Abstract
Fortification of human milk is the standard of care for very low birth weight (VLBW) infants and is required to support adequate postnatal growth and development. Achieving adequate growth velocity and preventing growth faltering is critical for the developing neonatal brain and optimizing long-term neurodevelopmental outcomes. Mother’s milk is the gold standard nutrition to feed preterm infants, however, it does not provide the nutrients needed to support the growth of VLBW infants. After the decision is made to use mother’s milk (if available) or alternatively, donor human milk, many dilemmas exist with regards to additional treatment decisions surrounding the type of fortification to use, when to fortify, and the duration of fortification. In this article, we will review the differences in mother’s milk compared to donor milk, the different types of human milk fortifiers, the optimal timing of fortification, and discuss when to discontinue human milk fortification.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Eidelman AI. Breastfeeding and the use of human milk: an analysis of the American Academy of Pediatrics 2012 Breastfeeding Policy Statement. Breastfeed Med: Off J Acad Breastfeed Med. 2012;7:323–4.
Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Wright LL, Langer JC, et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics. 2006;118:e115–123.
Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Higgins RD, Langer JC, et al. Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes of extremely low birth weight infants at 30 months of age. Pediatrics. 2007;120:e953–9.
Brown JVE, Walsh V, McGuire W. Formula versus maternal breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev. 2019;8:Cd002972.
Schanler RJ. Evaluation of the evidence to support current recommendations to meet the needs of premature infants: the role of human milk. Am J Clin Nutr. 2007;85:625s–8s.
Fenton TR, Cormack B, Goldberg D, Nasser R, Alshaikh B, Eliasziw M, et al. “Extrauterine growth restriction” and “postnatal growth failure” are misnomers for preterm infants. J Perinatol. 2020;40:704–14.
Chou FS, Pandey V, Yeh HW. Postnatal growth in extremely low birth weight newborns: nature or nurture? J Perinatol. 2021;41:648–9.
Belfort MB, Ramel SE. NICU diet, physical growth and nutrient accretion, and preterm infant brain development. Neoreviews. 2019;20:e385–96.
Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010;50:85–91.
Fenton TR, Griffin IJ, Groh-Wargo S, Gura K, Martin CR, Taylor SN, et al. Very low birthweight preterm infants: a 2020 evidence analysis center evidence-based nutrition practice guideline. J Acad Nutr Diet. 2022;122:182–206.
Gidrewicz DA, Fenton TR. A systematic review and meta-analysis of the nutrient content of preterm and term breast milk. BMC Pediatr. 2014;14:216.
Quigley M, Embleton ND, McGuire W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev. 2019;7:Cd002971.
Goldberg DL, Becker PJ, Brigham K, Carlson S, Fleck L, Gollins L, et al. Identifying malnutrition in preterm and neonatal populations: recommended indicators. J Acad Nutr Diet. 2018;118:1571–82.
Brown JV, Embleton ND, Harding JE, McGuire W. Multi-nutrient fortification of human milk for preterm infants. Cochrane Database Syst Rev. 2016;5:Cd000343.
Fenton TR, Groh-Wargo S, Gura K, Martin CR, Taylor SN, Griffin IJ, et al. Effect of enteral protein amount on growth and health outcomes in very-low-birth-weight preterm infants: phase II of the pre-B project and an evidence analysis center systematic review. J Acad Nutr Diet. 2021;121:2287–2300.e2212.
Taylor SN, Martin CR. Evidence-based discharge nutrition to optimize preterm infant outcomes. Neoreviews. 2022;23:e108–e116.
Rustico SE, Calabria AC, Garber SJ. Metabolic bone disease of prematurity. J Clin Transl Endocrinol. 2014;1:85–91.
Faienza MF, D’Amato E, Natale MP, Grano M, Chiarito M, Brunetti G. et al. Metabolic bone disease of prematurity: diagnosis and management. Front Pediatr. 2019;7:143.
Kositamongkol S, Suthutvoravut U, Chongviriyaphan N, Feungpean B, Nuntnarumit P. Vitamin A and E status in very low birth weight infants. J Perinatol. 2011;31:471–6.
Mactier H, Weaver LT. Vitamin A and preterm infants: what we know, what we don’t know, and what we need to know. Arch Dis Child Fetal Neonatal Ed. 2005;90:F103–108.
