Abstract
Objective
To compare the frequency and severity of neonatal hypoglycemia in pregnancies treated with and without late preterm antenatal corticosteroids.
Study design
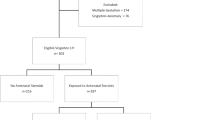
We conducted a retrospective cohort study of late preterm deliveries at LAC + USC (2015–2018). Neonatal outcomes were compared between pregnancies treated with and without corticosteroids.
Results
93 pregnancies (39.9%) received corticosteroids and 140 (60.1%) did not. Neonates born to women given corticosteroids were more likely to be hypoglycemic (47.3 vs. 29.3%, ORadj 2.25, padj = 0.01). The mean initial glucose (45.6 mg/dL vs. 51.9 mg/dL, p = 0.01) and glucose nadir (39.1 mg/dL vs. 45.4 mg/dL, p < 0.001) were significantly lower if the neonates received corticosteroids. Neonates admitted to the NICU solely for hypoglycemia were more likely to be born to women treated with corticosteroids (ORadj 4.71, padj = 0.01).
Conclusion
Administration of late preterm corticosteroids was associated with an increased incidence and severity of neonatal hypoglycemia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Gilstrap LC, Christensen R, Clewell WH, D'Alton ME, Davidson Jr EC, Escobedo MB, et al. Effect of corticosteroids for fetal maturation on perinatal outcomes. NIH consensus development panel on the effect of corticosteroids for fetal maturation on perinatal outcomes. JAMA 1995;273:413–18.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3:CD004454.
Escobar GJ, Clark RH, Greene JD. Short-term outcomes of infants born at 35 and 36 weeks gestation: we need to ask more questions. Semin Perinatol. 2006;30:28–33.
Gyamfi-Bannerman C, Thom EA, Blackwell SC, Tita AT, Reddy UM, Saade GR, et al. Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med. 2016;374:1311–20.
Committee on Obstetric Practice. Committee opinion no. 713: antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol. 2017;130:e102–9.
Society for Maternal-Fetal Medicine Publications Committee. Implementation of the use of antenatal corticosteroids in the late preterm birth period in women at risk for preterm delivery. Am J Obstet Gynecol. 2016;215:B13–5.
Papageorgiou AN, Desgranges MF, Masson M, Colle E, Shatz R, Gelfand MM. The antenatal use of betamethasone in the prevention of respiratory distress syndrome: a controlled double-blind study. Pediatrics. 1979;63:73–9.
Kamath-Rayne BD, DeFranco EA, Marcotte MP. Antenatal steroids for treatment of fetal lung immaturity after 34 weeks of gestation: an evaluation of neonatal outcomes. Obstet Gynecol. 2012;119:909–16.
Ramadan MK, Hussein G, Saheb W, Rajab M, Mirza FG. Antenatal corticosteroids in the late preterm period: a prospective cohort study. J Neonatal Perinat Med. 2016;9:15–22.
Sifianou P, Thanou V, Karga H. Metabolic and hormonal effects of antenatal betamethasone after 35 weeks of gestation. J Pediatr Pharm Ther. 2015;20:138–43.
Committee on Fetus and Newborn, Adamkin DH. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics. 2011;127:575–57911.
Harris DL, Weston PJ, Harding JE. Incidence of neonatal hypoglycemia in babies identified as at risk. J Pediatr. 2012;161:787–91.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81.
Shah R, Harding J, Brown J, McKinlay C. Neonatal glycaemia and neurodevelopmental outcomes: a systematic review and meta-analysis. Neonatology. 2019;115:116–26.
Kugelman A, Colin AA. Late preterm infants: near term but still in a critical developmental time period. Pediatrics. 2013;132:741–51.
Funding
EC was the recipient of the 2017 Keck School of Medicine Summer Research Fellowship Award to support her work on the conduct of this research.
Author information
Authors and Affiliations
Contributions
KRU designed the study, acquired data, and was the primary author of the Institutional Review Board proposal and manuscript. RHL helped design the study, write the Institutional Review Board proposal, interpret the data, and edit the manuscript. SS helped design the study, write the Institutional Review Board proposal, interpret the data, and edit the manuscript. EC acquired data and helped write the manuscript. UI performed the statistical analysis and helped write the manuscript. VKC developed the statistical analysis plan, oversaw statistical analysis, and helped write the manuscript. LB helped design the study, write the Institutional Review Board proposal, interpret the data, and edit the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Uquillas, K.R., Lee, R.H., Sardesai, S. et al. Neonatal hypoglycemia after initiation of late preterm antenatal corticosteroids. J Perinatol 40, 1339–1348 (2020). https://doi.org/10.1038/s41372-020-0589-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0589-1
This article is cited by
-
Late preterm antenatal steroid use and infant outcomes in a single center
Journal of Perinatology (2024)
-
Late preterm antenatal corticosteroids in singleton and twin gestations: a retrospective cohort study
BMC Pregnancy and Childbirth (2022)
-
Antenatal dexamethasone use and respiratory distress in late preterm infants: results from first Vietnamese matched cohort study
BMC Pregnancy and Childbirth (2021)
-
Respiratory and glycemic control outcomes of late preterm infants after antenatal corticosteroid exposure
Journal of Perinatology (2021)