Abstract
Background
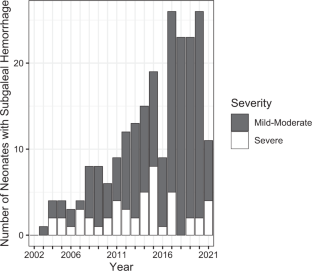
In 2011, we reported 38 neonates with subgaleal hemorrhage (SH), relating an increasing incidence. It is unclear whether the incidence in our hospitals continued to rise and which risk factors and outcomes are associated with this condition.
Design
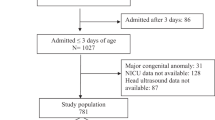
We retrospectively analyzed every recognized case of SH in our hospitals from the end of our previous report (2010) to the present (2022). We redescribed the incidence, scored severity, tabulated blood products transfused, and recorded outcomes.
Results
Across 141 months, 191 neonates were diagnosed with SH; 30 after vacuum or forceps. The incidence (one/1815 births) was higher than in our 2011 report (one/7124 births). Also, severe SH (requiring transfusion) was more common (one/10,033 births vs. one/20,950 births previously). Four died (all with severe SH) and 12 had neurodevelopmental impairment.
Conclusion
Recognized cases of SH are increasing in our system without a clear explanation. Adverse outcomes are rare but continue to occur.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
A deidentified dataset is available by written request to the corresponding author.
References
Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health. 1996;32:228–32.
Levin G, Mankuta D, Eventov-Friedman S, Ezra Y, Koren A, Yagel S, et al. Factors associated with the severity of neonatal subgaleal haemorrhage following vacuum assisted delivery. Eur J Obstet Gynecol Reprod Biol. 2020;245:205–9.
Levin G, Elchalal U, Yagel S, Eventov-Friedman S, Ezra Y, Sompolinsky Y, et al. Risk factors associated with subgaleal hemorrhage in neonates exposed to vacuum extraction. Acta Obstet Gynecol Scand. 2019;98:1464–72.
Boo NY, Foong KW, Mahdy ZA, Yong SC, Jaafar R. Risk factors associated with subaponeurotic haemorrhage in full-term infants exposed to vacuum extraction. BJOG 2005;112:1516–21.
Lee SJ, Kim JK, Kim SJ. The clinical characteristics and prognosis of subgaleal hemorrhage in newborn. Korean J Pediatr. 2018;61:387–91.
Kilani RA, Wetmore J. Neonatal subgaleal hematoma: presentation and outcome—radiological findings and factors associated with mortality. Am J Perinatol. 2006;23:41–8.
Uchil D, Arulkumaran S. Neonatal subgaleal hemorrhage and its relationship to delivery by vacuum extraction. Obstet Gynecol Surv. 2003;58:687–93.
Swanson AE, Veldman A, Wallace EM, Malhotra A. Subgaleal hemorrhage: risk factors and outcomes. Acta Obstet Gynecol Scand 2012;91:260–3.
Liu LY, Antaya RJ. Neonatal subgaleal hematoma from trauma during vaginal delivery without instrument use. Pediatr Dermatol 2017;34:e40–e41.
El-Dib M, Parziale MP, Johnson L, Benson CB, Grant PE, Robinson J, et al. Encephalopathy in neonates with subgaleal hemorrhage is a key predictor of outcome. Pediatr Res. 2019;86:234–41.
Levin G, Mankuta D, Eventov-Friedman S, Ezra Y, Elchalal U, Yagel S, et al. Neonatal subgaleal hemorrhage unrelated to assisted vaginal delivery: clinical course and outcomes. Arch Gynecol Obstet. 2020;301:93–9.
Rohyans JA, Miser AW, Miser JS. Subgaleal hemorrhage in infants with hemophilia: report of two caes and review of the literature. Pediatrics 1982;70:306–7.
Wetzel EA, Kingma PS. Subgaleal hemorrhage in a neonate with factor X deficiency following a non-traumatic cesarean section. J Perinatol 2012;32:304–5.
Christensen RD, Baer VL, Henry E. Neonatal subgaleal hemorrhage in a multihospital healthcare system: prevalence, associations, and outcomes. E J Neo Res. 2011;1:1–8.
Bahr TM, Kerry BB, Baserga MC, Christensen RD. Improving thermoregulation in transported preterm infants. J Perinatol. 2021;41:356–7.
Hulse W, Bahr TM, Fredrickson L, Canfield CM, Friddle K, Pysher TJ, et al. Warming blood products for transfusion to neonates: In vitro assessments. Transfusion 2020;60:1924–8.
Plauche. Subgaleal hematoma. A complication of instrumental delivery. JAMA 1980;244:1597–8.
Hünseler C, Kribs A, Eifinger F, Roth B. Recombinant activated factor seven in acute life-threatening bleeding in neonates: report on three cases and review of literature. J Perinatol. 2006;26:706–13.
Strauss T, Kenet G, Schushan-Eisen I, Mazkereth R, Kuint J. Rescue recombinant activated factor VII for neonatal subgaleal hemorrhage. Isr Med Assoc J. 2009;11:639–40.
Legge N, Guaran R. Critical bleeding protocol for infants used for a catastrophic subgaleal hemorrhage. J Paed Child Health. 2022;58:542–5.
Gertler R, Grubler M, Grassin-Delyle, Urien S, Martin K, Tassani-Prell P, et al. Pharmacokinetics of tranexamic acid in neonates and infants undergoing cardiac surgery. Br J Clin Pharm. 2017;83:1745–57.
Devereaux PJ, Marcucci M, Painter TW, Conen D, Lomivorotov V, Sessler DI, et al. Tranexamic acid in patients undergoing noncardiac surgery. N. Engl J Med. 2022;26:386 1986–97.