Mactier H, McCulloch DL, Hamilton R, Galloway P, Bradnam MS, Young D, et al. Vitamin A supplementation improves retinal function in infants at risk of retinopathy of prematurity. J Pediatr. 2012;160:954–9.e951.
Shenai JP. Vitamin A supplementation in very low birth weight neonates: rationale and evidence. Pediatrics. 1999;104:1369–74.
Greer FR. Feeding the premature infant in the 20th century. J Nutr. 2001;131:426s–30s.
American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–841.
Arslanoglu S, Corpeleijn W, Moro G, Braegger C, Campoy C, Colomb V, et al. Donor human milk for preterm infants: current evidence and research directions. J Pediatr Gastroenterol Nutr. 2013;57:535–42.
American Academy of Pediatrics Committee on Nutrition, Section on Breastfeeding, Committee on Fetus and Newborn. Donor human milk for the high-risk infant: preparation, safety, and usage options in the united states. Pediatrics. 2017;139:e20163440.
Meier P, Patel A, Esquerra-Zwiers A. Donor human milk update: evidence, mechanisms, and priorities for research and practice. J Pediatr. 2017;180:15–21.
Friend LL, Perrin MT. Fat and protein variability in donor human milk and associations with milk banking processes. Breastfeed Med: Off J Acad Breastfeed Med. 2020;15:370–6.
Burge K, Vieira F, Eckert J, Chaaban H. Lipid composition, digestion, and absorption differences among neonatal feeding strategies: potential implications for intestinal inflammation in preterm infants. Nutrients. 2021;13:550.
Arslanoglu S, Boquien CY, King C, Lamireau D, Tonetto P, Barnett D, et al. Fortification of human milk for preterm infants: update and recommendations of the European Milk Bank Association (EMBA) Working Group on human milk fortification. Front Pediatr. 2019;7:76.
Koo W, Tice H. Human milk fortifiers do not meet the current recommendation for nutrients in very low birth weight infants. J Parenter Enter Nutr. 2018;42:813–20.
Barrington KJ, Fortin-Pellerin E, Pennaforte T. Fluid restriction for treatment of preterm infants with chronic lung disease. Cochrane Database Syst Rev. 2017;2:Cd005389.
Sullivan S, Schanler RJ, Kim JH, Patel AL, Trawoger R, Kiechl-Kohlendorfer U, et al. An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J Pediatr. 2010;156:562–7.e561.
Cristofalo EA, Schanler RJ, Blanco CL, Sullivan S, Trawoeger R, Kiechl-Kohlendorfer U, et al. Randomized trial of exclusive human milk versus preterm formula diets in extremely premature infants. J Pediatr. 2013;163:1592–5.e1.
Hair AB, Rechtman DJ, Lee ML, Niklas V. Beyond necrotizing enterocolitis: other clinical advantages of an exclusive human milk diet. Breastfeed Med: Off J Acad Breastfeed Med. 2018;13:408–11.
Assad M, Elliott MJ, Abraham JH. Decreased cost and improved feeding tolerance in VLBW infants fed an exclusive human milk diet. J Perinatol. 2016;36:216–20.
O’Connor DL, Kiss A, Tomlinson C, Bando N, Bayliss A, Campbell DM, et al. Nutrient enrichment of human milk with human and bovine milk-based fortifiers for infants born weighing <1250 g: a randomized clinical trial. Am J Clin Nutr. 2018;108:108–16.
Bergner EM, Taylor SN, Gollins LA, Hair AB. Human milk fortification: a practical analysis of current evidence. Clin Perinatol. 2022;49:447–60.
Meredith-Dennis L, Xu G, Goonatilleke E, Lebrilla CB, Underwood MA, Smilowitz JT. Composition and variation of macronutrients, immune proteins, and human milk oligosaccharides in human milk from nonprofit and commercial milk banks. J Hum Lactation. 2018;34:120–9.
Ramey SR, Merlino Barr S, Moore KA, Groh-Wargo S. Exploring innovations in human milk analysis in the neonatal intensive care unit: a survey of the United States. Front Nutr. 2021;8:692600.
