doi.org/10.1016/s0002-9378(03)00828-7.
Brumbaugh DE, Tearse P, Cree-Green M, Fenton LZ, Brown M, Scherzinger A, et al. Intrahepatic fat is increased in the neonatal offspring of obese women with gestational diabetes. J Pediatr. 2013;162:930–6.e1. https://doi.org/10.1016/j.jpeds.2012.11.017.
Shulman M, Cho E, Aasi B, Cheng J, Nithiyanantham S, Waddell N, et al. Quantitative analysis of fetal magnetic resonance phantoms and recommendations for an anthropomorphic motion phantom. MAGMA. 2020;33:257–72. https://doi.org/10.1007/s10334-019-00775-x.
Satkunasingham J, Nik HH, Fischer S, Menezes R, Selzner N, Cattral M, et al. Can negligible hepatic steatosis determined by magnetic resonance imaging-proton density fat fraction obviate the need for liver biopsy in potential liver donors? Liver Transpl. 2018;24:470–7. https://doi.org/10.1002/lt.24965.
Acknowledgements
The authors would like to acknowledge Dr. Carla Janzen, Dr. Michelle Tsai, Dr. Alexandra Havard, Dr. Ilina Pluym, and Dr. Thalia Wong who assisted with recruitment and provided insight into maternal data. The authors would also like to thank the MRI technologists at University of California Los Angeles for assisting with the study.
Funding
KMS received research support from University of California Los Angeles Children’s Discovery Institute. HHW and KLC received funding from NIH/NIDDK R01-124417-01.
Author information
Authors and Affiliations
Contributions
KMS, HHW, and KLC conceptualized and designed the study. KMS recruited and consented all subjects. KMS, SS, SGK, AA, and RM assisted with data collection and interpretation. KMS performed all the data analysis under guidance of DE. KMS wrote the initial draft of the manuscript. All authors edited and approved the final draft of the manuscript. KLC had the primary responsibility for the final content.
Corresponding author
Ethics declarations
Competing interests
KLC has received research support from Fresenius Kabi. KLC has served as an advisor for Fresenius Kabi, Mead Johnson, Baxter, and Prolacta. KLC serves as an institutional principal investigator, with no salary funding, for a consortium database sponsored by Mead Johnson. HHW receives research support from Siemens Medical Solutions USA.
Ethics approval and consent to participate
The University of California Los Angeles Institutional review board approved the study. Each participant participated with informed consent. The study was performed in accordance with Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Strobel, K.M., Kafali, S.G., Shih, SF. et al. Pregnancies complicated by gestational diabetes and fetal growth restriction: an analysis of maternal and fetal body composition using magnetic resonance imaging. J Perinatol 43, 44–51 (2023). https://doi.org/10.1038/s41372-022-01549-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01549-5