Vanderspurt CK, Spinella PC, Cap AP, Hill R, Matthews SA, Corley JB, et al. The use of whole blood in US military operations in Iraq, Syria, and Afghanistan since the introduction of low-titer Type O whole blood: feasibility, acceptability, challenges. Transfusion 2019;59:965–70.
Bahr TM, DuPont TL, Morris DS, Pierson SE, Esplin MS, Brown SM, et al. First report of using low-titer cold-stored type O whole blood in massive postpartum hemorrhage. Transfusion 2019;59:3089–92.
Carr NR, Henry E, Bahr TM, Ohls RK, Page JM, Ilstrup SJ, et al. Fetomaternal hemorrhage: Evidence from a multihospital healthcare system that up to 40% of severe cases are missed. Transfusion 2022;62:60–70.
Carr NR, Hulse WL, Bahr TM, Davidson JM, Ilstrup SJ, Christensen RD First report of transfusing low-titer cold-stored type O whole blood to an extremely-low-birth-weight neonate after acute blood loss. Transfusion. 2022. https://doi.org/10.1111/trf.17034.
Jacquot C, Mo YD, Luban NLC Transfusion Practices. In Neonatal Hematology, 3rd Edition. Eds, de Alarcon PA, Werner EJ, Christensen RD, Sola-Visner MC Cambridge Medicine, Cambridge UK, 2021; pp 329–66.
Leeper CM, Yazer MH, Triulzi DJ, Neal MD, Gaines BA. Whole blood is superior to component transfusion for injured children: A propensity matched analysis. Ann Surg. 2020;272:590–4.
Leeper CM, Yazer MH, Cladis FP, Saladino R, Triulzi DJ, Gaines BA. Cold-stored whole blood platelet function is preserved in injured children with hemorrhagic shock. J Trauma Acute Care Surg. 2019;87:49–53.
Leeper CM, Yazer MH, Morgan KM, Triulzi DJ, Gaines BA. Adverse events after low titer group O whole blood versus component product transfusion in pediatric trauma patients: A propensity-matched cohort study. Transfusion. 2021;61:2621–8.
Morgan KM, Yazer MH, Triulzi DJ, Strotmeyer S, Gaines BA, Leeper CM. Safety profile of low-titer group O whole blood in pediatric patients with massive hemorrhage. Transfusion. 2021;61:S8–s14.
Salazar EG, Handley SC, Greenberg LT, Edwards EM, Lorch SA Measuring quality of care in moderate and late preterm infants. J Perinatol. 2022. https://doi.org/10.1038/s41372-022-01.
Bi SY, Yu YH, Li C, Xu P, Xu HY, Li JH, et al. A standardized implementation of multicenter quality improvement program of very low birth weight newborns could significantly reduce admission hypothermia and improve outcomes. BMC Pediatr. 2022;14:281. 22.
Hausfeld K, Baker RB, Boettcher-Prior P, Hancock D, Helms C, Jablonski T, et al. Randomized prospective clinical trial comparing room temperature and warmed intravenous fluid boluses on pediatric patients’ comfort. J Pediatr Nurs. 2015;30:e3–9.
Blumenberg A. Dosing heat: expected core temperature change with warmed or cooled intravenous fluids. Ther Hypothermia Temp Manag 2021;11:223–9.
Nair SS, Sreedevi V, Nagesh DS. Warming of blood and intravenous fluids using low-power infra-red light-emitting diodes. J Med Eng Technol. 2021;45:614–26.
Mattson MK, Groves C, Smith MM, Christensen JM, Chen D, Stubbs JR, et al. Platelet transfusion: The effects of a fluid warmer on platelet function. Transfusion 2021;61:52–6.
Patel S, Ohls RK. Darbepoetin administration in term and preterm neonates. Clin Perinatol. 2015;42:557–66.
Ohls RK, Kamath-Rayne BD, Christensen RD, Wiedmeier SE, Rosenberg A, Fuller JA, et al. Cognitive outcomes of preterm infants randomized to darbepoetin, erythropoietin or placebo. Pediatrics 2014;133:1023–30.
Ohls RK, Cannon DC, Phillips J, Caprihan A, Patel S, Winter S, et al. Preschool assessment of preterm infants treated with darbepoetin and erythropoietin. Pediatrics 2016;137:1–9.
Burd J, Gomez J, Berghella V, Bellussi F, de Vries B, Phipps H, et al. Prophylactic rotation for malposition in the second stage of labor: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol MFM 2022;4:100554 https://doi.org/10.1016/j.ajogmf.2021.100554. Epub 2022 Feb 6.
Acknowledgements
The authors thank Molly Adams, Intermountain Healthcare Women and Newborn’s Research Department, for assistance with Institutional Review Board communications.
Author information
Authors and Affiliations
Contributions
TRC: conceptualization, investigation, data curation, and review of final manuscript. TMB: conceptualization, investigation, data curation, data analysis, and review of final manuscript. EH: investigation, data curation, and review of final manuscript. CL: conceptualization and review of final manuscript. THH: conceptualization, investigation, data curation, and review of final manuscript. JMP: conceptualization and review of final manuscript. SJL: investigation, data curation, and review of final manuscript. NRC: conceptualization and review of final manuscript. RKO: conceptualization and review of final manuscript. RDC: conceptualization, investigation, data curation, initial draft of manuscript, and review of final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Christensen, T.R., Bahr, T.M., Henry, E. et al. Neonatal subgaleal hemorrhage: twenty years of trends in incidence, associations, and outcomes. J Perinatol 43, 573–577 (2023). https://doi.org/10.1038/s41372-022-01541-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01541-z