Meinzen-Derr J, Poindexter B, Wrage L, Morrow AL, Stoll B, Donovan EF. Role of human milk in extremely low birth weight infants’ risk of necrotizing enterocolitis or death. J Perinatol. 2009;29:57–62.
https://www.fda.gov/consumers/infant-formula-recall-what-know. Accessed 26 Feb 2022.
Hair AB, Hawthorne KM, Chetta KE, Abrams SA. Human milk feeding supports adequate growth in infants ≤1250 grams birth weight. BMC Res Notes. 2013;6:459.
Yee WH, Soraisham AS, Shah VS, Aziz K, Yoon W, Lee SK, et al. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics. 2012;129:e298–304.
Hampson G, Roberts SLE, Lucas A, Parkin D. An economic analysis of human milk supplementation for very low birth weight babies in the USA. BMC Pediatr. 2019;19:337.
Radmacher PG, Adamkin DH. Fortification of human milk for preterm infants. Semin Fetal Neonatal Med. 2017;22:30–35.
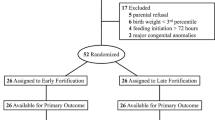
Thanigainathan S, Abiramalatha T. Early fortification of human milk versus late fortification to promote growth in preterm infants. Cochrane Database Syst Rev. 2020;7:CD013392.
Shah SD, Dereddy N, Jones TL, Dhanireddy R, Talati AJ. Early versus delayed human milk fortification in very low birth weight infants-a randomized controlled trial. J Pediatr. 2016;174:126–31.e121.
Godden B, Collins CT, Hilditch C, McLeod G, Keir A. Does early compared to late fortification of human milk for preterm infants improve clinical outcomes? J Paediatr Child Health. 2019;55:867–72.
Poindexter BB, Cormack BE, Bloomfield FH. Approaches to growth faltering. World Rev Nutr Diet. 2021;122:312–24.
Brennan AM, Kiely ME, Fenton S, Murphy BP. Standardized parenteral nutrition for the transition phase in preterm infants: a bag that fits. Nutrients. 2018;10:170.
Falciglia GH, Murthy K, Holl JL, Palac HL, Oumarbaeva Y, Woods DM, et al. Energy and protein intake during the transition from parenteral to enteral nutrition in infants of very low birth weight. J Pediatr. 2018;202:38–43.e31.
Miller M, Vaidya R, Rastogi D, Bhutada A, Rastogi S. From parenteral to enteral nutrition: a nutrition-based approach for evaluating postnatal growth failure in preterm infants. J Parenter Enter Nutr. 2014;38:489–97.
Parker MG, Greenberg LT, Edwards EM, Ehret D, Belfort MB, Horbar JD. National trends in the provision of human milk at hospital discharge among very low-birth-weight infants. JAMA Pediatr. 2019;173:961–8.
Groh-Wargo S, Thompson M. Managing the human-milk-fed, preterm, VLBW infant at NICU discharge: the sprinkles dilemma. Infant, Child, Adolesc Nutr. 2014;6:262–9.
Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). 2021 https://www.fns.usda.gov/wic/about-wic. Accessed 1 May 2022.
McCallie KR, Lee HC, Mayer O, Cohen RS, Hintz SR, Rhine WD. Improved outcomes with a standardized feeding protocol for very low birth weight infants. J Perinatol. 2011;31:S61–7.
Funding
BS is supported by Gerber Foundation grant #21-6234 and a grant from Evolve Biosystems. ABH and MG are supported by the National Institutes of Health (NIH) grant R01DK124614, and MG is also supported by NIH grants R01DK118568 and R01HD105301. None of the funding sources had any role in this manuscript.
Author information
Authors and Affiliations
Contributions
ABH, BS, and MG wrote the initial and final drafts of the manuscript, approved the final published version, and are accountable for all aspects of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hair, A.B., Scottoline, B. & Good, M. Dilemmas in human milk fortification. J Perinatol 43, 103–107 (2023). https://doi.org/10.1038/s41372-022-01502-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01502-6
This article is cited by
-
Supplementing human milk for preterm infants: a nutritional challenge?
Pediatric Research (2024)
-
Immediate fortification of human milk with a bovine milk-derived human milk fortifier in very low birth weight infants: a randomized clinical trial
Journal of Perinatology (2024)
-
Dilemmas in establishing preterm enteral feeding: where do we start and how fast do we go?
Journal of Perinatology (2023)