Abstract
Objective
Evaluate racial/ethnic differences in maternal resilience and its associations with low birthweight (LBW).
Study design
Retrospective cohort study of 3244 women surveyed in the Longitudinal Study of Adolescent to Adult Health. The Add Health Resilience Instrument assessed resilience. Logistic regression models explored associations between women’s resilience and risk of LBW.
Result
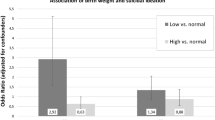
Resilience scores were lowest in American Indian women. Women with the lowest resilience scores were more likely to deliver a LBW infant than highly resilient women, after adjusting for demographic and health-related factors (aOR 1.58 95% CI 1.05–2.38). The risk-adjusted rate of LBW among highly resilient Black women (15.6%) was significantly higher than the risk-adjusted rate of LBW among highly resilient white women (9.1%, p = 0.01) and highly resilient Hispanic women (8.6%, p = 0.04).
Conclusion
Resilience scores differ significantly among women of different race and ethnicity but do not appear to entirely account for racial/ethnic disparities in LBW.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
This study utilized both the public use and restricted-use data provided by the original Add Health investigative team. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth).
Code availability
We used STATA version 15 (StataCorp LLC, College Station, TX) for all analyses. The codes used for the analyses in this paper are available upon request.
References
Hughes MM, Black RE, Katz J. 2500-g low birth weight cutoff: history and implications for future research and policy. Matern Child Health J. 2017;21:283–9.
Visentin S, Grumolato F, Nardelli GB, Di Camillo B, Grisan E, Cosmi E. Early origins of adult disease: low birth weight and vascular remodeling. Atherosclerosis. 2014;237:391–9.
Boeri L, Ventimiglia E, Capogrosso P, Ippolito S, Pecoraro A, Paciotti M, et al. Low birth weight is associated with a decreased overall adult health status and reproductive capability—results of a cross-sectional study in primary infertile patients. PLoS ONE. 2016;11:e0166728.
Hovi P, Andersson S, Eriksson JG, Järvenpää A-L, Strang-Karlsson S, Mäkitie O, et al. Glucose regulation in young adults with very low birth weight. N Engl J Med. 2007;356:2053–63.
Institute of Medicine (US) Committee on Improving Birth Outcomes, Bale JR, Stoll BJ, Lucas AO. Improving birth outcomes: meeting the challenge in the developing world. Washington DC: National Academies Press (US); 2003.
Hamilton BE, Martin JA, Osterman MJK, Rossen LM. Births: provisional data for 2018. Vital Statistics Rapid Release; no 7. Hyattsville, MD: National Center for Health Statistics; May 2019.
Burris HH, Hacker MR. Birth outcome racial disparities: a result of intersecting social and environmental factors. Semin Perinatol. 2017;41:360–6.
Lorch SA, Enlow E. The role of social determinants in explaining racial/ethnic disparities in perinatal outcomes. Pediatr Res. 2015;79:141–7.
McDonald SW, Kingston D, Bayrampour H, Dolan SM, Tough SC. Cumulative psychosocial stress, coping resources, and preterm birth. Arch Womens Ment Health. 2014;17:559–68.
Wainstock T, Anteby E, Glasser S, Shoham-Vardi I, Lerner-Geva L. The association between prenatal maternal objective stress, perceived stress, preterm birth and low birthweight. J Matern Fetal Neonatal Med. 2013;26:973–7. https://doi.org/10.3109/14767058.2013.766696.
Grobman WA, Parker C, Wadhwa PD, Willinger M, Simhan H, Silver B, et al. Racial/ethnic disparities in measures of self-reported psychosocial states and traits during pregnancy. Am J Perinatol. 2016;33:1426–32.
Rosenthal L, Lobel M. Explaining racial disparities in adverse birth outcomes: unique sources of stress for Black American women. Soc Sci Med. 2011;72:977–83.
Olson DM, Severson EM, Verstraeten BSE, Ng JWY, McCreary JK, Metz GAS. Allostatic load and preterm birth. Int J Mol Sci. 2015;16:29856–74.
Hux VJ, Catov JM, Roberts JM. Allostatic load in women with a history of low birth weight infants: the national health and nutrition examination survey. J Womens Health. 2014;23:1039–45.
Solivan AE, Wallace ME, Kaplan KC, Harville EW. Use of a resiliency framework to examine pregnancy and birth outcomes among adolescents: a qualitative study. Fam Syst Health. 2015;33:349–55.
Bhatia N, Chao SM, Higgins C, Patel S, Crespi CM. Association of mothers’ perception of neighborhood quality and maternal resilience with risk of preterm birth. Int J Environ Res Public Health. 2015;12:9427–43.
Lobel M, DeVincent CJ, Kaminer A, Meyer BA. The impact of prenatal maternal stress and optimistic disposition on birth outcomes in medically high-risk women. Health Psychol. 2000;19:544–53.
Grobman WA, Parker CB, Willinger M, Wing DA, Silver RM, Wapner RJ, et al. Racial disparities in adverse pregnancy outcomes and psychosocial stress. Obstet Gynecol. 2018;131:328–35.
Harris KM, Halpern CT, Whitsel E, Hussey J, Tabor J, Entzel P, et al. The National Longitudinal Study of Adolescent to Adult Health: research design. 2009. http://www.cpc.unc.edu/projects/addhealth/design.
Montoya-Williams D, Passarella M, Lorch SA. Retrospective development of a novel resilience scale using existing cohort data: the adolescent to adult health resilience instrument. Under review.
Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health Qual Life Outcomes. 2011;9:8.
Blanco V, Guisande MA, Sánchez MT, Otero P, Vázquez FL. Spanish validation of the 10-item Connor-Davidson Resilience Scale (CD-RISC 10) with non-professional caregivers. Aging Ment Health. 2017;23:1–6.
Green KT, Hayward LC, Williams AM, Dennis PA, Bryan BC, Taber KH, et al. Examining the factor structure of the Connor-Davidson Resilience Scale (CD-RISC) in a post-9/11 U.S. military veteran sample. Assessment. 2014;21:443–51.
Notario-Pacheco B, Solera-Martínez M, Serrano-Parra MD, Bartolomé-Gutiérrez R, García- Campayo J, Martínez-Vizcaíno V. Reliability and validity of the Spanish version of the 10-item Connor-Davidson Resilience Scale (10-item CD-RISC) in young adults. Health Qual Life Outcomes. 2011;9:63.
Chen P, Chantala K. Guidelines for analyzing add health data. Carolina Digit Repos. 2014. https://doi.org/10.17615/C6BW8W.
Oliveira ACP de Miss, Machado APG Mr, Aranha RN Miss. Identification of factors associated with resilience in medical students through a cross-sectional census. BMJ Open. 2017;7:e017189.
Wu Z, Liu Y, Li X, Li X. Resilience and associated factors among mainland Chinese women newly diagnosed with breast cancer. PLoS ONE. 2016;11:e0167976.
Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43:962–70.
Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Osterman MJK. Births: final data for 2008. Natl Vital Stat Rep. 2010;59:1–72.
Rutter M. Resilience as a dynamic concept. Dev Psychopathol. 2012;24:335–44.
Lee ACC, Katz J, Blencowe H, Cousens S, Kozuki N, Vogel JP, et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle- income countries in 2010. Lancet Glob Health. 2013;1:e26–36.
Hogue CJR, Bremner JD. Stress model for research into preterm delivery among black women. Am J Obstet Gynecol. 2005;192 Suppl 5:S47–55.
Borders AEB, Wolfe K, Qadir S, Kim K-Y, Holl J, Grobman W. Racial/ethnic differences in self- reported and biologic measures of chronic stress in pregnancy. J Perinatol. 2015;35:580–4.
Boyd RW, Lindo EG, Weeks LD, Lemore MR. On racism: a new standard for publishing on racial health inequities. Health Aff Blog. 2020. https://www.healthaffairs.org/do/10.1377/hblog20200630.939347/full/.
Vyas DA, Eisenstein LG, Jones DS. Hidden in plain sight—reconsidering the use of race correction in clinical algorithms. N Engl J Med. 2020. https://doi.org/10.1056/NEJMms2004740.
Ashok S. The rise of the American “Others.” The Atlantic. 2016. https://www.theatlantic.com/politics/archive/2016/08/the-rise-of-the-others/497690/.
Helmreich I, Kunzler A, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions for resilience enhancement in adults. Cochrane Database Syst Rev. 2017. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6464102/.
Liauw J, Jacobsen GW, Larose TL, Hutcheon JA. Short interpregnancy interval and poor fetal growth: evaluating the role of pregnancy intention. Paediatr Perinat Epidemiol. 2019;33:O73–85.
Acknowledgements
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. No direct support was received from grant P01-HD31921 for this study, however we would like to acknowledge the Division of Neonatology at the Children’s Hospital of Philadelphia for administrative support and Ms. Ali Chandler for her assistance in preparing this paper.
Funding
This research uses data from Add Health, which was originally funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. The authors of this paper received no additional funding to complete this study.
Author information
Authors and Affiliations
Contributions
Using their own language, all authors whose names appear on the submission: (1) made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; (2) drafted the work or revised it critically for important intellectual content; (3) approved the version to be published; and (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was deemed exempt by the local Institutional Review Board as it uses de-identified, publicly available data. This study was performed in accordance with the Declarations of Helsinki.
Informed consent
All original participants provided written, informed consent to participate. The written consent informed participants that results, in aggregate, would be published.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Montoya-Williams, D., Passarella, M., Grobman, W.A. et al. Racial/ethnic differences in maternal resilience and associations with low birthweight. J Perinatol 41, 196–203 (2021). https://doi.org/10.1038/s41372-020-00837-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00837-2
This article is cited by
-
Critical disparities in perinatal health—understanding risks and changing the outcomes
Journal of Perinatology (2021)